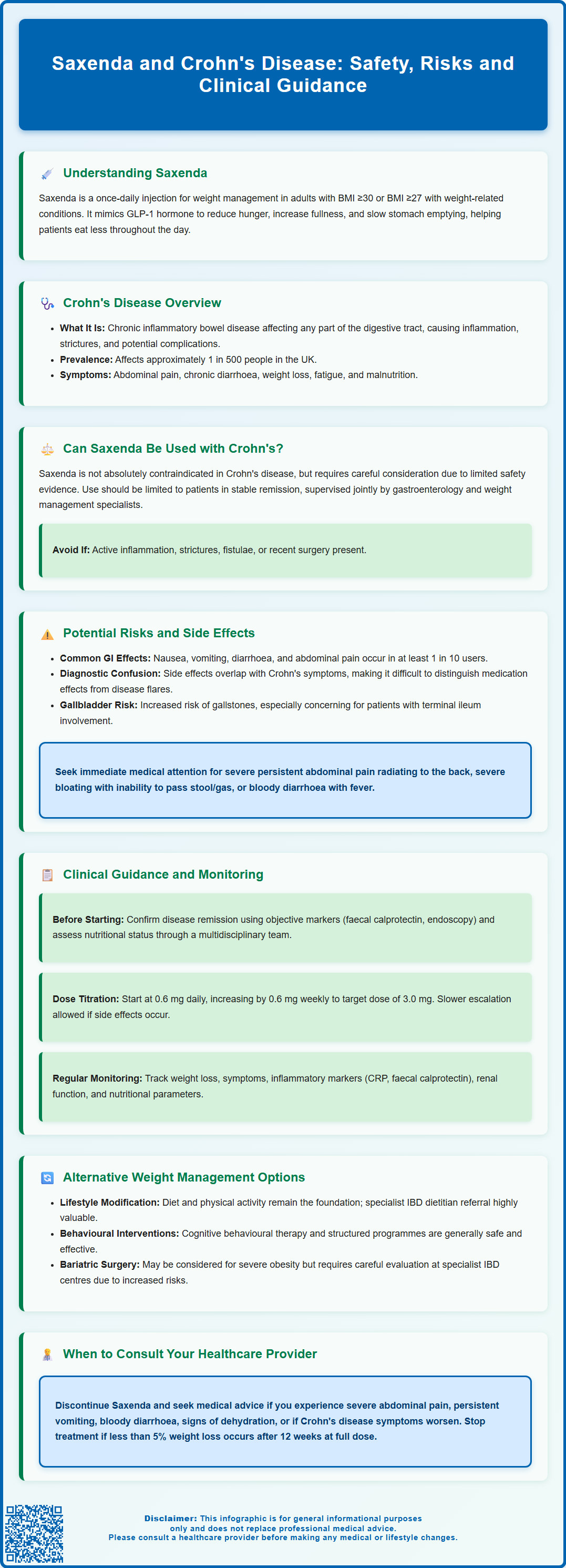
Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults and adolescents with obesity or overweight with comorbidities. For patients with Crohn's disease, the use of Saxenda requires careful consideration due to overlapping gastrointestinal side effects and the potential impact on disease activity. This article examines the safety, risks, and clinical guidance for using Saxenda in patients with Crohn's disease, alongside alternative weight management strategies suitable for this population.
Summary: Saxenda is not contraindicated in Crohn's disease but requires careful clinical consideration and should generally only be used in patients with stable remission under specialist supervision.
- Saxenda is a GLP-1 receptor agonist that slows gastric emptying and reduces appetite through hypothalamic GLP-1 receptor activation.
- Common gastrointestinal side effects include nausea, vomiting, diarrhoea, and abdominal pain, which overlap with Crohn's disease symptoms.
- The MHRA-approved SmPC advises caution in severe gastrointestinal disease but does not list inflammatory bowel disease as an absolute contraindication.
- Patients with active inflammation, strictures, fistulae, or recent surgery should generally avoid Saxenda until optimally controlled.
- Multidisciplinary assessment and ongoing monitoring of inflammatory markers and nutritional status are essential if Saxenda is prescribed.
- Alternative weight management options include specialist dietetic input, behavioural interventions, and consideration of bariatric surgery in selected cases.
Table of Contents
- Understanding Saxenda and Its Mechanism of Action
- Crohn's Disease: Overview and Gastrointestinal Considerations
- Can Saxenda Be Used Safely in Patients with Crohn's Disease?
- Potential Risks and Gastrointestinal Side Effects of Saxenda
- Clinical Guidance and Monitoring for Crohn's Patients Considering Saxenda
- Alternative Weight Management Options for Patients with Crohn's Disease
- Scientific References
- Frequently Asked Questions
Understanding Saxenda and Its Mechanism of Action
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as type 2 diabetes, hypertension, or dyslipidaemia. It is also licensed for weight management in adolescents aged 12-17 years with obesity. Saxenda is administered as a once-daily subcutaneous injection and is intended to be used alongside a reduced-calorie diet and increased physical activity.
Liraglutide belongs to a class of medications known as glucagon-like peptide-1 (GLP-1) receptor agonists. GLP-1 is a naturally occurring incretin hormone released from the intestine in response to food intake. By mimicking this hormone, Saxenda activates GLP-1 receptors in several key areas of the body, particularly in appetite-regulating centres such as the hypothalamus, where it reduces hunger and increases feelings of satiety.
Saxenda also slows gastric emptying, which prolongs the sensation of fullness after meals and contributes to reduced calorie intake. This effect on gastrointestinal motility is central to its weight-loss efficacy but also underlies some of its most common adverse effects.
The standard dosing begins at 0.6 mg daily, with weekly increases of 0.6 mg until reaching the maintenance dose of 3.0 mg daily. According to the Summary of Product Characteristics (SmPC), treatment should be discontinued if patients have not lost at least 5% of their initial body weight after 12 weeks on the 3.0 mg dose.
Important safety considerations include contraindications in pregnancy and breastfeeding, caution in patients with gallbladder disease or history of pancreatitis, and caution in those with severe gastrointestinal disease including gastroparesis. When used with insulin or sulfonylureas, dose adjustments of these medications may be needed to reduce the risk of hypoglycaemia.
While Saxenda is approved for use in the UK, NHS availability varies according to local commissioning decisions and formulary restrictions.
Crohn's Disease: Overview and Gastrointestinal Considerations
Crohn's disease is a chronic, relapsing inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract from the mouth to the anus, though it most commonly involves the terminal ileum and colon. It is characterised by transmural inflammation, meaning the inflammation extends through the entire thickness of the bowel wall, which can lead to complications such as strictures, fistulae, and abscesses. Symptoms typically include abdominal pain, chronic diarrhoea (which may be bloody), weight loss, fatigue, and malnutrition.
The aetiology of Crohn's disease is multifactorial, involving genetic susceptibility, environmental triggers, gut microbiota dysbiosis, and immune dysregulation. According to Crohn's & Colitis UK, the condition affects approximately 1 in 500 people in the UK, with diagnosis often occurring in young adulthood, though it can present at any age.
Management is guided by NICE guideline NG129 and focuses on inducing and maintaining remission, managing complications, and improving quality of life. Treatment options include corticosteroids, immunosuppressants (such as azathioprine or methotrexate), and biologic therapies (such as anti-TNF agents, anti-integrins, and IL-12/23 inhibitors). Aminosalicylates have a limited role in Crohn's disease management according to current UK guidance.
Some patients with Crohn's disease may experience altered gastrointestinal motility, though this varies considerably between individuals and disease states. The disease itself can affect nutritional status, with some patients experiencing weight loss due to malabsorption and reduced appetite during active disease, while others may gain weight during periods of remission or as a consequence of corticosteroid therapy. Any pharmacological intervention must be carefully considered in the context of the underlying inflammatory bowel condition and its potential impact on gastrointestinal function.
Can Saxenda Be Used Safely in Patients with Crohn's Disease?
The use of Saxenda in patients with Crohn's disease requires careful clinical consideration, as there is limited specific evidence regarding its safety and efficacy in this population. The Summary of Product Characteristics (SmPC) for Saxenda, as approved by the MHRA, does not list inflammatory bowel disease as an absolute contraindication. However, it does advise caution in patients with severe gastrointestinal disease, including gastroparesis, and does not provide specific guidance on use in patients with Crohn's disease.
The primary concern relates to Saxenda's gastrointestinal side effects, which are among the most common adverse reactions reported. These include nausea, vomiting, diarrhoea, constipation, and abdominal pain—symptoms that overlap significantly with those of active Crohn's disease. In a patient with Crohn's, it may be difficult to distinguish between disease flare, medication side effects, or complications such as obstruction or infection. This diagnostic uncertainty could potentially delay appropriate management of serious complications.
Furthermore, Saxenda's effect on gastric emptying may theoretically exacerbate symptoms in patients with pre-existing gastrointestinal dysmotility or stricturing disease. There is no official link established between Saxenda and worsening of Crohn's disease activity, but the overlapping symptom profile necessitates caution.
Based on clinical experience and expert opinion, Saxenda should generally only be considered in patients with Crohn's disease who are in stable remission, under the supervision of both gastroenterology and weight management specialists. Shared decision-making, with full discussion of potential risks and benefits, is essential.
As a precautionary approach, patients with active inflammation, strictures, fistulae, or recent surgery should generally avoid Saxenda until their condition is optimally controlled. Patients should be advised to stop the medication and seek urgent medical assessment if they experience severe abdominal pain, persistent vomiting, or symptoms suggestive of bowel obstruction or pancreatitis.
Potential Risks and Gastrointestinal Side Effects of Saxenda
Saxenda is associated with a range of gastrointestinal adverse effects, which according to the SmPC are very common (affecting ≥1/10 users). These include nausea, vomiting, diarrhoea, and constipation. Other common side effects (affecting ≥1/100 to <1/10 users) include dyspepsia and abdominal pain. These effects are generally dose-dependent and tend to diminish over time as tolerance develops, though some patients discontinue treatment due to persistent symptoms.
For patients with Crohn's disease, these side effects pose additional challenges. Nausea and vomiting can lead to reduced oral intake, potentially worsening nutritional status in individuals already at risk of malnutrition. Diarrhoea may be difficult to distinguish from a Crohn's flare, and persistent diarrhoea can lead to dehydration and electrolyte disturbances. Abdominal pain, a hallmark symptom of Crohn's, may be intensified or confused with medication side effects, complicating clinical assessment.
Gallbladder disorders, including cholelithiasis and cholecystitis, are also reported with Saxenda use. This is particularly relevant for patients with Crohn's disease affecting the terminal ileum, as they may already have an increased risk of gallstone formation due to disrupted bile salt metabolism.
There have been post-marketing reports of acute pancreatitis in patients taking GLP-1 receptor agonists, including liraglutide. Whilst the absolute risk is low, patients should be advised to seek immediate medical attention if they experience severe, persistent abdominal pain radiating to the back, accompanied by nausea and vomiting.
Another consideration is the potential for gastroparesis or severe delay in gastric emptying, which has been reported with GLP-1 agonists. This could theoretically increase the risk of bowel obstruction in patients with stricturing Crohn's disease. Patients should be advised to seek urgent medical care if they develop symptoms of obstruction such as severe abdominal distension, absolute constipation, or inability to pass flatus.
Other adverse effects include injection site reactions, headache, and increased heart rate. When used with insulin or sulfonylureas, there is an increased risk of hypoglycaemia, which may require dose adjustments of these medications.
Patients should be encouraged to report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Clinical Guidance and Monitoring for Crohn's Patients Considering Saxenda
If Saxenda is being considered for a patient with Crohn's disease, a comprehensive pre-treatment assessment is essential. This should include confirmation that the Crohn's disease is in clinical and biochemical remission, ideally supported by objective markers such as faecal calprotectin and, where appropriate, endoscopic or radiological evidence of mucosal healing. The patient's nutritional status, including BMI, micronutrient levels, and any history of malabsorption, should be thoroughly evaluated. A multidisciplinary approach involving gastroenterology, dietetics, and weight management specialists is strongly recommended.
Before initiating Saxenda, patients should be counselled about the expected gastrointestinal side effects and the importance of distinguishing these from symptoms of Crohn's disease activity. Clear safety-netting advice should be provided, including when to seek urgent medical attention—for example, if they experience severe abdominal pain, persistent vomiting, bloody diarrhoea, fever, abdominal distension, absolute constipation, or signs of dehydration. Patients should be advised to maintain adequate fluid intake.
The dose titration schedule should be followed carefully, starting at 0.6 mg daily and increasing by 0.6 mg weekly until reaching the 3.0 mg maintenance dose. For patients experiencing significant gastrointestinal side effects, slower titration may be considered to improve tolerability.
Women of childbearing potential should be advised to use contraception, as Saxenda is not recommended during pregnancy or breastfeeding. If a patient becomes pregnant while taking Saxenda, the medication should be discontinued.
Ongoing monitoring is crucial. Regular follow-up appointments should assess weight loss progress, tolerability of the medication, and any changes in Crohn's disease symptoms. Monitoring of inflammatory markers (such as C-reactive protein and faecal calprotectin) may help detect subclinical disease activity. Blood tests to assess renal function, electrolytes, and nutritional parameters should be performed periodically, particularly if gastrointestinal side effects are prominent.
According to the Saxenda SmPC, treatment should be discontinued if patients have not lost at least 5% of their initial body weight after 12 weeks on the 3.0 mg dose. In patients with Crohn's disease, the threshold for discontinuation should be lower if there is any suggestion of disease exacerbation or intolerable side effects. Patients should be empowered to stop the medication and seek medical advice if they have concerns about their symptoms.
Alternative Weight Management Options for Patients with Crohn's Disease
For patients with Crohn's disease who require weight management but for whom Saxenda is unsuitable or not tolerated, several alternative approaches should be considered. The cornerstone of weight management remains lifestyle modification, including dietary changes and increased physical activity tailored to the individual's capabilities and disease status. Referral to a specialist dietitian with expertise in inflammatory bowel disease is invaluable, as they can provide personalised advice that addresses both weight management and the nutritional challenges of Crohn's disease.
Other pharmacological options for weight management licensed in the UK include orlistat, which works by inhibiting pancreatic lipase and reducing fat absorption. However, orlistat commonly causes gastrointestinal side effects such as oily stools, faecal urgency, and flatulence, which may be poorly tolerated in patients with Crohn's disease, particularly those with diarrhoea-predominant symptoms.
Semaglutide (Wegovy), another GLP-1 receptor agonist, has been approved by NICE (TA875) for weight management in adults with at least one weight-related condition and a BMI of at least 35 kg/m² (or 32.5 kg/m² for people from certain ethnic groups), or a BMI of at least 30 kg/m² (or 27.5 kg/m² for people from certain ethnic groups) with exceptional specialist circumstances. However, it shares a similar side effect profile to Saxenda and would pose comparable concerns for patients with Crohn's disease.
For patients with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) who have not responded to non-surgical interventions, bariatric surgery may be considered in line with NICE guidance. However, the presence of Crohn's disease requires careful evaluation, as surgery carries additional risks in this population, including anastomotic complications, malabsorption, and potential exacerbation of inflammatory bowel disease. Procedures such as sleeve gastrectomy or gastric bypass should only be undertaken in specialist centres with experience in managing patients with IBD, and after thorough multidisciplinary discussion.
Behavioural interventions, including cognitive behavioural therapy and structured weight management programmes, can be effective and are generally safe for patients with Crohn's disease. Addressing psychological factors such as stress, anxiety, and depression—which are common in IBD patients—may also support weight management efforts. Ultimately, an individualised, holistic approach that prioritises both weight management goals and optimal control of Crohn's disease is essential for achieving the best outcomes.
Scientific References
Frequently Asked Questions
Is Saxenda safe for patients with Crohn's disease?
Saxenda is not contraindicated in Crohn's disease, but it should generally only be used in patients with stable remission under specialist supervision. The gastrointestinal side effects of Saxenda overlap with Crohn's symptoms, making careful monitoring essential.
What are the main risks of using Saxenda in Crohn's disease?
The main risks include difficulty distinguishing medication side effects from disease flare, potential worsening of gastrointestinal symptoms, and complications such as dehydration or malnutrition. Patients with active inflammation, strictures, or fistulae should avoid Saxenda.
What weight management alternatives exist for Crohn's disease patients?
Alternatives include specialist dietetic support, behavioural interventions, and lifestyle modification tailored to the individual's disease status. Bariatric surgery may be considered in selected cases with severe obesity, though it requires careful multidisciplinary evaluation in patients with inflammatory bowel disease.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript