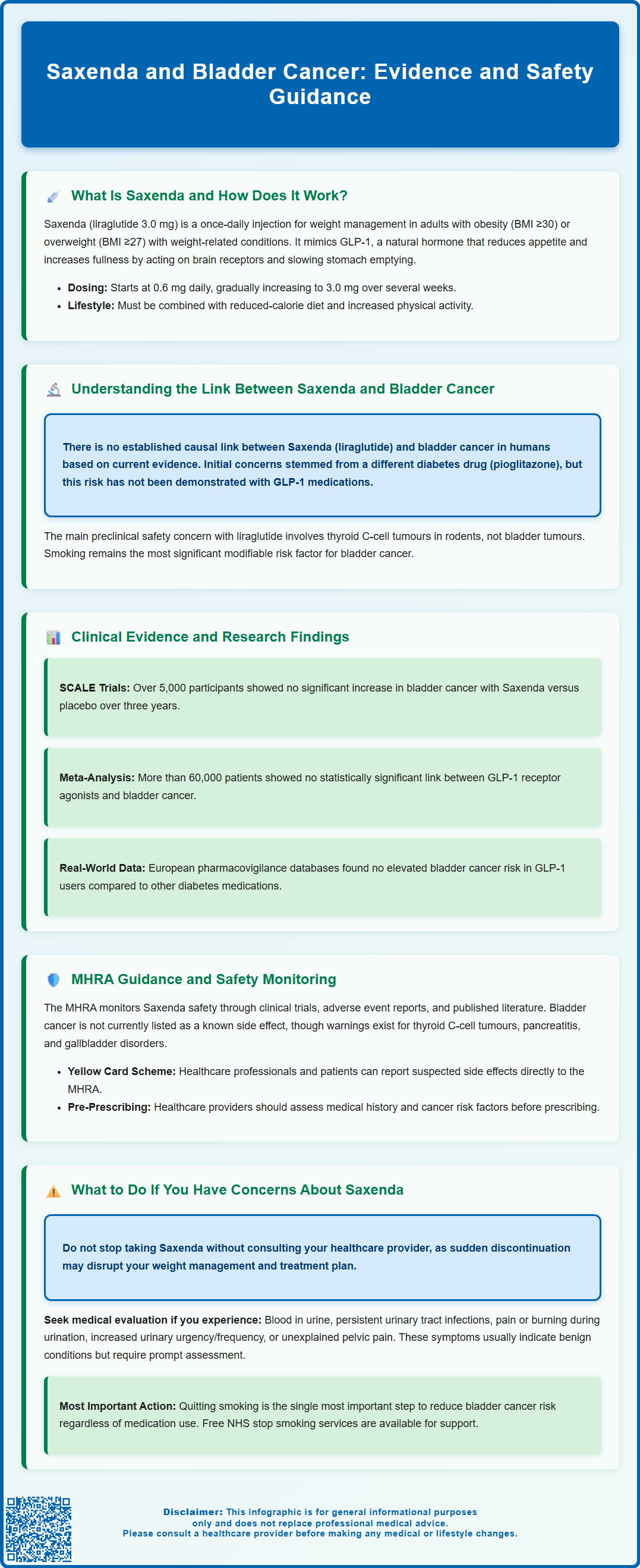
Saxenda and bladder cancer concerns have emerged in discussions about GLP-1 receptor agonist safety, prompting questions from patients and healthcare professionals. Saxenda (liraglutide 3.0 mg) is a prescription weight management medicine licensed in the UK for adults with obesity or overweight with comorbidities, and for adolescents aged 12–17 years with obesity. Whilst regulatory monitoring continues, current evidence does not establish a causal link between Saxenda and bladder cancer. This article examines the available clinical data, MHRA guidance, and practical advice for patients considering or currently using this treatment.
Summary: Current evidence does not establish a causal link between Saxenda (liraglutide) and bladder cancer in humans.
- Saxenda is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities, and adolescents with obesity.
- Large-scale clinical trials and meta-analyses involving over 60,000 patients show no statistically significant association between GLP-1 receptor agonists and bladder cancer.
- The MHRA Summary of Product Characteristics for Saxenda does not list bladder cancer as a known or suspected adverse reaction.
- Patients experiencing unexplained haematuria, persistent urinary symptoms, or pelvic pain should seek prompt medical evaluation regardless of medication use.
- Smoking remains the most significant modifiable risk factor for bladder cancer, and cessation support is recommended for all patients.
Table of Contents
What Is Saxenda and How Does It Work?
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as type 2 diabetes, hypertension, or dyslipidaemia. It is also licensed for weight management in adolescents aged 12 to <18 years with body weight above 60 kg and obesity. Saxenda is administered as a once-daily subcutaneous injection and is intended to be used alongside a reduced-calorie diet and increased physical activity.
The active ingredient, liraglutide, belongs to a class of medicines called glucagon-like peptide-1 (GLP-1) receptor agonists. GLP-1 is a naturally occurring hormone released by the intestine in response to food intake. Liraglutide mimics this hormone by binding to GLP-1 receptors in the brain, particularly in areas that regulate appetite and food intake. This action leads to increased feelings of fullness (satiety), reduced hunger, and consequently lower calorie consumption.
In addition to its effects on appetite, liraglutide slows gastric emptying, which prolongs the sensation of fullness after meals. It also influences insulin secretion in a glucose-dependent manner, meaning it has a low risk of causing hypoglycaemia when used alone, though this risk increases when used with insulin or sulfonylureas. These combined mechanisms support gradual, sustained weight loss when used as part of a comprehensive weight management programme.
Saxenda is typically initiated at a low dose (0.6 mg daily) and gradually increased over several weeks to the maintenance dose of 3.0 mg daily. This titration schedule helps minimise common gastrointestinal side effects such as nausea, vomiting, and diarrhoea. Treatment should be discontinued if patients do not achieve at least 5% weight loss after 12 weeks on the 3.0 mg daily dose. For adolescents, treatment should be discontinued and re-evaluated if body weight has not decreased by at least 4% BMI after 12 weeks on the 3.0 mg dose.
Understanding the Link Between Saxenda and Bladder Cancer
Concerns about a potential association between GLP-1 receptor agonists and bladder cancer have emerged primarily from post-marketing surveillance data. It is important to emphasise that there is no established causal link between Saxenda (liraglutide) and bladder cancer in humans based on current evidence. However, regulatory authorities and researchers continue to monitor this potential safety signal carefully.
The concern initially arose from studies involving another diabetes medication, pioglitazone (a thiazolidinedione), which showed an increased risk of bladder cancer in some populations. Subsequently, attention turned to other glucose-lowering agents, including GLP-1 receptor agonists. It's important to note that the bladder cancer risk associated with pioglitazone has not been demonstrated with GLP-1 receptor agonists based on current evidence. The main preclinical safety signal with liraglutide relates to thyroid C-cell tumours in rodents, not bladder tumours.
In clinical practice, bladder cancer is relatively uncommon, with an incidence of approximately 20 cases per 100,000 people per year in the UK, according to Cancer Research UK. Risk factors include smoking (the most significant modifiable risk factor), occupational exposure to certain chemicals (such as aromatic amines), chronic bladder inflammation, and increasing age. Some studies suggest obesity itself may be associated with a modest increase in bladder cancer risk, which complicates the interpretation of any potential drug-related effects.
Patients prescribed Saxenda should be aware that regulatory bodies have not identified a definitive increased risk of bladder cancer with liraglutide use. Nonetheless, healthcare professionals are advised to remain vigilant for any urological symptoms and to consider individual patient risk factors when prescribing weight management therapies.
Clinical Evidence and Research Findings
The SCALE (Satiety and Clinical Adiposity – Liraglutide Evidence) clinical trial programme represents the most comprehensive evaluation of Saxenda's safety and efficacy. These randomised controlled trials involved over 5,000 participants followed for up to three years. In these trials, no significant increase in bladder cancer incidence was observed in patients treated with liraglutide 3.0 mg compared to placebo, though specific event numbers were small, as would be expected for a rare condition.
A large-scale meta-analysis published in Diabetes, Obesity and Metabolism examined cardiovascular and cancer outcomes across multiple GLP-1 receptor agonist trials. The analysis included data from more than 60,000 patients and found no statistically significant association between GLP-1 receptor agonist use and bladder cancer. The overall cancer incidence was similar between treatment and control groups, providing reassurance about the safety profile of this drug class.
Real-world evidence from pharmacovigilance databases and population-based cohort studies has similarly failed to demonstrate a clear link between liraglutide and bladder malignancy. European observational studies comparing GLP-1 receptor agonist users with other antidiabetic medication users found no elevated risk of bladder cancer after adjusting for confounding factors such as smoking, age, and diabetes duration.
However, researchers acknowledge that long-term safety data beyond five years remain limited, and rare adverse events may only become apparent with extended post-marketing surveillance. Ongoing pharmacoepidemiological studies continue to monitor cancer outcomes in patients prescribed Saxenda and other GLP-1 receptor agonists.
It is worth noting that the benefits of clinically significant weight loss—including reduced cardiovascular risk, improved glycaemic control, and enhanced quality of life—must be weighed against theoretical or unproven risks when making treatment decisions.
MHRA Guidance and Safety Monitoring
The Medicines and Healthcare products Regulatory Agency (MHRA) is responsible for monitoring the safety of all medicines used in the UK, including Saxenda. The MHRA continuously reviews emerging safety data from clinical trials, spontaneous adverse event reports, and published literature to ensure that the benefits of licensed medicines outweigh their risks.
Currently, the Summary of Product Characteristics (SmPC) for Saxenda does not list bladder cancer as a known or suspected adverse reaction. The product information does, however, include warnings about other potential risks, including thyroid C-cell tumours (based on rodent studies). The SmPC contains a warning that liraglutide causes dose-dependent and treatment-duration-dependent thyroid C-cell tumours in rodents, though the human relevance of this finding is unknown. Other warnings include pancreatitis, gallbladder disorders, and hypoglycaemia when used with certain other medications.
Healthcare professionals prescribing Saxenda are advised to conduct a thorough medical history assessment, including evaluation of cancer risk factors, before initiating treatment. Patients should be counselled about potential side effects and advised to report any unusual symptoms promptly. The MHRA recommends that prescribers remain vigilant for signs and symptoms that may indicate serious adverse reactions.
The Yellow Card Scheme enables healthcare professionals and patients to report suspected side effects directly to the MHRA via yellowcard.mhra.gov.uk or the Yellow Card app. This spontaneous reporting system is a vital component of post-marketing surveillance, helping to identify previously unrecognised safety signals.
Regular safety reviews ensure that product information remains current and that any necessary risk minimisation measures are implemented promptly. Patients can access the most up-to-date safety information through the MHRA website or by consulting their healthcare provider.
What to Do If You Have Concerns About Saxenda
If you are currently taking Saxenda and have concerns about bladder cancer or any other potential side effects, do not stop your medication abruptly without first consulting your prescribing healthcare professional. Sudden discontinuation may affect your weight management progress and overall treatment plan.
Contact your GP or specialist if you experience any of the following symptoms, which may warrant further investigation:
-
Visible blood in your urine (haematuria) without infection or that persists/recurs after treatment
-
Persistent or recurrent urinary tract infections
-
Pain or burning sensation when urinating (dysuria)
-
Increased urgency or frequency of urination without an obvious cause
-
Lower abdominal or pelvic pain that does not resolve
These symptoms are not specific to bladder cancer and are more commonly caused by benign conditions such as urinary tract infections or bladder stones. However, they should always be evaluated promptly, particularly in individuals with additional risk factors such as smoking history or occupational chemical exposure.
Your healthcare provider may arrange appropriate investigations, which could include urinalysis, urine microscopy and culture, blood tests, and possibly ultrasound of the renal tract. According to NICE guidance (NG12), urgent referral (within two weeks) is recommended for suspected bladder cancer in patients aged 45 and over with unexplained visible haematuria without urinary tract infection or that persists/recurs after treatment, or aged 60 and over with unexplained non-visible haematuria and either dysuria or a raised white cell count on blood tests. A specialist may then arrange cystoscopy (a procedure to examine the inside of the bladder).
Lifestyle modifications remain crucial for reducing bladder cancer risk, regardless of medication use. If you smoke, accessing smoking cessation support is the single most important step you can take. The NHS offers free stop smoking services, including behavioural support and pharmacotherapy.
Finally, maintain open communication with your healthcare team about any concerns. Your prescriber can provide personalised advice based on your individual medical history, risk factors, and treatment goals, ensuring that your weight management strategy remains both safe and effective.
Frequently Asked Questions
Does Saxenda increase the risk of bladder cancer?
Current evidence from large clinical trials and meta-analyses does not demonstrate an increased risk of bladder cancer with Saxenda (liraglutide) use. Regulatory authorities continue to monitor safety data, but no causal link has been established.
What symptoms should I watch for whilst taking Saxenda?
Contact your GP if you experience visible blood in urine, persistent urinary tract infections, pain or burning when urinating, increased urgency or frequency of urination, or unexplained lower abdominal pain. These symptoms warrant prompt medical evaluation.
Should I stop taking Saxenda if I'm worried about bladder cancer?
Do not stop Saxenda without consulting your prescribing healthcare professional. Discuss any concerns with your GP or specialist, who can provide personalised advice based on your individual medical history and risk factors.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript