Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities. Questions about Saxenda and breast cancer have emerged from preclinical studies and post-marketing surveillance. However, current clinical evidence does not establish a causal link between Saxenda use and increased breast cancer risk in humans. This article examines the available evidence, considerations for patients with breast cancer history, and essential safety monitoring for those prescribed Saxenda under NHS specialist weight management services.
Summary: Current clinical evidence does not establish a causal relationship between Saxenda (liraglutide) use and increased breast cancer risk in humans.
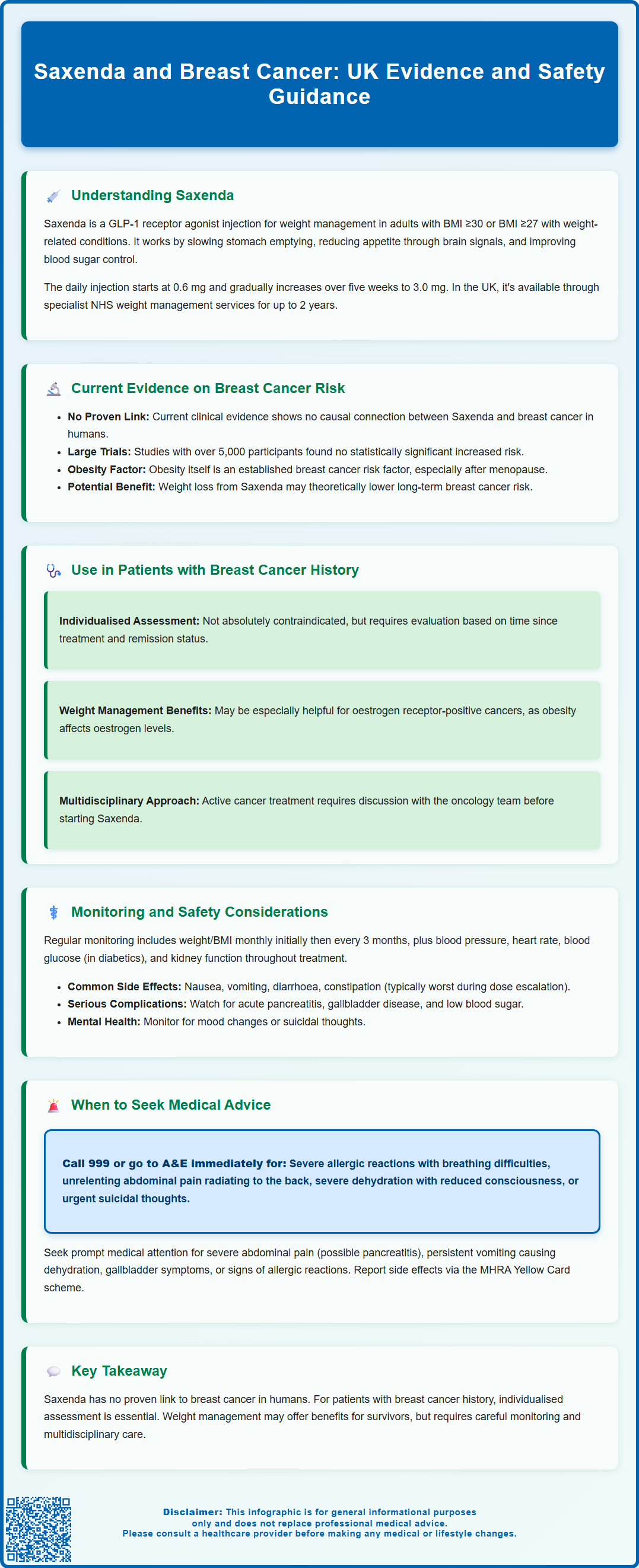
- Saxenda is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities.
- Large-scale clinical trials and real-world data have not demonstrated a statistically significant increased breast cancer risk with liraglutide.
- Previous breast cancer is not an absolute contraindication, but requires individualised assessment and multidisciplinary discussion.
- Patients require regular monitoring including weight, cardiovascular parameters, renal function, and assessment for pancreatitis and thyroid symptoms.
- Under NICE guidance, Saxenda is available only through NHS specialist weight management services for a maximum of 2 years.
- Treatment should be discontinued if patients have not lost at least 5% of initial body weight after 12 weeks on the 3.0 mg daily dose.
Table of Contents
Understanding Saxenda and Its Primary Uses
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity or those who are overweight with weight-related health conditions. It is also licensed for adolescents aged 12-17 years with body weight above 60 kg and obesity. Saxenda belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which were originally developed for type 2 diabetes management.
The mechanism of action involves mimicking the naturally occurring hormone GLP-1, which is released from the intestine after eating. Saxenda works by:
-
Slowing gastric emptying, which helps you feel fuller for longer after meals
-
Reducing appetite through effects on brain regions that regulate hunger
-
Improving blood sugar control by enhancing insulin secretion when glucose levels are elevated
Saxenda is administered as a once-daily subcutaneous injection, typically starting at a low dose (0.6 mg) and gradually increasing over five weeks to the maintenance dose of 3.0 mg daily.
The medication is indicated for adults with a body mass index (BMI) of 30 kg/m² or greater, or those with a BMI of 27 kg/m² or greater who have at least one weight-related comorbidity such as hypertension, type 2 diabetes, dyslipidaemia, or obstructive sleep apnoea.
Under NHS guidance (NICE TA664), Saxenda is only available through specialist weight management services (tier 3 or 4) for a maximum duration of 2 years, and patients must meet specific eligibility criteria.
Treatment should be discontinued if patients have not lost at least 5% of their initial body weight after 12 weeks on the 3.0 mg daily dose. Saxenda is not licensed for use in pregnant or breastfeeding women.
Current Evidence on Saxenda and Breast Cancer Risk
Concerns about a potential link between Saxenda and breast cancer have emerged from both preclinical studies and post-marketing surveillance data. However, there is currently no established causal relationship between liraglutide use and increased breast cancer risk in humans based on available clinical evidence.
In preclinical rodent studies, some GLP-1 receptor agonists have been associated with thyroid C-cell tumours. The UK SmPC notes these rodent findings but indicates that their relevance to humans remains uncertain due to species-specific differences in GLP-1 receptor distribution. The SmPC advises vigilance for thyroid symptoms, but does not list a specific contraindication related to thyroid cancer history.
Regarding breast cancer specifically, large-scale clinical trials and real-world data analyses have not demonstrated a statistically significant increased risk. The SCALE (Satiety and Clinical Adiposity – Liraglutide Evidence) clinical trial programme, which included over 5,000 participants treated with liraglutide 3.0 mg, did not identify breast cancer as a safety signal. Post-marketing pharmacovigilance data collected by the MHRA and EMA continue to monitor for any emerging safety concerns, as very long-term cancer risk data remain limited.
It is worth noting that obesity itself is an established risk factor for breast cancer, particularly in postmenopausal women. The relationship between body weight and breast cancer risk is complex, involving hormonal mechanisms including increased oestrogen production in adipose tissue. Therefore, weight loss achieved through Saxenda treatment may theoretically reduce long-term breast cancer risk, though this potential benefit requires further investigation through long-term epidemiological studies. Patients with concerns about cancer risk should discuss their individual circumstances with their healthcare provider.
Saxenda Use in Patients with a History of Breast Cancer
The use of Saxenda in patients with a previous diagnosis of breast cancer requires careful individualised assessment. The Summary of Product Characteristics (SmPC) for Saxenda does not list previous breast cancer as an absolute contraindication, but clinical judgement must consider the patient's overall health status, cancer treatment history, and current disease status.
Key considerations for healthcare professionals include:
-
Time since diagnosis and treatment completion – patients who have completed treatment and are in remission may be considered differently from those with active disease
-
Hormone receptor status of the previous breast cancer – as obesity affects oestrogen levels, weight management may be particularly relevant for oestrogen receptor-positive cancers
-
Current medications – while no specific interactions with tamoxifen or aromatase inhibitors are established, review all medicines due to potential effects on oral drug absorption
-
Overall cardiovascular and metabolic health – many breast cancer survivors have additional comorbidities that may benefit from weight management
For patients in active breast cancer treatment, the decision to initiate Saxenda should involve multidisciplinary discussion with the oncology team. Weight management during cancer treatment is complex, as some patients experience weight gain (particularly with certain chemotherapy regimens or hormonal therapies), whilst others may experience weight loss.
The potential benefits of weight loss in breast cancer survivors include improved cardiovascular and metabolic health and better quality of life. While some evidence suggests weight loss may be associated with reduced cancer recurrence risk, this evidence remains uncertain and is still under investigation. These potential benefits must be weighed against any theoretical risks and the individual patient's circumstances. Shared decision-making between the patient, GP, and specialist teams is essential to determine whether Saxenda is an appropriate option within a comprehensive weight management strategy.
Monitoring and Safety Considerations
Patients prescribed Saxenda require regular monitoring to ensure both efficacy and safety throughout treatment. Healthcare professionals should establish a structured follow-up schedule that addresses both weight management outcomes and potential adverse effects.
Routine monitoring should include:
-
Weight and BMI measurements at baseline and regularly (typically monthly initially, then every 3 months)
-
Blood pressure and heart rate – as Saxenda can cause modest increases in heart rate
-
Blood glucose levels in patients with diabetes or prediabetes
-
Renal function tests – particularly in patients with existing kidney disease or those experiencing significant gastrointestinal side effects that could cause dehydration
-
Assessment for signs of pancreatitis – patients should be counselled about symptoms such as severe, persistent abdominal pain
-
Mental health assessment – monitor for mood changes or suicidal thoughts, which are rare but important safety concerns noted in the UK SmPC
-
Thyroid symptoms – be vigilant for persistent neck swelling, hoarseness or other thyroid-related symptoms
Common adverse effects that patients should be aware of include:
-
Gastrointestinal symptoms (nausea, vomiting, diarrhoea, constipation) – usually most prominent during dose escalation
-
Injection site reactions
-
Headache and dizziness
-
Fatigue
More serious but rare adverse effects include acute pancreatitis, gallbladder disease, and hypoglycaemia (particularly in patients taking other glucose-lowering medications). Patients should report suspected side effects via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
For patients with a history of breast cancer or those concerned about cancer risk, it may be prudent to ensure they maintain regular breast screening according to NHS guidelines and attend routine oncology follow-up appointments as scheduled. Any new breast symptoms (lumps, skin changes, nipple discharge) should be reported promptly, though these would warrant investigation regardless of Saxenda use. Documentation of the risk-benefit discussion in the patient's medical records is essential for continuity of care.
When to Seek Medical Advice
Patients using Saxenda should be clearly informed about circumstances that require prompt medical attention. Whilst most side effects are mild and self-limiting, certain symptoms warrant urgent assessment.
Contact your GP or healthcare provider promptly if you experience:
-
Severe abdominal pain that does not resolve – this may indicate pancreatitis, particularly if accompanied by nausea and vomiting
-
Persistent nausea or vomiting that prevents adequate fluid intake, risking dehydration
-
Signs of gallbladder problems – pain in the upper right abdomen, fever, yellowing of skin or eyes
-
Symptoms of low blood sugar (if taking other diabetes medications) – shakiness, confusion, sweating, rapid heartbeat
-
Unexplained rapid heart rate or palpitations
-
Signs of allergic reaction – rash, itching, swelling, difficulty breathing
-
New or worsening depression, thoughts of self-harm or suicide
-
Persistent neck swelling, hoarseness or difficulty swallowing
Contact NHS 111 for urgent advice when your GP is unavailable, or seek immediate medical attention (call 999 or attend A&E) if you develop:
-
Severe allergic reactions with breathing difficulties or facial swelling
-
Severe, unrelenting abdominal pain radiating to the back
-
Signs of severe dehydration with reduced consciousness
-
Suicidal thoughts requiring immediate support
For patients with breast cancer history, contact your GP or breast care team if you notice:
-
Any new breast lumps or changes in breast tissue
-
Nipple discharge, particularly if blood-stained
-
Skin changes on the breast (dimpling, redness, or puckering)
-
Changes in breast size or shape
These symptoms require investigation regardless of Saxenda use, but patients should feel empowered to report any concerns. Additionally, if you are not achieving adequate weight loss (less than 5% after 12 weeks on the 3.0 mg dose), discuss this with your prescriber, as continuing treatment may not be appropriate. Do not stop Saxenda without speaking to your prescriber, particularly if you have diabetes, as this may affect your blood sugar control. Regular communication with your healthcare team ensures optimal safety and treatment outcomes.
Frequently Asked Questions
Does Saxenda increase the risk of breast cancer?
Current clinical evidence does not demonstrate a statistically significant increased risk of breast cancer with Saxenda use. Large-scale trials and post-marketing surveillance by the MHRA and EMA have not identified breast cancer as a safety signal, though very long-term data remain limited.
Can I use Saxenda if I have had breast cancer previously?
Previous breast cancer is not an absolute contraindication to Saxenda, but requires careful individualised assessment. The decision should involve multidisciplinary discussion with your GP and oncology team, considering factors such as time since diagnosis, treatment completion status, and overall health.
What monitoring is required when taking Saxenda?
Regular monitoring includes weight and BMI measurements, blood pressure, heart rate, blood glucose (if diabetic), renal function, and assessment for signs of pancreatitis, thyroid symptoms, and mental health changes. Patients should also maintain routine NHS breast screening and report any new breast symptoms promptly.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










