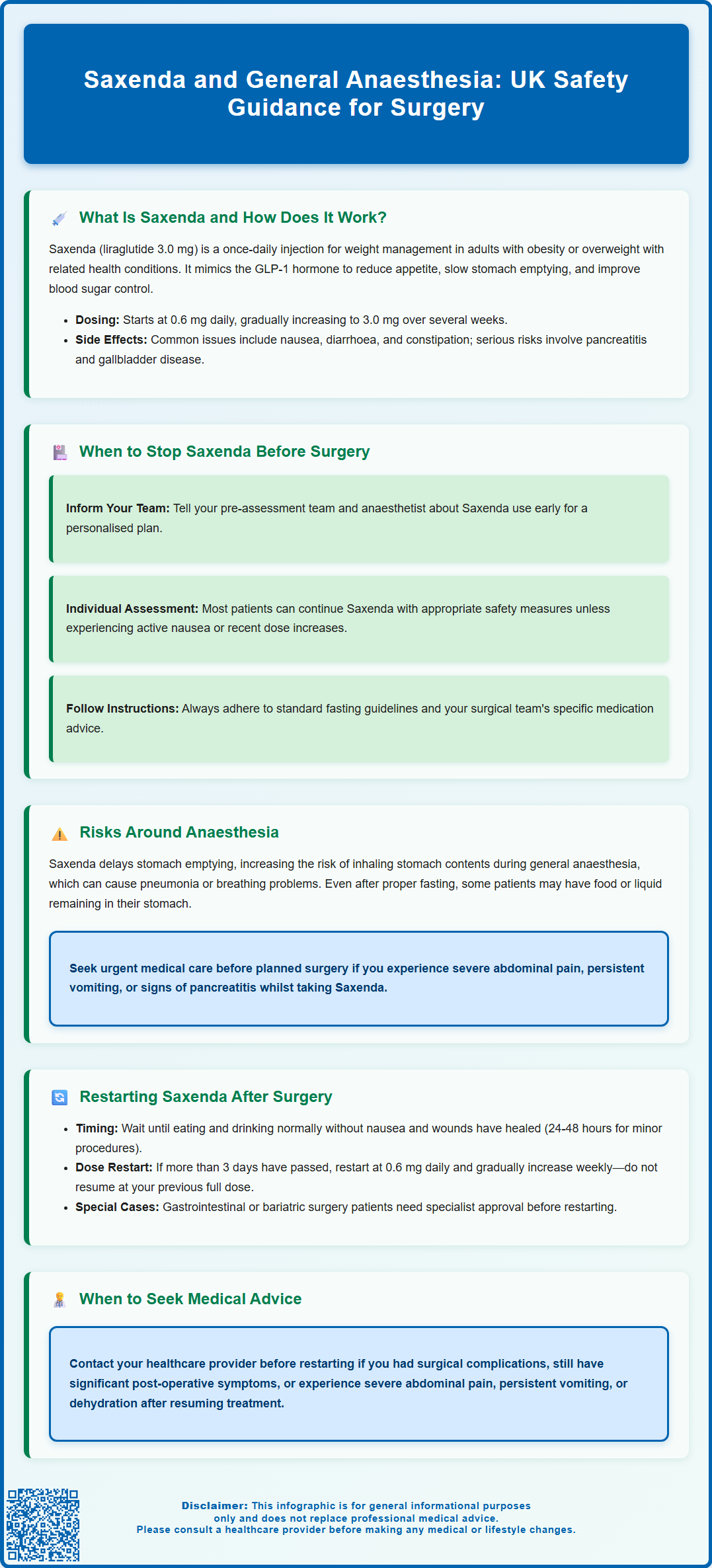
Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist prescribed for weight management in the UK. If you are taking Saxenda and have surgery planned, understanding how this medication interacts with general anaesthesia is essential for your safety. The primary concern relates to Saxenda's effect on gastric emptying, which may influence aspiration risk during anaesthesia. This article explains when to discuss stopping Saxenda before surgery, the risks involved, and guidance on safely restarting treatment afterwards, in line with UK clinical practice and MHRA-approved prescribing information.
Summary: Saxenda (liraglutide) may delay gastric emptying, potentially increasing aspiration risk during general anaesthesia, requiring individualised perioperative management with your surgical and anaesthetic team.
- Saxenda is a GLP-1 receptor agonist that slows gastric emptying and reduces appetite for weight management.
- Management before surgery should be individualised; many patients continue Saxenda with appropriate risk mitigation strategies.
- The main perioperative concern is pulmonary aspiration due to delayed gastric emptying during anaesthesia.
- Always inform your surgical team about Saxenda use and follow their specific preoperative instructions.
- Restart Saxenda only after resuming normal oral intake; if more than 3 days have elapsed, restart at 0.6 mg daily with dose escalation.
- Patients undergoing gastrointestinal or bariatric surgery require specialist input before restarting Saxenda.
Table of Contents
What Is Saxenda and How Does It Work?
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity or those who are overweight with weight-related health conditions. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists. Saxenda is administered once daily via subcutaneous injection, typically in the abdomen, thigh, or upper arm.
The mechanism of action involves mimicking the naturally occurring hormone GLP-1, which is released from the intestine after eating. Liraglutide works by:
-
Reducing appetite – acting on areas of the brain that regulate hunger and satiety
-
Slowing gastric emptying – food remains in the stomach for longer, promoting feelings of fullness (though this effect may diminish over time)
-
Improving glycaemic control – enhancing insulin secretion and suppressing glucagon release in a glucose-dependent manner
Saxenda is prescribed alongside a reduced-calorie diet and increased physical activity. Treatment starts at 0.6 mg daily, increasing weekly to the maintenance dose of 3.0 mg daily. According to NICE guidance (TA664), treatment should be discontinued if patients have not lost at least 5% of their initial body weight after 12 weeks on the 3.0 mg daily dose.
Common adverse effects include nausea, diarrhoea, constipation, vomiting, and injection site reactions. Important safety considerations include risks of pancreatitis, gallbladder disease, dehydration leading to acute kidney injury, and suicidal ideation. Saxenda should not be used during pregnancy or breastfeeding, or in combination with other GLP-1 receptor agonists.
The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Saxenda for weight management, and NICE guidance recognises GLP-1 receptor agonists within specific clinical pathways for obesity treatment.
When to Stop Saxenda Before Surgery
Management of Saxenda before surgery should be based on individual risk assessment rather than a standard discontinuation period. The primary concern relates to the medication's effect on gastric emptying, which may increase the risk of pulmonary aspiration during anaesthesia induction and recovery.
For elective procedures, current UK guidance generally supports:
-
Continuing Saxenda for most patients – with appropriate risk mitigation strategies
-
Discussing Saxenda use with your pre-assessment team and anaesthetist as early as possible
-
Following specific instructions from your surgical team – they may recommend temporary discontinuation based on your individual circumstances, particularly if you have active gastrointestinal symptoms or are in the dose-escalation phase
If you are considered at higher risk for aspiration (e.g., active nausea/vomiting, recent dose increases, known gastroparesis), your anaesthetist may recommend:
-
A liquid-only diet for 24 hours before surgery
-
Treating you as having a "full stomach" regardless of fasting time
-
Using modified anaesthetic techniques such as rapid sequence induction
-
Performing gastric ultrasound to assess stomach contents, where available
For emergency surgery, your anaesthetist will implement appropriate precautions based on your individual risk assessment.
Patients should follow standard preoperative fasting instructions provided by their hospital. Your local hospital may have specific perioperative medicines policies regarding GLP-1 receptor agonists, which your surgical team will follow.
Always inform your surgical team about all medications you are taking, including Saxenda, and follow their specific advice for your situation.
Risks of Using Saxenda Around the Time of Anaesthesia
The main concern with Saxenda around the time of general anaesthesia is the potential for pulmonary aspiration – the inhalation of gastric contents into the lungs. This complication can lead to aspiration pneumonitis, pneumonia, acute respiratory distress, and in severe cases, can be serious.
Why is there concern about aspiration risk?
GLP-1 receptor agonists like Saxenda can delay gastric emptying, meaning food and liquid may remain in the stomach for longer periods. During general anaesthesia, protective airway reflexes are suppressed. Studies using gastric ultrasound have shown that some patients taking GLP-1 medications may have increased gastric contents even after appropriate fasting periods, though the evidence linking this to clinical aspiration events remains limited.
Additional perioperative considerations include:
-
Glycaemic control – whilst Saxenda has glucose-lowering effects, the risk of hypoglycaemia is generally low unless used alongside insulin or sulphonylureas in people who also have diabetes
-
Nausea and vomiting – Saxenda commonly causes gastrointestinal side effects, which may complicate postoperative recovery
-
Fluid and nutritional status – patients experiencing significant nausea or reduced oral intake before surgery may require additional assessment
-
Gallbladder disease – Saxenda increases the risk of gallstones, which may be relevant for abdominal surgery
-
Dehydration risk – particularly important in the perioperative period
The decision to proceed with surgery while on Saxenda should be made collaboratively between your prescribing physician, surgeon, and anaesthetist, with appropriate risk mitigation strategies in place.
If you develop symptoms such as severe abdominal pain, persistent vomiting, or signs of pancreatitis, contact your GP or seek urgent medical attention, particularly if surgery is planned. Suspected adverse reactions to Saxenda should be reported via the MHRA Yellow Card Scheme.
Restarting Saxenda After Surgery: What You Need to Know
Restarting Saxenda after surgery requires careful consideration of your recovery, nutritional status, and the type of procedure performed. Decisions should be individualised in consultation with your healthcare team.
General principles for restarting Saxenda post-surgery:
-
Wait until you have resumed normal oral intake – you should be eating and drinking normally without significant nausea or vomiting
-
Ensure adequate wound healing – particularly important after gastrointestinal surgery
-
For minor procedures, this may be possible within 24-48 hours of surgery
Important dosing information when restarting:
-
According to the Saxenda Summary of Product Characteristics (SmPC), if more than 3 days have elapsed since your last dose, you should restart at 0.6 mg daily and follow the dose-escalation schedule (increasing weekly) back to your maintenance dose
-
Do not restart at your previous maintenance dose after a significant break, as this may increase side effects
Special considerations:
For patients who have undergone gastrointestinal or bariatric surgery, restarting Saxenda requires specialist input from both your surgical and weight management teams. Some bariatric procedures already significantly alter gastric emptying and appetite regulation, and adding Saxenda may require modified dosing strategies or may not be appropriate.
Monitoring after restarting:
-
Watch for common side effects (nausea, diarrhoea, constipation)
-
Monitor your weight and nutritional intake, particularly if your appetite was already reduced post-surgery
-
Contact your GP if you develop severe abdominal pain, persistent vomiting, or signs of dehydration
When to seek medical advice:
If you are unsure when to restart Saxenda, or if you experience any concerning symptoms after resuming treatment, contact your prescribing clinician or GP. Do not restart Saxenda without medical guidance if you have had complications during or after surgery, or if you are still experiencing significant postoperative symptoms. Your healthcare team can provide personalised advice based on your surgical outcome and overall recovery progress.
Frequently Asked Questions
Should I stop taking Saxenda before having surgery?
Management should be individualised based on your risk assessment. Many patients continue Saxenda with appropriate precautions, but your anaesthetist may recommend temporary discontinuation if you have active gastrointestinal symptoms or are at higher aspiration risk. Always discuss Saxenda use with your surgical team during pre-assessment.
Why is Saxenda a concern during general anaesthesia?
Saxenda can delay gastric emptying, meaning stomach contents may remain longer even after fasting. During general anaesthesia, protective airway reflexes are suppressed, potentially increasing the risk of pulmonary aspiration if gastric contents enter the lungs.
When can I restart Saxenda after surgery?
Restart Saxenda once you have resumed normal eating and drinking without significant nausea or vomiting. If more than 3 days have passed since your last dose, restart at 0.6 mg daily and follow the weekly dose-escalation schedule back to your maintenance dose, as per the Summary of Product Characteristics.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript