Saxenda rebound weight gain is a common concern for patients discontinuing liraglutide treatment for weight management. After stopping Saxenda, many individuals experience a return of appetite and gradual weight regain as the medication's appetite-suppressing effects diminish. This phenomenon reflects the chronic nature of obesity and the body's metabolic adaptations to weight loss, including hormonal changes that promote hunger and reduce energy expenditure. Understanding why rebound weight gain occurs and implementing strategies to minimise it—such as sustained lifestyle modifications, behavioural support, and ongoing medical follow-up—are essential for long-term success. This article explores the mechanisms behind Saxenda rebound weight gain and evidence-based approaches to maintain weight loss after treatment cessation.
Summary: Saxenda rebound weight gain occurs because stopping liraglutide reverses its appetite-suppressing effects, leading to increased hunger and gradual weight regain in many patients.
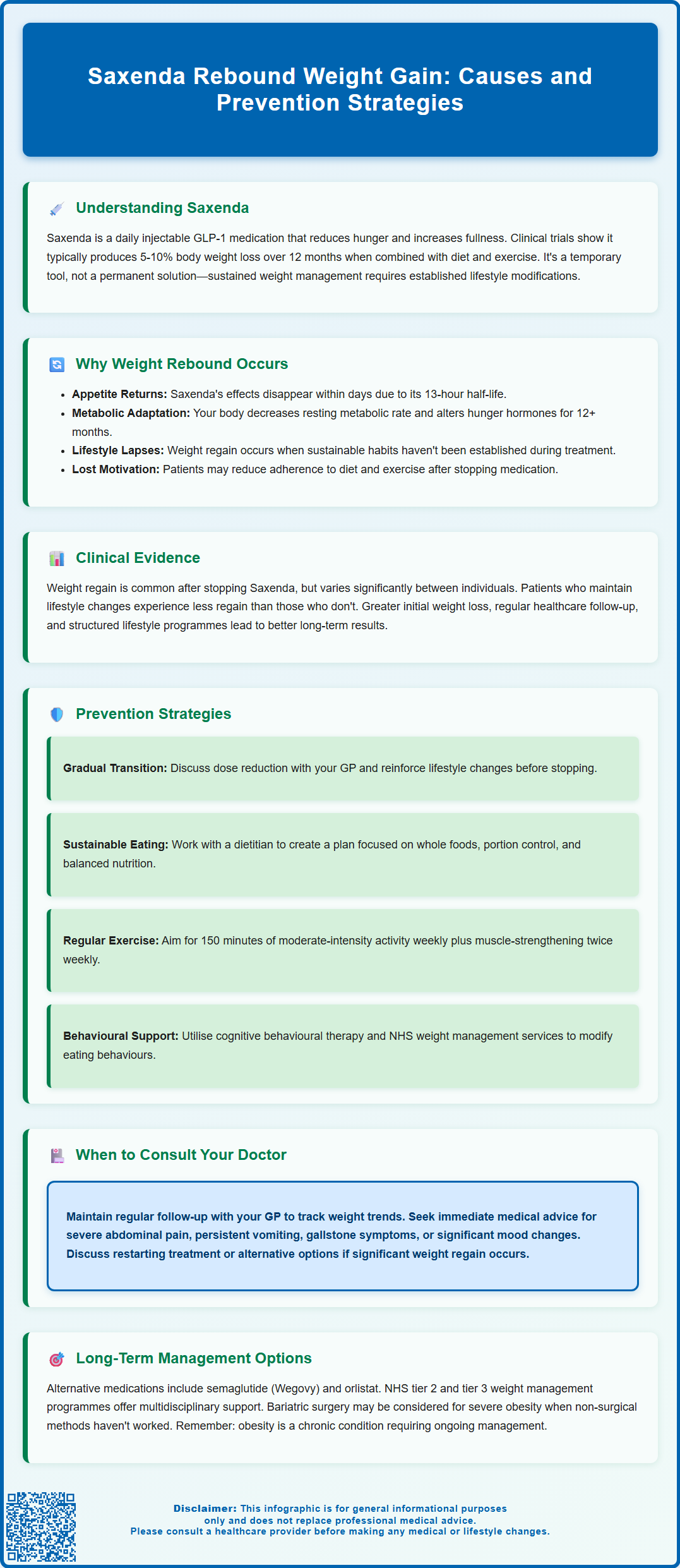
- Liraglutide (Saxenda) is a GLP-1 receptor agonist that reduces appetite by acting on brain receptors; its effects diminish within days of stopping treatment due to its 13-hour half-life.
- Weight regain after Saxenda cessation is driven by metabolic adaptations including increased hunger hormones (ghrelin), decreased satiety hormones (leptin), and reduced resting metabolic rate.
- Clinical trials show varying degrees of weight regain after stopping Saxenda, with better outcomes in patients who maintain lifestyle modifications and regular healthcare follow-up.
- Strategies to minimise rebound weight gain include establishing sustainable dietary habits, achieving at least 150 minutes of weekly physical activity, and accessing NHS tier 2 or tier 3 weight management services.
- Alternative treatments such as semaglutide (Wegovy) or orlistat may be considered if significant weight regain occurs, subject to NICE guidance and local NHS commissioning decisions.
Table of Contents
- Understanding Saxenda and Weight Regain After Stopping Treatment
- Why Does Weight Rebound Occur After Discontinuing Saxenda?
- Clinical Evidence on Weight Regain Following Saxenda Cessation
- Strategies to Minimise Weight Rebound After Stopping Saxenda
- Long-Term Weight Management: Alternatives and Maintenance Approaches
- Frequently Asked Questions
Understanding Saxenda and Weight Regain After Stopping Treatment
Saxenda (liraglutide 3.0 mg) is a once-daily injectable medication licensed by the MHRA for weight management in adults with a body mass index (BMI) of 30 kg/m² or above, or 27 kg/m² or above with weight-related comorbidities such as type 2 diabetes, hypertension, dyslipidaemia or obstructive sleep apnoea. As a glucagon-like peptide-1 (GLP-1) receptor agonist, Saxenda works by mimicking the action of the naturally occurring hormone GLP-1, which regulates appetite and food intake.
The medication acts on specific receptors in the brain's appetite centres, particularly in the hypothalamus, to reduce hunger and increase feelings of fullness. This mechanism helps patients consume fewer calories whilst maintaining better control over eating behaviours. Clinical trials have demonstrated that Saxenda, when combined with a reduced-calorie diet and increased physical activity, can lead to clinically significant weight loss—typically 5–10% of initial body weight over 12 months, as shown in the SCALE (Satiety and Clinical Adiposity—Liraglutide Evidence) trials.
However, a common concern amongst patients and healthcare professionals is the phenomenon of weight regain after discontinuing Saxenda. This rebound effect is not unique to liraglutide but is observed across many pharmacological weight management interventions. Understanding why this occurs and how to mitigate it is essential for setting realistic expectations and developing sustainable long-term weight management strategies.
It is important to recognise that Saxenda is not a permanent solution but rather a tool to facilitate weight loss during a critical period. According to the Saxenda SmPC, treatment should be discontinued after 12 weeks on the 3.0 mg daily dose if patients have not lost at least 5% of their initial body weight. Treatment should be initiated and monitored by healthcare professionals experienced in weight management and obesity-related comorbidities. Saxenda should not be used in combination with other GLP-1 receptor agonists.
The medication does not cure obesity or alter the underlying metabolic and behavioural factors that contribute to weight gain. Consequently, when treatment is stopped, patients may experience a return of appetite and gradual weight regain unless appropriate lifestyle modifications and maintenance strategies are firmly established.
Why Does Weight Rebound Occur After Discontinuing Saxenda?
Weight regain following Saxenda cessation is primarily driven by the reversal of the medication's pharmacological effects on appetite regulation. Liraglutide has a half-life of approximately 13 hours, as stated in the Saxenda SmPC, meaning that within days of stopping treatment, circulating levels of the drug decline significantly. As GLP-1 receptor stimulation diminishes, the appetite-suppressing effects wane, and patients often experience a return of hunger signals to pre-treatment levels.
This phenomenon is partly explained by the body's metabolic adaptation to weight loss. During periods of caloric restriction and weight reduction, the body undergoes physiological changes designed to defend against further weight loss—a survival mechanism rooted in evolutionary biology. These adaptations include decreased resting metabolic rate, increased hunger hormones (such as ghrelin), and reduced levels of satiety hormones (such as leptin). Research by Sumithran et al. (NEJM 2011) has demonstrated that these hormonal changes can persist for 12 months or longer after weight loss, creating an environment conducive to weight regain when Saxenda is discontinued.
Additionally, many patients may not have fully established the behavioural and lifestyle changes necessary for long-term weight maintenance during their treatment period. Saxenda can facilitate weight loss by reducing appetite, but if patients have not developed sustainable eating patterns, regular physical activity habits, and psychological coping strategies, they are more vulnerable to reverting to previous behaviours once the medication is stopped.
There is also a psychological component to consider. Some patients may experience a sense of loss or reduced motivation after stopping treatment, particularly if they perceive the medication as the primary driver of their success. This can lead to decreased adherence to dietary and exercise recommendations, further contributing to weight regain. Understanding these multifactorial causes is crucial for developing effective strategies to minimise rebound weight gain.
Clinical Evidence on Weight Regain Following Saxenda Cessation
Clinical trial data demonstrate that weight regain commonly occurs after discontinuing Saxenda. In the SCALE (Satiety and Clinical Adiposity—Liraglutide Evidence) trials, which formed the basis for Saxenda's regulatory approval, participants who stopped liraglutide treatment experienced gradual weight regain over the following months. The extent and rate of weight regain varied considerably between individuals.
The SCALE Maintenance trial examined weight trajectories after treatment cessation. Participants who had initially lost weight with liraglutide and then stopped the medication showed varying degrees of weight regain, with those who maintained lifestyle modifications experiencing less weight regain compared to those who did not sustain these behaviours.
Observational studies indicate that many patients regain a proportion of lost weight within the first year after stopping Saxenda, with regain rates varying based on factors such as initial weight loss achieved, duration of treatment, and adherence to lifestyle interventions. The pattern and extent of weight regain appear to be influenced by multiple factors, including biological, behavioural, and environmental considerations.
It is worth noting that not all patients experience significant rebound weight gain. Those who achieve greater initial weight loss, maintain regular follow-up with healthcare professionals, and continue structured lifestyle programmes tend to have better long-term outcomes. These findings underscore the importance of viewing Saxenda as part of a comprehensive weight management strategy rather than a standalone solution.
While individual responses vary considerably, research suggests that without continued lifestyle intervention, many patients will experience some degree of weight regain after discontinuing pharmacological treatment for obesity. This highlights the chronic nature of obesity and the need for ongoing management strategies.
Strategies to Minimise Weight Rebound After Stopping Saxenda
Some clinicians may consider gradual dose reduction rather than abrupt cessation when stopping Saxenda, though this approach is not included in the SmPC and there is limited formal evidence to support it. Any tapering should only be done under healthcare professional supervision. Discussing your treatment plan with your GP or specialist can allow time to reinforce lifestyle changes and adjust to the return of appetite signals. This approach may also help identify patients who might benefit from continued treatment or alternative pharmacological support.
Establishing robust dietary habits during Saxenda treatment is crucial for long-term success. Working with a registered dietitian to develop a sustainable eating plan that emphasises whole foods, appropriate portion sizes, and balanced macronutrients can provide a foundation for weight maintenance. Strategies such as meal planning, mindful eating, and keeping a food diary have been shown to support continued weight management after medication cessation.
Regular physical activity is one of the strongest predictors of successful weight maintenance. The UK Chief Medical Officers' guidelines, endorsed by the NHS, recommend at least 150 minutes of moderate-intensity aerobic activity per week, along with muscle-strengthening exercises on two or more days. Building physical activity into daily routines—such as walking, cycling, or swimming—can help offset the metabolic adaptations that promote weight regain. Importantly, exercise should be enjoyable and sustainable rather than punitive.
Behavioural support and psychological interventions play a vital role in preventing rebound weight gain. Cognitive behavioural therapy (CBT) techniques can help patients identify and modify unhelpful thoughts and behaviours related to eating and weight. Your GP can refer you to NHS tier 2 or tier 3 weight management services that offer group or individual support programmes that continue after medication is stopped. Regular self-monitoring of weight, food intake, and physical activity can also enhance accountability and early detection of weight regain.
Finally, ongoing medical follow-up is essential. Patients should maintain regular contact with their GP or weight management service to monitor weight trends, address any concerns, and adjust management strategies as needed. If weight regain occurs despite lifestyle efforts, discussing the possibility of restarting treatment (subject to the SmPC criteria) or considering alternative treatments may be appropriate.
Long-Term Weight Management: Alternatives and Maintenance Approaches
For patients who experience significant weight regain after stopping Saxenda, several alternative pharmacological options may be considered. Other GLP-1 receptor agonists, such as semaglutide (marketed as Wegovy for weight management), offer similar mechanisms of action. Wegovy is recommended by NICE (TA875) for adults with a BMI of at least 35 kg/m² (or at least 30 kg/m² with weight-related comorbidities) and is available through specialist NHS weight management services. Orlistat, which works by reducing fat absorption in the gut, represents a different pharmacological approach and may be suitable for some patients.
NICE guidance recommends that pharmacological interventions for obesity should only be continued if patients achieve and maintain clinically beneficial weight loss (typically ≥5% of initial body weight). If Saxenda or alternative medications are considered, they should be combined with comprehensive lifestyle interventions and regular monitoring. It is important to recognise that long-term or intermittent pharmacological treatment may be necessary for some individuals, as obesity is a chronic relapsing condition rather than an acute illness. Availability and funding for weight management medications on the NHS varies locally.
Structured weight management programmes provide valuable support for long-term maintenance. NHS-commissioned services, such as tier 2 and tier 3 weight management programmes, offer multidisciplinary input including dietary advice, physical activity support, and psychological interventions. Your GP can refer you to these services. Commercial programmes with evidence of effectiveness, such as Weight Watchers (WW) or Slimming World, may also be beneficial for some patients. The key is finding an approach that is sustainable and aligns with individual preferences and circumstances.
For patients with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) who have not achieved adequate weight loss with non-surgical interventions, bariatric surgery may be considered. NICE recommends that bariatric surgery should be offered as part of a comprehensive care pathway with long-term follow-up. Expedited assessment for bariatric surgery may be appropriate for people with recent-onset type 2 diabetes and a BMI of 35 kg/m² or more.
Patient safety considerations are paramount throughout the weight management journey. Patients should contact their GP if they experience concerning weight regain, worsening of obesity-related comorbidities, or psychological distress related to weight changes. If you have used Saxenda and experience severe abdominal pain, persistent vomiting, symptoms of gallstones, or significant mood changes, seek medical advice promptly. Suspected side effects can be reported via the MHRA Yellow Card scheme. Regular monitoring of blood pressure, blood glucose, and lipid profiles is important, particularly for those with pre-existing cardiovascular or metabolic conditions. Ultimately, successful long-term weight management requires a personalised, compassionate approach that addresses the biological, psychological, and social factors contributing to obesity.
Frequently Asked Questions
How quickly does weight regain occur after stopping Saxenda?
Weight regain typically begins within weeks to months after stopping Saxenda as the medication's appetite-suppressing effects diminish. The rate and extent of weight regain vary considerably between individuals, with those maintaining lifestyle modifications experiencing less regain than those who do not sustain dietary and physical activity changes.
Can I restart Saxenda if I regain weight after stopping treatment?
Restarting Saxenda may be considered if you meet the prescribing criteria (BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidities) and have regained weight despite lifestyle efforts. This decision should be made in consultation with your GP or weight management specialist, who will assess your individual circumstances and ensure appropriate monitoring.
What NHS services can help prevent weight regain after stopping Saxenda?
Your GP can refer you to NHS tier 2 or tier 3 weight management services, which provide multidisciplinary support including dietary advice, physical activity programmes, and behavioural interventions. These structured programmes offer ongoing support to help maintain weight loss after medication cessation, though availability varies by local commissioning.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript