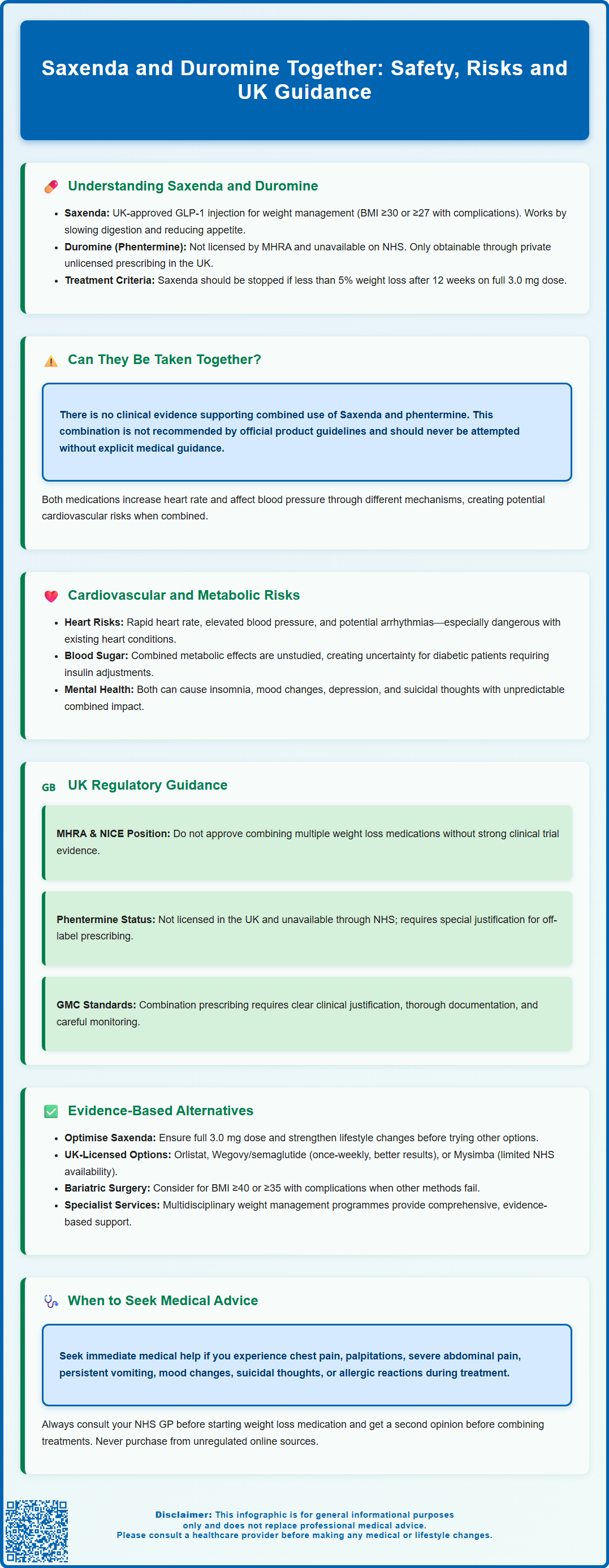
Saxenda (liraglutide) and phentermine (branded as Duromine in some countries) are distinct weight management medications with different mechanisms and regulatory status in the UK. Saxenda is an MHRA-licensed GLP-1 receptor agonist used for chronic weight management, whilst phentermine is not currently licensed for use in the UK. Patients sometimes enquire about combining these agents to enhance weight loss, but there is no clinical evidence supporting this approach. Understanding the safety concerns, regulatory guidance, and evidence-based alternatives is essential for anyone considering weight management pharmacotherapy.
Summary: Saxenda and Duromine (phentermine) should not be taken together as there is no clinical evidence supporting this combination and it is not recommended by UK regulatory authorities.
- Saxenda is an MHRA-licensed GLP-1 receptor agonist for weight management; phentermine is not licensed in the UK.
- No clinical trials have examined the safety or efficacy of combining liraglutide with phentermine.
- Both medications can affect heart rate and blood pressure through different mechanisms, potentially amplifying cardiovascular risks.
- The Saxenda Summary of Product Characteristics states that concomitant use with other weight loss products is not recommended.
- Evidence-based alternatives include optimising single-agent therapy, switching to licensed alternatives like Wegovy, or intensive lifestyle interventions.
- Patients should consult their GP or specialist before combining any weight loss medications and report adverse effects via the Yellow Card scheme.
Table of Contents
- Understanding Saxenda and Duromine: Mechanisms and Approved Uses
- Can Saxenda and Duromine Be Taken Together? Clinical Evidence and Safety Concerns
- Risks of Combining Saxenda and Duromine: Cardiovascular and Metabolic Effects
- UK Regulatory Guidance on Combining Weight Loss Medications
- Evidence-Based Alternatives to Combining Saxenda and Duromine
- When to Seek Medical Advice About Weight Loss Treatment Options
- Frequently Asked Questions
Understanding Saxenda and Duromine: Mechanisms and Approved Uses
Saxenda (liraglutide) and phentermine (sometimes branded as Duromine outside the UK) are two distinct medications used for weight management, each with different mechanisms of action and regulatory status in the UK.
Saxenda is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for chronic weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater in the presence of at least one weight-related comorbidity such as type 2 diabetes or hypertension. Administered as a once-daily subcutaneous injection, liraglutide works by mimicking the action of the naturally occurring hormone GLP-1. It slows gastric emptying, increases feelings of satiety, and reduces appetite through effects on the hypothalamus. NICE Technology Appraisal (TA631) supports its use as part of a comprehensive weight management programme that includes dietary modification and increased physical activity. Treatment should be discontinued if at least 5% weight loss has not been achieved after 12 weeks on the full 3.0 mg daily dose.
Phentermine is a sympathomimetic amine that acts as an appetite suppressant. It stimulates the release of noradrenaline in the central nervous system, which reduces hunger signals. It is important to note that phentermine (including branded versions such as Duromine) is not currently licensed by the MHRA for use in the UK and is not available on the NHS. Any use in the UK would be considered unlicensed and typically only available through private prescribing channels.
Saxenda requires careful patient selection, ongoing monitoring, and should only be prescribed by healthcare professionals experienced in obesity management. Key precautions include monitoring for pancreatitis (severe abdominal pain), gallbladder disease, and avoiding use during pregnancy or breastfeeding. Understanding the distinct regulatory status and pharmacological profiles of these medications is essential when considering weight management options.
Can Saxenda and Duromine Be Taken Together? Clinical Evidence and Safety Concerns
There is no official clinical evidence supporting the combined use of Saxenda and phentermine, and this combination is not recommended. According to the Saxenda Summary of Product Characteristics (SmPC), concomitant use with other weight loss products has not been studied and is not recommended.
The absence of robust clinical trials examining the safety and efficacy of combining liraglutide with phentermine means that healthcare professionals lack evidence-based data to guide such prescribing decisions. While some studies have explored combinations of GLP-1 receptor agonists with other weight loss agents, phentermine's sympathomimetic properties make it a particularly concerning candidate for combination therapy without proper clinical validation.
Key safety concerns include the potential for additive adverse effects, particularly on the cardiovascular system. Both medications can affect heart rate and blood pressure, though through different mechanisms. Saxenda's product information warns of increases in heart rate (average 2–3 beats per minute), whilst phentermine is known to cause tachycardia, palpitations, and elevated blood pressure as sympathomimetic effects. Combining these agents could theoretically amplify cardiovascular risks.
Additionally, both medications affect the central nervous system and gastrointestinal function. Overlapping side effects such as nausea, constipation, headache, and dizziness may be intensified when used together, potentially reducing treatment tolerability and adherence. The lack of pharmacokinetic interaction studies means potential drug-drug interactions remain uncharacterised. GLP-1 receptor agonists like Saxenda can delay gastric emptying, which may affect the absorption of oral medications like phentermine.
Patients should never combine prescription weight loss medications without explicit guidance from their prescribing clinician. Any healthcare professional considering such an approach would need to provide exceptionally close monitoring and document clear clinical justification, given the absence of supporting evidence and potential safety implications. Such prescribing would fall under the GMC's guidance on off-label and unlicensed medicines.
Risks of Combining Saxenda and Duromine: Cardiovascular and Metabolic Effects
The cardiovascular risks associated with combining Saxenda and phentermine represent the most significant safety concern. Phentermine's sympathomimetic activity stimulates the sympathetic nervous system, leading to increased noradrenaline release. This can cause tachycardia (rapid heart rate), elevated blood pressure, palpitations, and in susceptible individuals, may precipitate arrhythmias. Based on non-UK product information, phentermine is typically contraindicated in patients with cardiovascular disease, uncontrolled hypertension, and hyperthyroidism.
Saxenda has been associated with modest increases in resting heart rate, averaging 2–3 beats per minute in clinical trials, though some patients experience more substantial elevations. The LEADER cardiovascular outcomes trial demonstrated that liraglutide (at the 1.8 mg diabetes dose, not the 3.0 mg obesity dose) did not increase major adverse cardiovascular events in patients with type 2 diabetes, but the cardiovascular safety profile when combined with sympathomimetic agents remains unknown. Patients with pre-existing cardiac conditions, including coronary artery disease or heart failure, would face amplified risks from this combination.
Metabolic and endocrine effects also warrant consideration. Both medications influence glucose metabolism, though through different pathways. Saxenda improves glycaemic control in patients with type 2 diabetes, whilst phentermine may affect insulin sensitivity. The combined metabolic impact has not been systematically studied, creating uncertainty about glucose management in diabetic patients. Patients with diabetes using Saxenda alongside insulin or sulfonylureas may require dose adjustments to prevent hypoglycaemia.
Gastrointestinal adverse effects are common with Saxenda, particularly nausea (occurring in approximately 40% of patients), vomiting, diarrhoea, and constipation. Saxenda carries warnings about pancreatitis; patients should seek urgent medical attention for severe, persistent abdominal pain. There is also an increased risk of gallbladder disease, including cholelithiasis and cholecystitis. Phentermine can cause dry mouth, constipation, and gastrointestinal disturbance. Combining these medications may result in intolerable gastrointestinal symptoms that compromise nutritional intake and treatment adherence.
Psychiatric and neurological effects represent another concern. Phentermine can cause insomnia, nervousness, restlessness, and mood changes. The Saxenda SmPC notes that patients should be monitored for depression or suicidal thoughts. The combined neuropsychiatric impact of these agents is unpredictable and could potentially exacerbate mental health conditions.
UK Regulatory Guidance on Combining Weight Loss Medications
UK regulatory bodies, including the MHRA and NICE, do not endorse the routine combination of multiple weight loss pharmacotherapies without substantial clinical evidence. The MHRA's licensing framework requires that medication combinations undergo rigorous clinical trials demonstrating both safety and efficacy before approval for concurrent use.
NICE guidance on obesity management (Clinical Guideline 189) and specific Technology Appraisals for weight loss medications (TA631 for liraglutide and TA664 for semaglutide) provide comprehensive recommendations for pharmacological interventions. These guidelines advise that pharmacotherapy should only be prescribed as part of a multicomponent intervention, with ongoing support for behaviour change, dietary modification, and physical activity. The guidance specifies criteria for initiating and continuing treatment with individual agents but does not support combining multiple prescription weight loss medications.
Phentermine is not currently licensed by the MHRA for use in the UK and is not available on the NHS. Any prescribing of phentermine in the UK would be considered unlicensed use, requiring adherence to the GMC's guidance on prescribing unlicensed medicines. This includes ensuring there is sufficient evidence or experience of using the medicine to demonstrate its safety and efficacy, taking responsibility for prescribing the medicine and for overseeing the patient's care, and obtaining informed consent from the patient.
The General Medical Council's prescribing guidance emphasises that doctors must prescribe within their competence and ensure that prescribing decisions are based on the best available evidence. Off-label prescribing (using medications outside their licensed indications or in unapproved combinations) requires clear clinical justification, informed patient consent, and careful documentation. Given the absence of evidence supporting Saxenda and phentermine combination therapy, such prescribing would be difficult to justify.
Patients should be aware that reputable NHS and private healthcare providers will follow these regulatory frameworks. Any practitioner suggesting combination therapy without thorough cardiovascular assessment, clear rationale, and intensive monitoring should prompt patients to seek a second opinion from another qualified healthcare professional.
Evidence-Based Alternatives to Combining Saxenda and Duromine
Rather than combining medications with uncertain safety profiles, evidence-based alternatives offer safer and more effective approaches to weight management.
Optimising single-agent pharmacotherapy represents the first-line approach. If Saxenda alone provides insufficient weight loss, the prescriber should review adherence, dosing (ensuring titration to the full 3.0 mg daily dose if tolerated), and the intensity of accompanying lifestyle interventions before considering alternatives. Treatment should be discontinued if less than 5% of initial body weight is lost after 12 weeks on the full dose.
Alternative pharmacological options licensed in the UK include:
-
Orlistat – a lipase inhibitor that reduces dietary fat absorption, available both on prescription and over-the-counter (as Alli). It has an established safety profile and can be used long-term.
-
Wegovy (semaglutide 2.4 mg) – a once-weekly GLP-1 receptor agonist that has demonstrated superior weight loss compared to liraglutide in head-to-head trials. NICE (TA664) recommends it for adults with a BMI of at least 35 kg/m² (or 30 kg/m² with weight-related comorbidities) and at least one weight-related condition. Access is typically via specialist weight management services.
-
Mysimba (naltrexone/bupropion) – a combination tablet affecting appetite and reward pathways. While licensed in the UK, NICE has not recommended it for routine NHS use (terminated appraisal), so availability is limited and often through private healthcare providers.
Intensive lifestyle interventions remain the cornerstone of weight management. NICE recommends multicomponent programmes incorporating:
-
Structured dietary approaches with ongoing dietetic support
-
Progressive physical activity programmes tailored to individual capability
-
Behavioural strategies addressing eating patterns and psychological factors
-
Group or individual psychological support when appropriate
Bariatric surgery should be considered for patients with BMI ≥40 kg/m² (or ≥35 kg/m² with comorbidities) when non-surgical measures have been unsuccessful. NICE also recommends considering assessment for bariatric surgery for people with a BMI of 30-34.9 kg/m² who have recent-onset type 2 diabetes. Lower BMI thresholds may apply for people of South Asian and some other minority ethnic groups. Procedures such as gastric bypass or sleeve gastrectomy offer substantial, sustained weight loss with metabolic benefits.
Specialist weight management services can provide comprehensive assessment and access to multidisciplinary expertise, ensuring patients receive evidence-based, individualised treatment plans rather than potentially hazardous medication combinations.
When to Seek Medical Advice About Weight Loss Treatment Options
Patients should consult their GP or specialist before starting, stopping, or combining any weight loss medications. Immediate medical advice is essential in several circumstances:
Before starting treatment, a comprehensive medical assessment is necessary to:
-
Evaluate suitability for pharmacotherapy based on BMI and comorbidities
-
Screen for contraindications, including cardiovascular disease, uncontrolled hypertension, psychiatric conditions, and pregnancy
-
Review current medications for potential interactions
-
Establish baseline measurements (weight, blood pressure, heart rate, blood glucose)
-
Discuss realistic expectations, potential side effects, and treatment duration
During treatment, patients should contact their healthcare provider if they experience:
-
Cardiovascular symptoms – chest pain, palpitations, significant increases in heart rate, breathlessness, or leg swelling
-
Severe gastrointestinal effects – persistent vomiting, severe abdominal pain, or signs of pancreatitis (severe upper abdominal pain radiating to the back)
-
Mood changes – depression, suicidal thoughts, or significant anxiety
-
Allergic reactions – rash, swelling, or difficulty breathing
-
Inadequate weight loss – less than 5% body weight reduction after 12 weeks at full dose (a specific stopping rule for Saxenda)
Patients considering combining medications or who have been advised to do so by non-NHS practitioners should seek a second opinion from their NHS GP or a consultant specialising in obesity medicine. This is particularly important if:
-
The prescriber cannot provide clear evidence supporting the combination
-
Adequate monitoring arrangements are not in place
-
The cost seems disproportionate or the source of medications is unclear
Patients should avoid purchasing weight-loss medicines, including phentermine/Duromine, from unregulated online sources, as these may be counterfeit, contaminated, or inappropriate for their medical condition.
Regular monitoring should include weight, blood pressure, heart rate, and assessment of comorbidities at intervals determined by the prescribing clinician, typically every 1–3 months initially.
Pregnant women or those planning pregnancy must not use either Saxenda or phentermine and should discuss alternative weight management strategies with their healthcare team. Both medications should be discontinued if pregnancy occurs.
Patients can access support through their GP, NHS specialist weight management services, or by self-referring to local tier 3 services where available. The NHS website (www.nhs.uk) provides information on local services and evidence-based weight management approaches.
Patients should report any suspected side effects from medications to the MHRA through the Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Is it safe to take Saxenda and Duromine together?
No, it is not safe to take Saxenda and Duromine (phentermine) together. There is no clinical evidence supporting this combination, and both medications can affect heart rate and blood pressure, potentially increasing cardiovascular risks.
Is phentermine (Duromine) available on the NHS in the UK?
No, phentermine (including branded versions such as Duromine) is not currently licensed by the MHRA for use in the UK and is not available on the NHS. Any use would be considered unlicensed and typically only available through private prescribing channels.
What are the evidence-based alternatives to combining weight loss medications?
Evidence-based alternatives include optimising single-agent pharmacotherapy such as Saxenda or Wegovy, using orlistat, implementing intensive lifestyle interventions with dietetic support, or considering bariatric surgery for eligible patients. NICE guidance recommends these approaches as part of comprehensive weight management programmes.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript