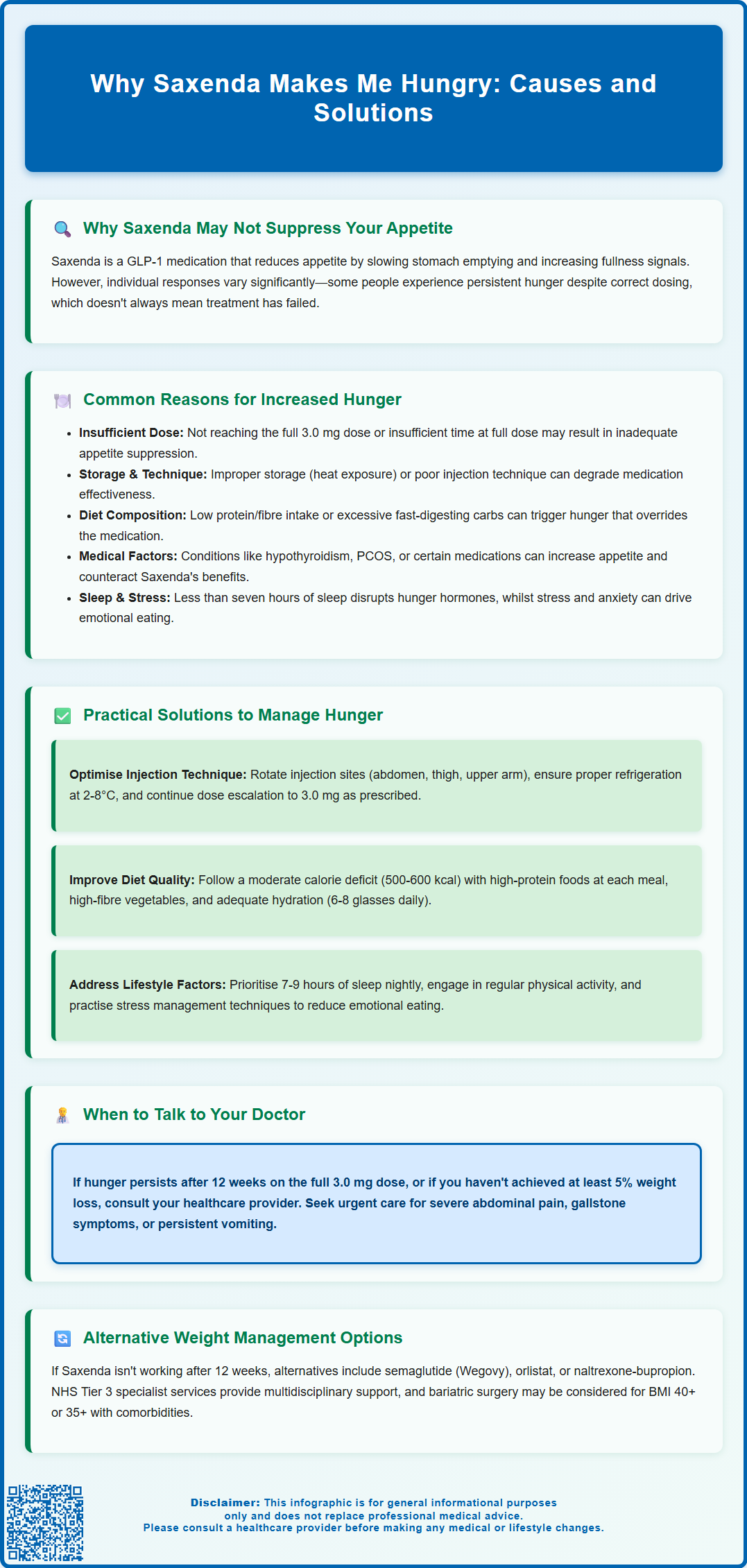
Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed for weight management that works by suppressing appetite and slowing gastric emptying. However, some patients report that Saxenda makes them feel hungry despite adherence to treatment, which can be distressing and undermine confidence in therapy. This paradoxical response may result from inadequate dosing, incorrect injection technique, dietary factors, underlying medical conditions, or lifestyle influences such as poor sleep. Understanding why appetite suppression may not occur as expected is essential for optimising treatment outcomes. If you experience persistent hunger on Saxenda, discuss this with your prescribing clinician rather than stopping treatment independently, as adjustments or alternative strategies may restore effectiveness.
Summary: Saxenda may fail to suppress appetite or cause increased hunger due to insufficient dosing, incorrect injection technique, medication storage issues, dietary composition, psychological factors, underlying medical conditions, or inadequate sleep.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist that suppresses appetite by slowing gastric emptying and enhancing satiety signals to the brain.
- Individual responses vary considerably; some patients require the full 3.0 mg maintenance dose for several weeks before experiencing appetite suppression.
- Incorrect injection technique, improper medication storage (must be refrigerated 2-8°C before first use), or failure to rotate injection sites can compromise drug efficacy.
- Dietary factors such as low protein or fibre intake, severe calorie restriction, inadequate sleep, stress, and certain medications can trigger hunger independently of GLP-1 receptor activation.
- NICE guidance recommends reassessing treatment after 12 weeks on the maintenance dose and discontinuing if weight loss of at least 5% has not been achieved.
- Persistent hunger despite optimised dosing and lifestyle measures warrants clinical review to consider alternative GLP-1 agonists, other pharmacotherapy, specialist weight management services, or bariatric surgery.
Table of Contents
Why Saxenda May Not Suppress Your Appetite as Expected
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with weight-related comorbidities. The medication works by mimicking the action of the naturally occurring hormone GLP-1, which regulates appetite by slowing gastric emptying, enhancing satiety signals to the brain, and reducing hunger between meals. Clinical trials show that many people notice appetite reduction within weeks, but responses vary considerably.
However, individual responses to Saxenda vary considerably, and some patients report persistent or even increased hunger despite adherence to the prescribed dose escalation schedule. This paradoxical response can be distressing and may undermine confidence in the treatment. It is important to recognise that appetite regulation is a complex physiological process influenced by multiple factors beyond GLP-1 receptor activation, including hormonal balance, metabolic rate, psychological state, sleep quality, and dietary composition.
The absence of expected appetite suppression does not necessarily indicate treatment failure, but it does warrant careful evaluation. Understanding why Saxenda may not be working as anticipated requires consideration of both pharmacological factors—such as dose adequacy, injection technique, and medication storage—and lifestyle factors that can influence hunger signals. According to NICE guidance, treatment should be reassessed after 12 weeks on the maintenance dose of 3.0 mg, and discontinued if weight loss of at least 5% has not been achieved. If you are experiencing persistent hunger on Saxenda, it is essential to discuss this with your prescribing clinician rather than discontinuing treatment independently, as adjustments or alternative strategies may restore the medication's effectiveness.
Common Reasons Saxenda Makes You Feel Hungry
Several factors may explain why Saxenda fails to suppress appetite or appears to increase hunger in some individuals. Insufficient dose escalation is a frequent cause; Saxenda requires gradual titration from 0.6 mg daily up to the maintenance dose of 3.0 mg daily over five weeks. Patients who remain on lower doses may not achieve adequate GLP-1 receptor activation for appetite suppression. Conversely, some individuals may require the full maintenance dose for several weeks before noticing significant effects on hunger.
Incorrect injection technique or medication storage can compromise drug efficacy. Saxenda must be stored in a refrigerator (2-8°C) before first use and can then be kept at room temperature (below 30°C) or refrigerated for up to one month. Protect from heat and light, and do not freeze. Remove the needle after each injection. Exposure to excessive heat or freezing temperatures degrades liraglutide, rendering it less effective. Additionally, injecting into areas with potentially reduced absorption, or failing to rotate injection sites may result in inconsistent drug delivery.
Dietary composition significantly influences hunger perception while taking Saxenda. Diets excessively low in protein or fibre, or those high in rapidly digested carbohydrates, can trigger rebound hunger despite GLP-1 receptor agonism. Similarly, severe calorie restriction may activate compensatory hunger mechanisms that override the medication's appetite-suppressing effects. Psychological factors, including stress, anxiety, depression, and emotional eating patterns, can also drive hunger independently of physiological satiety signals.
Underlying medical conditions such as hypothyroidism, polycystic ovary syndrome (PCOS), or insulin resistance may contribute to hunger and weight gain. These conditions warrant clinical assessment and management alongside Saxenda treatment. Certain medications, including corticosteroids and some antipsychotics, can increase appetite and potentially counteract liraglutide's effects. Finally, inadequate sleep (less than seven hours per night) disrupts appetite-regulating hormones like leptin and ghrelin, potentially overwhelming Saxenda's appetite suppression. Increased appetite is not listed as an adverse reaction in the UK SmPC for Saxenda; if you suspect this as a reaction to the medication, discuss it with your healthcare provider.
How to Manage Increased Hunger While Taking Saxenda
If you are experiencing persistent hunger while taking Saxenda, several evidence-based strategies may help optimise treatment outcomes. First, verify your injection technique and medication storage with your prescribing clinician or practice nurse. Ensure you are rotating injection sites between the abdomen, thigh, and upper arm, and that the medication has been stored correctly. If you have not yet reached the 3.0 mg maintenance dose, continue the prescribed escalation schedule, as appetite suppression often improves at higher doses.
Dietary modification is crucial for managing hunger on Saxenda. NICE guidance emphasises that liraglutide should be used alongside a reduced-calorie diet (typically 500–600 kcal deficit) rather than severe restriction, which can trigger compensatory hunger. Focus on:
-
High-protein foods (lean meat, fish, eggs, legumes, Greek yoghurt) at each meal to enhance satiety
-
High-fibre vegetables and whole grains to slow digestion and prolong fullness
-
Adequate hydration (6-8 glasses of fluid daily, approximately 1.2 litres, more during hot weather or exercise), as thirst is often mistaken for hunger
-
Regular meal timing (three balanced meals with planned snacks if needed) to stabilise blood glucose and prevent extreme hunger
-
Minimising ultra-processed foods and refined sugars that cause rapid blood glucose fluctuations
Addressing lifestyle factors can significantly improve appetite regulation. Prioritise seven to nine hours of quality sleep per night, as sleep deprivation increases ghrelin (hunger hormone) and decreases leptin (satiety hormone). Incorporate regular physical activity, which helps regulate appetite hormones and improves insulin sensitivity. Stress management techniques—such as mindfulness, cognitive behavioural therapy (CBT), or relaxation exercises—may reduce emotional eating patterns.
Keep a detailed symptom diary documenting hunger levels, meal timing, food choices, sleep quality, and stress levels. This information helps your clinician identify patterns and adjust your treatment plan accordingly. If hunger persists despite these measures after 12 weeks on the full maintenance dose, contact your GP or prescribing specialist to discuss whether Saxenda is the appropriate treatment for you. Do not stop or change the dose without clinical advice.
Seek urgent medical attention if you experience severe, persistent abdominal pain (with or without vomiting), signs of gallstones, or persistent vomiting/dehydration. Stop Saxenda and contact your prescriber immediately if you become pregnant or are breastfeeding.
Alternative Weight Management Options if Saxenda Isn't Working
If Saxenda fails to produce adequate appetite suppression or weight loss after 12 weeks at the maintenance dose (defined by NICE as less than 5% body weight loss), your clinician should review your treatment plan and consider alternative approaches. Other GLP-1 receptor agonists may be more effective for some individuals; semaglutide (Wegovy), administered as a once-weekly injection, has demonstrated superior weight loss outcomes in clinical trials compared to liraglutide. Wegovy is recommended by NICE (TA875) for use in specialist services, subject to availability and specific eligibility criteria.
Alternative pharmacotherapy represents another option. Orlistat, a lipase inhibitor that reduces dietary fat absorption, works through a different mechanism and may be prescribed alongside lifestyle interventions. Treatment should be reviewed after 12 weeks and continued only if at least 5% weight loss has been achieved. Naltrexone-bupropion (Mysimba), which acts on central appetite regulation pathways, is licensed for weight management in the UK and requires review after 16 weeks (with a 5% weight loss threshold). Your prescribing clinician will assess your medical history, contraindications, and individual circumstances to determine the most appropriate alternative.
Specialist weight management services offer multidisciplinary support, including dietetic input, psychological therapy, and structured exercise programmes. NHS Tier 3 weight management services provide intensive behavioural interventions that address the complex factors contributing to obesity. Referral criteria vary by region, but your GP can facilitate access to these services.
Bariatric surgery may be considered for individuals with a BMI of 40 kg/m² or greater, or 35 kg/m² or greater with significant comorbidities (such as type 2 diabetes or obstructive sleep apnoea), particularly if non-surgical interventions have been unsuccessful. NICE also recommends considering surgery at a lower BMI threshold (30-34.9 kg/m²) for people with recent-onset type 2 diabetes. Procedures such as gastric bypass or sleeve gastrectomy have demonstrated substantial, sustained weight loss and metabolic benefits.
Regardless of the approach, ongoing lifestyle modification remains fundamental to successful weight management. Engage with registered dietitians, consider cognitive behavioural therapy for eating behaviours, and maintain regular physical activity. Weight management is a long-term commitment, and finding the right combination of interventions may require patience and persistence. Always discuss treatment changes with your healthcare team to ensure safe, evidence-based care tailored to your individual needs.
If you experience any suspected adverse reactions to Saxenda or other medications, report them through the MHRA Yellow Card scheme.
Frequently Asked Questions
Why does Saxenda make me feel hungry instead of suppressing my appetite?
Saxenda may fail to suppress appetite due to insufficient dosing (not yet at the 3.0 mg maintenance dose), incorrect injection technique, improper medication storage, dietary factors such as low protein or fibre intake, psychological stress, inadequate sleep, or underlying medical conditions like hypothyroidism or PCOS. Discuss persistent hunger with your prescribing clinician to identify the cause and optimise treatment.
How long does it take for Saxenda to reduce hunger?
Many patients notice appetite reduction within weeks of starting Saxenda, but individual responses vary considerably. Some people require the full 3.0 mg maintenance dose for several weeks before experiencing significant appetite suppression, as the medication is gradually escalated over five weeks from 0.6 mg daily.
What should I do if Saxenda isn't controlling my hunger after 12 weeks?
If hunger persists after 12 weeks on the full 3.0 mg maintenance dose and you have not achieved at least 5% weight loss, contact your GP or prescribing specialist. They may consider alternative GLP-1 receptor agonists such as semaglutide (Wegovy), other weight management medications, referral to specialist weight management services, or bariatric surgery depending on your individual circumstances and eligibility.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript