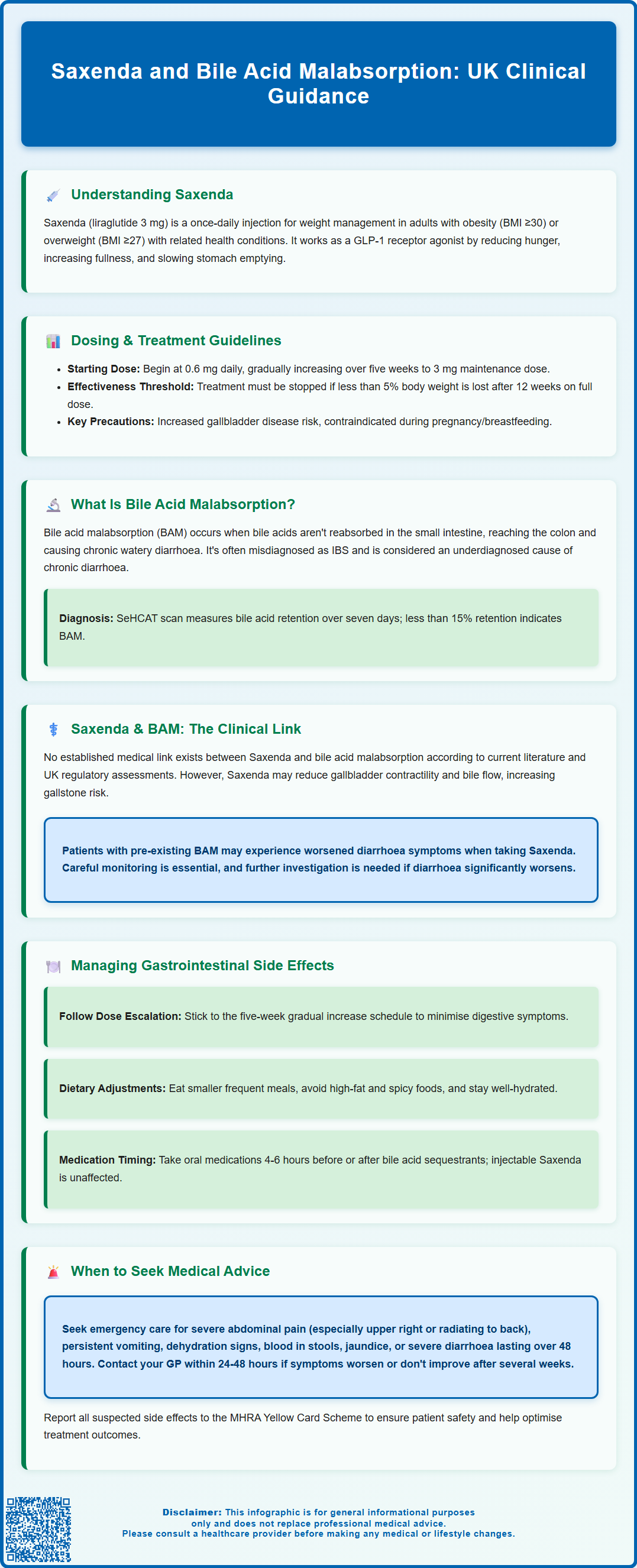
Saxenda (liraglutide 3 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities. Bile acid malabsorption (BAM) is a condition causing chronic diarrhoea due to impaired bile acid reabsorption in the terminal ileum. Patients considering Saxenda may wonder whether this medication could affect or worsen BAM. This article examines the relationship between Saxenda and bile acid malabsorption, exploring mechanisms of action, potential interactions, and practical guidance for patients with existing gastrointestinal conditions seeking weight management support.
Summary: There is no established link between Saxenda (liraglutide) and the development or worsening of bile acid malabsorption in current medical literature or UK regulatory assessments.
- Saxenda is a GLP-1 receptor agonist that slows gastric emptying and reduces appetite, licensed for weight management in adults with obesity or overweight with comorbidities.
- Bile acid malabsorption causes chronic diarrhoea when bile acids are not reabsorbed in the terminal ileum; diagnosis typically uses SeHCAT scanning with retention <15% considered abnormal.
- Common gastrointestinal side effects of Saxenda include nausea (40% of patients) and diarrhoea (15-20%), typically occurring during initial treatment and dose escalation.
- Patients with pre-existing bile acid malabsorption should discuss Saxenda use with their GP or specialist and maintain careful monitoring during treatment initiation.
- Seek urgent medical attention for severe abdominal pain, persistent vomiting, signs of dehydration, jaundice, or blood in stools whilst taking Saxenda.
Table of Contents
Understanding Saxenda and Its Mechanism of Action
Saxenda (liraglutide 3 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with weight-related comorbidities such as type 2 diabetes, hypertension, or dyslipidaemia. It is administered as a once-daily subcutaneous injection and is intended for use alongside a reduced-calorie diet and increased physical activity.
Liraglutide belongs to a class of medications known as glucagon-like peptide-1 (GLP-1) receptor agonists. It works by mimicking the action of the naturally occurring hormone GLP-1, which is released from the intestine in response to food intake. The mechanism of action involves several pathways that contribute to weight loss. Firstly, liraglutide acts on receptors in the brain's appetite centres, particularly in the hypothalamus, to reduce hunger and increase feelings of fullness (satiety). Secondly, it slows gastric emptying, meaning food remains in the stomach for longer, which prolongs the sensation of fullness after meals. Additionally, liraglutide helps regulate blood glucose levels by stimulating insulin secretion when blood sugar is elevated and suppressing glucagon release.
The MHRA approved Saxenda following clinical trials demonstrating significant weight loss compared to placebo when combined with lifestyle interventions. Patients typically start on a low dose (0.6 mg daily) and gradually increase over five weeks to the maintenance dose of 3 mg daily. This titration schedule helps minimise gastrointestinal side effects, which are among the most commonly reported adverse reactions.
Important safety considerations include:
-
Treatment should be discontinued if at least 5% weight loss has not been achieved after 12 weeks on the 3 mg dose
-
Saxenda increases the risk of gallbladder disease and should be used with caution in patients with existing gallbladder conditions
-
Patients with a history of pancreatitis require careful monitoring
-
Saxenda should not be used during pregnancy or breastfeeding, and women of childbearing potential should use contraception
-
The delayed gastric emptying effect may affect absorption of some oral medicines
In the NHS, Saxenda is typically available through specialist weight management services according to NICE criteria, which may differ from the licensed indications.
What Is Bile Acid Malabsorption and How Is It Diagnosed?
Bile acid malabsorption (BAM), also known as bile acid diarrhoea, is a condition in which bile acids are not properly reabsorbed in the terminal ileum and instead pass into the colon. Bile acids are produced by the liver, stored in the gallbladder, and released into the small intestine to aid fat digestion. Normally, approximately 95% of bile acids are reabsorbed in the distal ileum and recycled back to the liver. When this reabsorption process is impaired, excess bile acids reach the colon, where they stimulate water and electrolyte secretion, leading to chronic watery diarrhoea.
BAM is classified into three types: Type 1 occurs due to ileal disease or resection (such as in Crohn's disease); Type 2 is idiopathic, with no identifiable underlying cause; and Type 3 is secondary to other gastrointestinal conditions, including post-cholecystectomy, coeliac disease, or chronic pancreatitis. Many patients with BAM are initially misdiagnosed with irritable bowel syndrome (IBS), as the symptoms overlap considerably.
Diagnosis of BAM in the UK typically involves the SeHCAT (selenium homocholic acid taurine) scan, a nuclear medicine test that measures bile acid retention over seven days. According to British Society of Gastroenterology (BSG) guidance, a retention value of less than 15% at 7 days is considered abnormal, with severity classified as: mild (10-15%), moderate (5-10%), and severe (<5%). However, SeHCAT availability varies across NHS trusts.
Alternative diagnostic approaches include blood tests measuring 7α-hydroxy-4-cholesten-3-one (C4), a marker of bile acid synthesis, though these are not yet widely available. When objective testing is unavailable, therapeutic trials of bile acid sequestrants (such as colestyramine or colesevelam) may be considered, with symptomatic improvement supporting the diagnosis, though this approach has limitations in specificity.
The diagnostic workup for chronic diarrhoea should also include other investigations such as coeliac serology, faecal calprotectin to exclude inflammatory bowel disease, stool tests, and age-appropriate colorectal assessment before or alongside BAM testing. The BSG chronic diarrhoea guideline recognises BAM as an important and potentially underdiagnosed cause of chronic diarrhoea that should be considered in patients with persistent symptoms.
Can Saxenda Cause or Worsen Bile Acid Malabsorption?
There is no established link between Saxenda (liraglutide) and the development or worsening of bile acid malabsorption in current medical literature, the Saxenda Summary of Product Characteristics (SmPC), or regulatory assessments from the MHRA or EMA. However, understanding the potential interaction requires consideration of how GLP-1 receptor agonists affect gastrointestinal function and bile acid metabolism.
Saxenda's mechanism of slowing gastric emptying and altering gut motility could theoretically influence bile acid dynamics. Some research suggests that GLP-1 receptor agonists may affect gallbladder function, potentially reducing gallbladder contractility and bile flow. This has been associated with an increased risk of cholelithiasis (gallstones) and cholecystitis in some patients, as noted in the Saxenda SmPC. It's worth noting that rapid weight loss itself, regardless of method, can also increase the risk of gallstone formation. However, the direct impact of liraglutide on bile acid reabsorption in the terminal ileum remains unclear and is not well documented in clinical studies.
The most commonly reported gastrointestinal side effects of Saxenda include nausea, diarrhoea, constipation, vomiting, and abdominal pain. These occur in a significant proportion of patients, particularly during dose escalation. Diarrhoea associated with Saxenda is generally attributed to the drug's effects on gut motility and gastric emptying rather than bile acid malabsorption. However, in patients with pre-existing BAM, the additional gastrointestinal effects of Saxenda could potentially exacerbate diarrhoeal symptoms, making symptom management more challenging.
For patients with known or suspected bile acid malabsorption who are considering Saxenda for weight management, it is important to discuss this with their GP or specialist. Careful monitoring during treatment initiation and dose escalation is advisable. If diarrhoea worsens significantly or becomes difficult to manage, further investigation may be warranted to distinguish between Saxenda-related side effects and progression of underlying BAM. Healthcare professionals should maintain a high index of suspicion and consider alternative weight management strategies if gastrointestinal symptoms prove intolerable or if there is clinical concern about worsening malabsorption.
Managing Gastrointestinal Side Effects When Using Saxenda
Gastrointestinal side effects are the most frequently reported adverse reactions with Saxenda. According to the SmPC, nausea affects approximately 40% of patients, while diarrhoea, constipation and vomiting each affect 15-20% of patients in clinical trials. Effective management of these symptoms is crucial for treatment adherence and achieving weight loss goals. Nausea and diarrhoea typically occur during the initial weeks of treatment and often improve as the body adjusts to the medication.
Practical strategies to minimise gastrointestinal symptoms include:
-
Gradual dose escalation: Following the recommended five-week titration schedule allows the digestive system to adapt. Patients should not rush to increase the dose if experiencing significant symptoms.
-
Dietary modifications: Eating smaller, more frequent meals rather than large portions can reduce nausea. Avoiding high-fat, spicy, or heavily processed foods may help, as these can exacerbate gastrointestinal discomfort. Staying well-hydrated is essential, particularly if experiencing diarrhoea.
-
Timing of injection: Some patients may find that administering Saxenda at a consistent time each day helps manage symptoms. Evening administration is an option some patients find helpful for managing daytime nausea, though this should be individualised based on personal response.
-
Monitoring symptom patterns: Keeping a symptom diary can help identify triggers and patterns, which can be discussed with healthcare providers.
For patients with pre-existing bile acid malabsorption, additional considerations apply. If already taking bile acid sequestrants such as colestyramine or colesevelam, these should be continued as prescribed. However, it is important to note that bile acid sequestrants can potentially interfere with the absorption of other medications. According to the BNF, other oral medicines should generally be taken at least 4-6 hours before or after bile acid sequestrants. Saxenda (being an injectable medication) is not affected by this interaction. Patients should consult their pharmacist for specific timing advice for their medications.
Patients with diabetes who are taking insulin or sulfonylureas may need dose adjustments of these medications when starting Saxenda, as there is an increased risk of hypoglycaemia.
If gastrointestinal symptoms persist beyond the first few weeks, are severe, or significantly impact quality of life, patients should consult their prescribing clinician. Dose reduction or temporary treatment interruption may be necessary. In some cases, symptomatic treatment with anti-emetics for nausea or loperamide for diarrhoea may be considered, though this should be discussed with a healthcare professional.
When to Seek Medical Advice: Recognising Serious Symptoms
Whilst many gastrointestinal side effects of Saxenda are mild to moderate and self-limiting, certain symptoms warrant prompt medical attention. Patients should be educated about red flag symptoms that may indicate serious complications requiring urgent assessment.
Seek immediate medical advice or attend A&E if experiencing:
-
Severe, persistent abdominal pain, particularly if localised to the upper right quadrant or radiating to the back, which could indicate pancreatitis, cholecystitis, or gallstone complications
-
Persistent vomiting that prevents adequate fluid or medication intake, leading to dehydration
-
Signs of dehydration, including reduced urine output, dark urine, dizziness, confusion, or rapid heartbeat, particularly if accompanied by severe diarrhoea
-
Blood in stools or black, tarry stools, which may indicate gastrointestinal bleeding
-
Jaundice (yellowing of the skin or whites of the eyes), very pale stools and dark urine, which may indicate biliary obstruction
-
Severe or persistent diarrhoea lasting more than 48 hours, especially with fever, blood, or signs of dehydration
-
Symptoms of acute pancreatitis, such as severe upper abdominal pain radiating to the back, nausea, vomiting, and fever
Contact your GP or prescribing clinician within 24-48 hours if:
-
Gastrointestinal symptoms worsen significantly or do not improve after several weeks of treatment
-
You experience unexplained weight loss beyond expected therapeutic effects, or symptoms of malabsorption such as steatorrhoea (pale, floating, foul-smelling stools)
-
Diarrhoea becomes chronic and interferes with daily activities or quality of life
-
You have concerns about interactions with existing conditions, particularly known bile acid malabsorption or other gastrointestinal disorders
For patients with pre-existing bile acid malabsorption, it is particularly important to maintain regular follow-up with healthcare providers. Any significant change in bowel habit patterns or worsening of previously controlled symptoms should be reported promptly. Healthcare professionals may need to reassess the diagnosis, optimise bile acid sequestrant therapy, or consider whether Saxenda remains the most appropriate weight management option.
Patients are encouraged to report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app). Patient safety is paramount, and open communication between patients and their healthcare team ensures that treatment benefits are maximised whilst minimising risks and managing side effects effectively.
Frequently Asked Questions
Can Saxenda cause bile acid malabsorption?
There is no established evidence that Saxenda causes or worsens bile acid malabsorption. However, patients with pre-existing BAM should discuss treatment with their GP, as Saxenda's gastrointestinal effects could potentially exacerbate diarrhoeal symptoms.
How is bile acid malabsorption diagnosed in the UK?
Bile acid malabsorption is typically diagnosed using a SeHCAT scan, which measures bile acid retention over seven days. A retention value below 15% is considered abnormal, with severity classified as mild (10-15%), moderate (5-10%), or severe (<5%).
What should I do if I experience severe diarrhoea whilst taking Saxenda?
Contact your GP or prescribing clinician if diarrhoea persists beyond 48 hours, worsens significantly, or is accompanied by dehydration, fever, or blood in stools. Seek immediate medical attention if you experience severe symptoms or signs of dehydration.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










