Saxenda for PCOS weight loss is an emerging treatment option for women struggling with weight management related to polycystic ovary syndrome. Whilst not specifically licensed for PCOS in the UK, this GLP-1 receptor agonist has shown promise in clinical studies for addressing the metabolic challenges that make weight loss particularly difficult in this population. Women with PCOS often experience insulin resistance and hormonal imbalances that create a cycle of weight gain and worsening symptoms. Understanding how Saxenda works, the evidence supporting its use, and the safety considerations is essential for informed decision-making alongside your healthcare provider.
Summary: Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist used off-label for PCOS-related weight loss in the UK, showing promise in clinical studies for improving metabolic parameters and supporting weight management in women with polycystic ovary syndrome.
- Saxenda is licensed for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with comorbidities, but its use for PCOS specifically is off-label in the UK
- The medication works by mimicking GLP-1 hormone to reduce appetite, increase satiety, and slow gastric emptying, administered as a once-daily subcutaneous injection
- Clinical trials show greater weight loss versus placebo and metformin, with improvements in insulin sensitivity and metabolic markers relevant to PCOS
- Common side effects include gastrointestinal symptoms (nausea, diarrhoea, vomiting), typically most pronounced during dose escalation
- Treatment requires continuation criteria: at least 5% weight loss by 12 weeks, with regular monitoring for efficacy and adverse effects
- Comprehensive PCOS management should include lifestyle modification, metabolic screening, and consideration of alternatives such as metformin or combined oral contraceptives
Table of Contents
Understanding PCOS and Weight Management Challenges
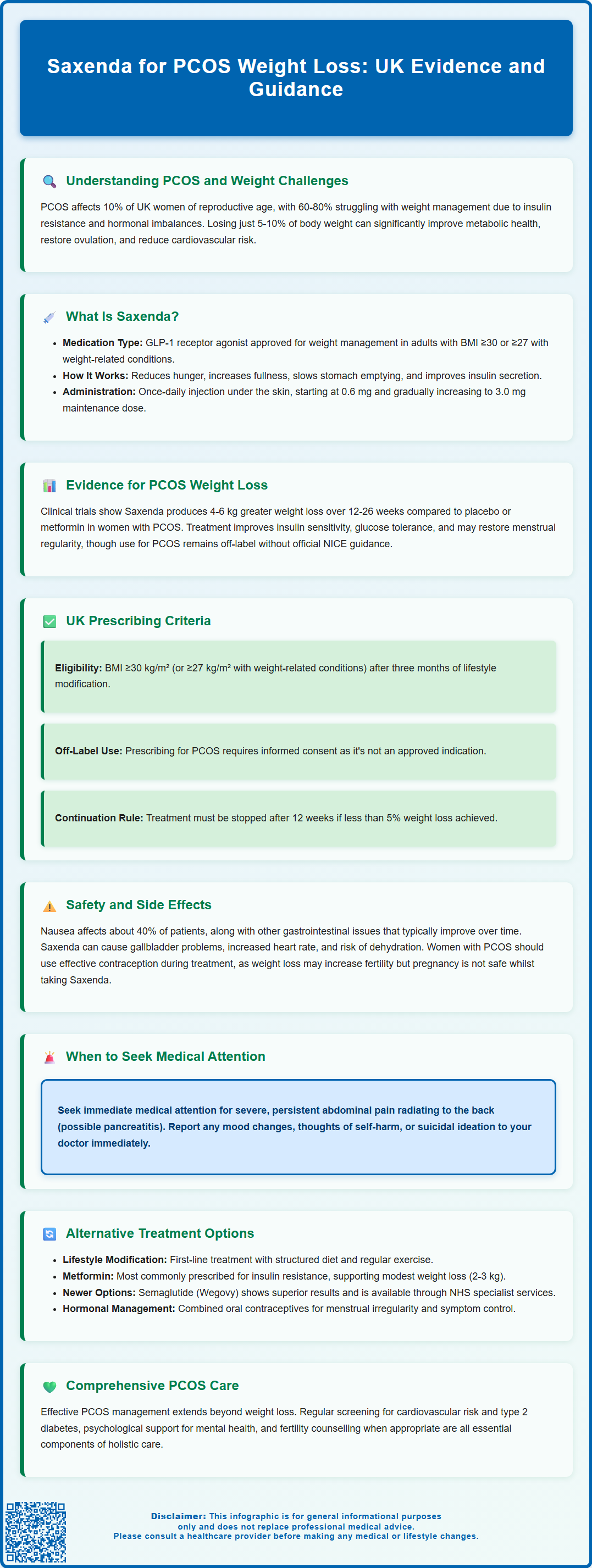
Polycystic ovary syndrome (PCOS) affects approximately 10% of women of reproductive age in the UK, making it one of the most common endocrine disorders. The condition is characterised by irregular ovulation, hyperandrogenism (excess male hormones), and/or polycystic ovarian morphology. A significant proportion of women with PCOS—estimated at 60–80%—experience difficulties with weight management, often presenting with central adiposity and insulin resistance.
The relationship between PCOS and weight is bidirectional and complex. Insulin resistance, present in up to 70% of women with PCOS regardless of body mass index (BMI), contributes to weight gain by promoting fat storage and making weight loss particularly challenging. Elevated insulin levels stimulate androgen production from the ovaries, exacerbating symptoms such as hirsutism, acne, and menstrual irregularity. This creates a metabolic cycle where excess weight worsens insulin resistance, which in turn aggravates PCOS symptoms.
Weight management is considered a cornerstone of PCOS treatment, as even modest weight loss of 5–10% of body weight can significantly improve metabolic parameters, restore ovulation, and reduce cardiovascular risk factors. However, women with PCOS often report greater difficulty losing weight compared to women without the condition, experiencing altered appetite regulation and increased hunger. This has led to growing interest in pharmacological interventions to support weight loss efforts.
Key challenges in PCOS weight management include:
-
Insulin resistance reducing metabolic efficiency
-
Hormonal imbalances affecting appetite regulation
-
Psychological factors including depression and anxiety
-
Reduced response to conventional diet and exercise interventions
Regular screening for associated conditions is recommended, including HbA1c or fasting glucose, lipid profile, and blood pressure monitoring to assess cardiovascular and diabetes risk.
What Is Saxenda and How Does It Work?
Saxenda (liraglutide 3.0 mg) is an injectable prescription medicine licensed in the UK for weight management in adults with a BMI of 30 kg/m² or above, or 27 kg/m² or above with at least one weight-related comorbidity. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, originally developed for type 2 diabetes management but subsequently approved at higher doses for obesity treatment. It is important to note that using Saxenda specifically for PCOS is considered off-label in the UK and requires informed consent.
The mechanism of action of liraglutide involves mimicking the naturally occurring hormone GLP-1, which is released from the intestine in response to food intake. By activating GLP-1 receptors in multiple tissues, Saxenda produces several beneficial effects that facilitate weight loss. In the brain, it acts on appetite centres in the hypothalamus to reduce hunger and increase feelings of satiety. In the gastrointestinal tract, it slows gastric emptying, prolonging the sensation of fullness after meals. Additionally, it enhances glucose-dependent insulin secretion from pancreatic beta cells whilst suppressing inappropriate glucagon release.
Saxenda is administered once daily via subcutaneous injection, typically in the abdomen, thigh, or upper arm. The treatment follows a gradual dose escalation protocol, starting at 0.6 mg daily and increasing weekly by 0.6 mg increments until reaching the maintenance dose of 3.0 mg daily. This titration schedule helps minimise gastrointestinal side effects, which are common during treatment initiation. Injections can be given at any time of day, independent of meals, but should be administered at a consistent time each day.
Pharmacological properties:
-
Half-life: Approximately 13 hours, allowing once-daily dosing
-
Onset of action: Appetite suppression typically noticed within days to weeks
-
Metabolism: Degraded endogenously similar to native GLP-1
-
Excretion: Metabolites eliminated via urine and faeces
Evidence for Saxenda in PCOS-Related Weight Loss
Whilst Saxenda is not specifically licensed for PCOS, emerging clinical evidence suggests potential benefits for weight management in this population. Several randomised controlled trials have investigated GLP-1 receptor agonists in women with PCOS, demonstrating promising results. A systematic review examining liraglutide use in PCOS found that participants achieved significantly greater weight loss compared to placebo or metformin, with reductions typically ranging from 4–6 kg over 12–26 weeks.
Beyond weight loss, studies have reported improvements in metabolic parameters particularly relevant to PCOS. Research indicates that liraglutide treatment can enhance insulin sensitivity, reduce fasting insulin levels, and improve glucose tolerance—addressing the underlying metabolic dysfunction characteristic of PCOS. Some trials have also documented improvements in menstrual regularity, with increased ovulation rates observed in women receiving GLP-1 agonist therapy, though these reproductive outcomes are generally considered secondary and likely mediated by weight loss and metabolic improvements. Similarly, modest reductions in androgen levels and improvements in hirsutism scores have been reported, though these effects appear secondary to weight loss and metabolic improvements.
However, it is important to note that most studies have been relatively small and of short to moderate duration. Long-term data specifically examining Saxenda in PCOS populations remain limited. The majority of evidence comes from studies conducted in women with PCOS who also had obesity or overweight, and results may not generalise to all PCOS phenotypes. Furthermore, there is no official NICE guidance specifically recommending Saxenda for PCOS management, and its use in this context remains off-label, requiring shared decision-making between clinician and patient.
Evidence summary:
-
Greater weight loss versus placebo and metformin in clinical trials
-
Improvements in insulin sensitivity and metabolic markers
-
Potential benefits for menstrual regularity and ovulation, likely secondary to weight loss
-
Limited long-term data specific to PCOS populations
Prescribing Criteria and Eligibility in the UK
In the UK, Saxenda is licensed for weight management in adults with a BMI of 30 kg/m² or above, or 27 kg/m² or above in the presence of weight-related comorbidities such as type 2 diabetes, hypertension, dyslipidaemia, or obstructive sleep apnoea. However, NHS access is more restricted and follows NICE Technology Appraisal guidance, which limits availability to specific patient groups within specialist weight management services.
It's important to understand that using Saxenda specifically for PCOS is an off-label prescription, as PCOS is not listed as an indication in the product licence. While PCOS with metabolic complications may be considered a relevant comorbidity by some clinicians, this remains at prescriber discretion and requires informed consent.
Before initiating Saxenda, patients should have attempted weight loss through a comprehensive lifestyle modification programme, typically involving dietary changes and increased physical activity for at least three months. Treatment should be prescribed as part of a multidisciplinary approach to weight management, ideally within specialist weight management services.
Continuation criteria are clearly defined in the product licence: treatment should only be continued beyond 12 weeks if the patient has lost at least 5% of their initial body weight. If this threshold is not achieved, Saxenda should be discontinued. Regular monitoring is essential, including assessment of weight loss progress, tolerability, and any adverse effects.
UK contraindications include:
-
Hypersensitivity to liraglutide or any excipients
-
Pregnancy
Important precautions and warnings:
-
Not recommended during breastfeeding
-
Caution in severe renal or hepatic impairment
-
Caution in inflammatory bowel disease or diabetic gastroparesis
-
History of pancreatitis
-
Risk of gallbladder disease with weight loss
Saxenda availability varies by region within NHS specialist weight management services, subject to local formulary decisions and NICE guidance. Private prescription is also an option, though costs can be substantial.
Safety Considerations and Side Effects
Saxenda is generally well-tolerated, but patients should be informed about potential adverse effects before commencing treatment. The most common side effects are gastrointestinal in nature, affecting the majority of users to some degree. These include nausea (affecting approximately 40% of patients), diarrhoea, constipation, vomiting, dyspepsia, and abdominal pain. Gastrointestinal symptoms are typically most pronounced during dose escalation and often diminish over time as tolerance develops. Slower dose titration and maintaining adequate hydration can help manage these effects.
More serious but less common adverse effects require clinical vigilance. Acute pancreatitis has been reported with GLP-1 receptor agonists, and patients should be advised to seek immediate medical attention if they experience severe, persistent abdominal pain radiating to the back. Gallbladder disorders, including cholelithiasis and cholecystitis, occur more frequently with rapid weight loss and have been associated with liraglutide use.
Additional important safety considerations include:
-
Increased heart rate (typically 2-3 beats per minute)
-
Risk of dehydration and acute kidney injury, particularly with severe gastrointestinal side effects
-
Rare cases of intestinal obstruction (ileus)
-
Reports of suicidal thoughts or behaviour in some patients
Hypoglycaemia is uncommon with Saxenda monotherapy but may occur if used alongside other glucose-lowering medications. Injection site reactions, including redness, itching, or bruising, affect approximately 10% of users but are usually mild and transient.
Important safety advice for patients:
-
Report severe or persistent abdominal pain immediately
-
Seek urgent medical care for persistent vomiting, severe abdominal pain, or signs of intestinal obstruction
-
Maintain adequate hydration, especially if experiencing vomiting or diarrhoea
-
Use effective contraception, as weight loss may increase fertility in PCOS and pregnancy is contraindicated during treatment
-
Report any changes in mood, thoughts of self-harm, or suicidal ideation
-
Contact your GP if side effects become intolerable or concerning symptoms develop
-
Attend regular monitoring appointments to assess treatment response and safety
-
Report suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app)
Alternatives and Comprehensive PCOS Management
Whilst Saxenda represents one pharmacological option for weight management in PCOS, a comprehensive treatment approach should address the multifaceted nature of the condition. Lifestyle modification remains the foundation of PCOS management, with structured diet and exercise programmes recommended as first-line interventions. A modest calorie deficit combined with regular physical activity can improve insulin sensitivity, promote weight loss, and ameliorate PCOS symptoms even without pharmacological support.
Metformin is the most commonly prescribed medication for PCOS in the UK, particularly for women with insulin resistance or impaired glucose tolerance. Whilst not licensed specifically for PCOS, it is widely used off-label and can support modest weight loss (typically 2–3 kg), improve metabolic parameters, and restore menstrual regularity in some women. Metformin may be considered before or alongside Saxenda, though combination therapy requires careful monitoring.
Other weight management medications licensed in the UK include orlistat, a lipase inhibitor that reduces dietary fat absorption, though its gastrointestinal side effects and modest efficacy (typically 3–5% weight loss) limit its appeal. Newer agents such as semaglutide (Wegovy), a once-weekly GLP-1 receptor agonist, have shown superior weight loss outcomes in clinical trials and are available through NHS specialist services for eligible patients according to NICE Technology Appraisal guidance.
For women with PCOS not primarily focused on weight loss, combined oral contraceptives effectively manage menstrual irregularity and hyperandrogenic symptoms such as hirsutism and acne. Anti-androgen medications like spironolactone or cyproterone acetate may be added for persistent androgenic symptoms, though effective contraception is essential with these treatments. Cyproterone acetate carries an MHRA warning about the risk of meningioma with long-term use. Women seeking fertility may require ovulation induction, with letrozole often used first-line in UK practice, and clomifene citrate as an alternative.
Comprehensive PCOS management should include:
-
Individualised dietary advice, potentially with dietitian support
-
Regular physical activity (at least 150 minutes moderate intensity weekly)
-
Psychological support for associated anxiety, depression, or body image concerns
-
Cardiovascular risk assessment and management
-
Screening for type 2 diabetes and metabolic syndrome
-
Fertility counselling when appropriate
Patients should be encouraged to discuss all available options with their healthcare provider to develop a personalised treatment plan addressing their specific symptoms, priorities, and circumstances. Regular follow-up is essential to monitor treatment response and adjust management strategies as needed.
Frequently Asked Questions
Is Saxenda approved for PCOS treatment in the UK?
Saxenda is not specifically licensed for PCOS in the UK; its use for this condition is considered off-label and requires informed consent. It is licensed for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidities.
How effective is Saxenda for weight loss in women with PCOS?
Clinical trials show that liraglutide produces greater weight loss in women with PCOS compared to placebo and metformin, with studies reporting reductions typically ranging from 4–6 kg over 12–26 weeks, alongside improvements in insulin sensitivity and metabolic parameters.
What are the main side effects of Saxenda?
The most common side effects are gastrointestinal, including nausea (affecting approximately 40% of patients), diarrhoea, constipation, vomiting, and abdominal pain. These symptoms are typically most pronounced during dose escalation and often diminish over time as tolerance develops.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript