Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults and adolescents with obesity. Whilst gastrointestinal side effects such as nausea and vomiting are well documented, some patients report experiencing taste disturbances during treatment. Loss of taste or altered taste perception (dysgeusia) is listed as an uncommon side effect in Saxenda's Summary of Product Characteristics, affecting up to 1 in 100 people. Understanding the potential connection between Saxenda and taste changes, alongside practical management strategies, can help patients maintain adequate nutrition whilst pursuing their weight management goals under medical supervision.
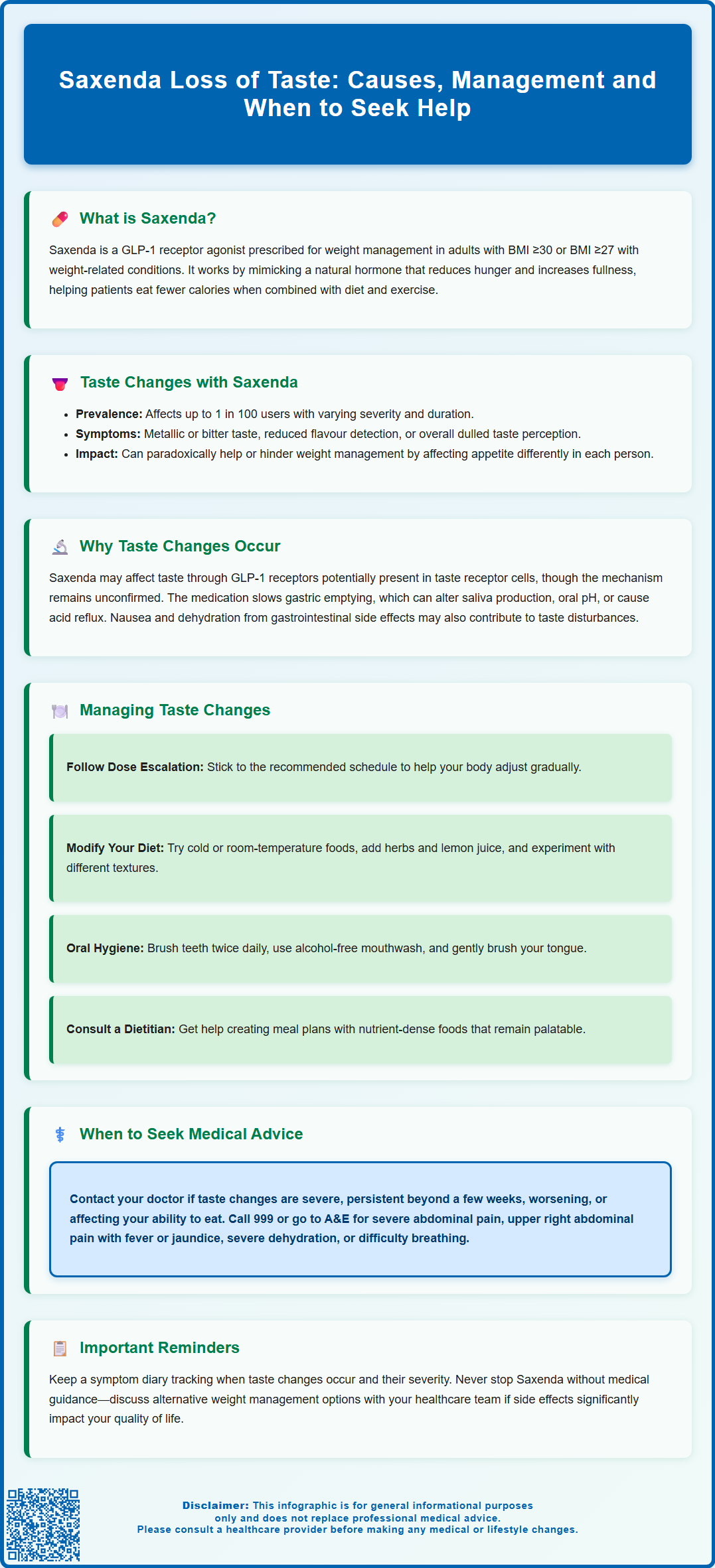
Summary: Saxenda can cause taste disturbances (dysgeusia) in up to 1 in 100 patients, though complete loss of taste is not specifically listed as a side effect.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults and adolescents with obesity.
- Taste alterations may manifest as metallic or bitter taste, reduced flavour detection, or overall dulling of taste perception.
- Possible mechanisms include GLP-1 receptor activation in taste cells, delayed gastric emptying, nausea-related changes, or dehydration from gastrointestinal side effects.
- Management strategies include maintaining oral hygiene, dietary modifications, adequate hydration, and following the recommended dose escalation schedule.
- Seek medical advice if taste changes are severe, persistent, progressively worsening, or accompanied by concerning symptoms such as severe abdominal pain or dehydration.
- Report suspected side effects to the MHRA through the Yellow Card Scheme to contribute to ongoing medication safety monitoring.
Table of Contents
Understanding Saxenda and Its Common Side Effects
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or those who are overweight (BMI ≥27 kg/m²) with weight-related health conditions such as type 2 diabetes, hypertension, or dyslipidaemia. It is also licensed for weight management in adolescents aged 12-<18 years with obesity (BMI corresponding to ≥30 kg/m² in adults) and body weight above 60 kg.
Saxenda belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates appetite and food intake.
The mechanism of action involves binding to GLP-1 receptors in the brain, particularly in areas that control appetite and satiety. This leads to reduced hunger, increased feelings of fullness after eating, and ultimately helps patients consume fewer calories. Saxenda is administered as a once-daily subcutaneous injection, typically in the abdomen, thigh, or upper arm, and is intended to be used alongside a reduced-calorie diet and increased physical activity.
Treatment starts with a dose of 0.6 mg daily, which is increased weekly by 0.6 mg until the maintenance dose of 3.0 mg daily is reached. This gradual dose escalation helps reduce gastrointestinal side effects. Treatment should be discontinued after 12 weeks on the 3.0 mg daily dose if patients have not lost at least 5% of their initial body weight.
Common side effects of Saxenda are predominantly gastrointestinal in nature and include nausea, vomiting, diarrhoea, constipation, and abdominal pain. These effects are usually most pronounced when starting treatment or increasing the dose, and often diminish over time as the body adjusts to the medication. According to the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA), nausea is the most frequently reported adverse effect, occurring in more than 1 in 10 patients.
Other reported side effects include injection site reactions, headache, dyspepsia, fatigue, dizziness, and changes in heart rate. People with type 2 diabetes taking Saxenda alongside sulfonylureas or insulin may experience an increased risk of hypoglycaemia and may need their diabetes medication doses adjusted.
Important safety warnings include the risk of pancreatitis (inflammation of the pancreas), gallbladder disease, dehydration potentially leading to acute kidney injury, and suicidal thoughts or behaviour. Saxenda should not be used during pregnancy or breastfeeding, and women of childbearing potential should use contraception during treatment.
Whilst gastrointestinal symptoms are well-documented, some patients report experiencing alterations in taste perception, which warrants further exploration to understand the potential connection between Saxenda and sensory changes.
Loss of Taste as a Potential Side Effect of Saxenda
Taste disturbances, including altered taste perception (dysgeusia), are listed as uncommon side effects (may affect up to 1 in 100 people) in Saxenda's UK Summary of Product Characteristics. Complete loss of taste (ageusia) is not specifically listed. The relatively low frequency means that many healthcare professionals and patients may not be aware of this potential side effect.
When taste changes do occur in patients taking Saxenda, they may manifest in several ways: a metallic or bitter taste in the mouth, reduced ability to detect certain flavours (particularly sweet or salty tastes), or an overall dulling of taste perception. These changes can affect appetite and eating habits, which may paradoxically either support or complicate weight management efforts depending on the individual's response.
The frequency and severity of taste-related symptoms appear to vary considerably between patients. Some individuals report mild, transient changes that resolve spontaneously within days or weeks, whilst others describe more persistent alterations that continue throughout treatment. In clinical practice, it can be challenging to determine whether taste changes are directly attributable to Saxenda, as multiple factors may contribute to sensory alterations.
Other common causes of taste disturbances include:
-
Viral infections including COVID-19 and upper respiratory tract infections
-
Dental problems or oral health issues
-
Other medications (including antibiotics, antidepressants, and blood pressure medicines)
-
Vitamin or mineral deficiencies
-
Neurological conditions
Patients experiencing taste disturbances should document the nature, onset, and duration of symptoms, as this information can help healthcare professionals assess whether the changes are likely related to Saxenda or may have alternative explanations. Maintaining open communication with prescribing clinicians is essential for appropriate management and to ensure that any concerning symptoms are properly evaluated.
Why Saxenda May Affect Taste Perception
The precise mechanism by which Saxenda might influence taste perception is not fully established, but several possible explanations exist based on the drug's pharmacological properties and systemic effects. These explanations remain largely hypothetical and require further research to confirm.
GLP-1 receptors are not only present in the pancreas and brain but are also found in various tissues throughout the body, including the gastrointestinal tract. Some research suggests these receptors may also be present in taste receptor cells, which could potentially influence taste perception when activated by liraglutide, though direct evidence in humans is currently limited.
One plausible explanation relates to Saxenda's gastrointestinal effects. The medication slows gastric emptying, which is part of its appetite-suppressing mechanism. This delayed gastric emptying can lead to feelings of fullness, nausea, and changes in digestive patterns. These gastrointestinal disturbances may indirectly affect taste perception through several pathways: altered saliva production, changes in oral pH, or the presence of refluxed gastric contents that create unpleasant tastes in the mouth. It's worth noting that the effect on gastric emptying tends to diminish over time with continued treatment.
Nausea and vomiting, which are common with Saxenda, may also contribute to taste alterations. Persistent nausea can create taste aversions or a general dulling of taste sensation, whilst vomiting can temporarily damage taste buds or alter the oral environment. Additionally, patients experiencing significant nausea may develop conditioned taste aversions to foods consumed whilst feeling unwell, which can be mistaken for a loss of taste.
Other potential contributing factors include dehydration (which can occur with gastrointestinal side effects) or nutritional changes associated with reduced calorie intake. Some researchers have also suggested that metabolic changes associated with weight loss itself, rather than the medication directly, could influence sensory perception.
Managing Taste Changes While Taking Saxenda
If you experience taste alterations whilst taking Saxenda, several practical strategies may help manage these symptoms and maintain adequate nutrition during your weight management journey. Firstly, ensure you are following the recommended dose escalation schedule, as starting with a lower dose and gradually increasing it allows your body to adjust to the medication and may reduce the intensity of side effects, including potential taste changes.
If taste changes are troublesome, discuss with your prescriber whether slowing the dose escalation or temporarily reducing the dose might help. Never adjust your dose without medical guidance.
Dietary modifications can be particularly helpful:
-
Experiment with temperature: Cold or room-temperature foods may be more palatable than hot meals if you're experiencing taste disturbances
-
Enhance flavours naturally: Use herbs, spices, lemon juice, or vinegar to add flavour without excessive salt or sugar
-
Try different textures: If certain textures become unappealing, explore alternatives that provide similar nutritional value
-
Maintain variety: Rotating different foods may help identify which items remain palatable and ensure balanced nutrition
-
Stay hydrated: Drinking adequate water throughout the day can help maintain saliva production and may improve taste perception
Oral hygiene plays a crucial role in managing taste changes. Brush your teeth at least twice daily, use an alcohol-free mouthwash, and consider gently brushing your tongue to remove any coating that might interfere with taste. Some patients find that rinsing with a solution of bicarbonate of soda and water helps neutralise unpleasant tastes, though you should discuss this with your dentist or doctor first.
If taste changes are affecting your ability to maintain adequate nutrition, consider consulting a registered dietitian who can help develop a meal plan that ensures you receive essential nutrients whilst accommodating your altered taste perception. They can suggest nutrient-dense foods that remain palatable and help prevent nutritional deficiencies that could develop if your diet becomes too restricted.
For people with type 2 diabetes who are taking Saxenda alongside sulfonylureas or insulin, monitor your blood glucose levels regularly, as taste changes might affect your eating patterns and potentially increase your risk of hypoglycaemia. Speak to your diabetes care team if you notice any changes in your glucose readings.
Keep a symptom diary documenting when taste changes occur, their severity, and any patterns you notice. This information can be valuable when discussing your experience with your GP or prescribing clinician, helping them determine whether adjustments to your treatment plan are necessary.
When to Seek Medical Advice About Taste Alterations
Whilst mild, transient taste changes may not require immediate medical attention, certain situations warrant prompt consultation with your GP or the healthcare professional who prescribed Saxenda. You should seek medical advice if taste alterations are severe, persistent (lasting more than a few weeks), or progressively worsening, as these patterns may indicate an underlying issue requiring investigation.
Contact your GP or prescribing clinician if you experience:
-
Complete loss of taste that significantly affects your ability to eat or enjoy food
-
Taste changes accompanied by other concerning symptoms such as severe nausea, persistent vomiting, signs of dehydration, or unexplained weight loss beyond your target
-
Development of a persistent metallic or bitter taste that doesn't resolve with oral hygiene measures
-
Taste alterations that lead to inadequate nutritional intake or significant changes in your eating patterns
-
Any symptoms suggesting an allergic reaction, including swelling of the face, lips, tongue, or throat
Seek emergency medical care (call 999 or go to A&E) if you experience:
-
Severe, persistent abdominal pain, with or without vomiting, which could indicate pancreatitis
-
Severe pain in the upper right side of your abdomen, possibly with fever or yellowing of the skin/eyes, which could suggest gallbladder disease
-
Signs of severe dehydration (extreme thirst, dry mouth, little or no urination, severe weakness, dizziness or lightheadedness)
-
Symptoms of anaphylaxis (severe allergic reaction) such as difficulty breathing, severe dizziness, or collapse
Your healthcare provider may wish to review your medication regimen, as taste disturbances can result from drug interactions or the cumulative effects of multiple medications. They may also consider whether dose adjustment or temporary discontinuation of Saxenda is appropriate whilst investigating the cause of your symptoms.
In some cases, your GP may recommend further investigations to rule out other causes of taste disturbances, such as vitamin or mineral deficiencies (particularly zinc or vitamin B12), thyroid disorders, oral infections, or neurological conditions. Blood tests may be arranged to assess nutritional status and screen for underlying health issues. If you've had a recent upper respiratory infection or COVID-19, this could also explain taste changes.
According to NICE guidance on obesity management (CG189), regular monitoring and follow-up are essential components of pharmacological weight management. If taste changes or other side effects are significantly impacting your quality of life or adherence to treatment, your healthcare team can discuss alternative weight management strategies, including other medications or non-pharmacological approaches. Never discontinue Saxenda abruptly without medical guidance, as your treatment plan should be reviewed and adjusted under professional supervision to ensure safe and effective weight management.
You can report any suspected side effects to the MHRA through the Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app. Reporting helps provide more information on the safety of this medicine.
Scientific References
- Saxenda | European Medicines Agency (EMA).
- Saxenda 6 mg/mL solution for injection in pre-filled pen - Summary of Product Characteristics.
- Liraglutide for managing overweight and obesity (TA664).
- Obesity: identification, assessment and management (CG189).
- Association of Glucagon-Like Peptide-1 Receptor Agonist Use With Risk of Gallbladder and Biliary Diseases: A Systematic Review and Meta-analysis of Randomized Clinical Trials.
Frequently Asked Questions
How common is loss of taste with Saxenda?
Taste disturbances (dysgeusia) are listed as uncommon side effects of Saxenda, affecting up to 1 in 100 people according to the UK Summary of Product Characteristics. Complete loss of taste (ageusia) is not specifically listed as a side effect.
What causes taste changes when taking Saxenda?
Possible mechanisms include GLP-1 receptor activation in taste receptor cells, delayed gastric emptying affecting oral pH and saliva production, nausea-related taste aversions, and dehydration from gastrointestinal side effects. The precise mechanism is not fully established and requires further research.
When should I contact my GP about taste changes on Saxenda?
Seek medical advice if taste alterations are severe, persistent (lasting more than a few weeks), progressively worsening, or affecting your ability to maintain adequate nutrition. Contact your GP if taste changes are accompanied by severe nausea, persistent vomiting, signs of dehydration, or other concerning symptoms.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










