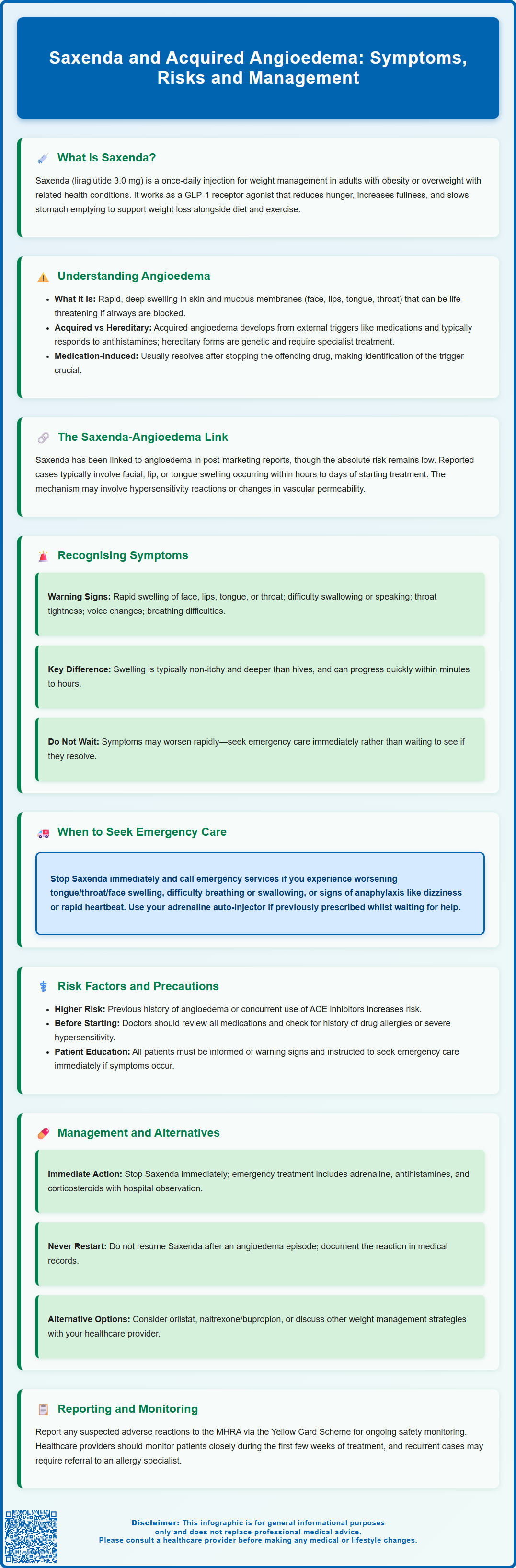
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities. Whilst generally well tolerated, Saxenda and acquired angioedema have been linked through post-marketing reports, with hypersensitivity reactions including angioedema documented in the Summary of Product Characteristics. Although rare, angioedema can cause rapid swelling of the face, lips, tongue, or throat, potentially leading to life-threatening airway obstruction. Understanding this association, recognising early symptoms, and knowing when to seek urgent medical attention are essential for patients and healthcare professionals to ensure safe use of this medication.
Summary: Saxenda (liraglutide) can trigger acquired angioedema, a rare hypersensitivity reaction causing rapid swelling of the face, lips, tongue, or throat, which requires immediate discontinuation and emergency medical attention if airway compromise occurs.
- Saxenda is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities.
- Angioedema associated with Saxenda is classified as 'not known' frequency in post-marketing surveillance and involves deeper tissue swelling distinct from urticaria.
- Symptoms include rapid facial or throat swelling, difficulty breathing or swallowing, and typically do not itch; onset can occur within hours to days of treatment.
- Patients with previous angioedema, concurrent ACE inhibitor use, or drug allergy history may have increased susceptibility to this reaction.
- Management involves immediate discontinuation of Saxenda, emergency treatment with adrenaline if airway compromise occurs, and avoidance of rechallenge with the medication.
- Suspected reactions should be reported to the MHRA via the Yellow Card Scheme, and alternative weight management options should be considered following an episode.
Table of Contents
- Understanding Saxenda and Its Mechanism of Action
- What Is Acquired Angioedema and How Does It Differ from Hereditary Forms?
- The Link Between Saxenda and Angioedema: Evidence and Reported Cases
- Recognising Symptoms and When to Seek Urgent Medical Attention
- Risk Factors and Precautions for Patients Prescribed Saxenda
- Management and Alternative Treatment Options
- Frequently Asked Questions
Understanding Saxenda and Its Mechanism of Action
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as type 2 diabetes, hypertension, or dyslipidaemia. It is administered as a once-daily subcutaneous injection and is intended to be used alongside a reduced-calorie diet and increased physical activity.
Liraglutide belongs to a class of medications known as glucagon-like peptide-1 (GLP-1) receptor agonists. It works by mimicking the action of the naturally occurring hormone GLP-1, which is released from the intestine in response to food intake. By binding to GLP-1 receptors in the brain, particularly in areas that regulate appetite, Saxenda helps to reduce hunger and increase feelings of fullness. This leads to a reduction in calorie intake and, consequently, weight loss over time.
The recommended titration schedule for Saxenda in the UK starts at 0.6 mg daily, with weekly increases of 0.6 mg until reaching the maintenance dose of 3.0 mg daily. This gradual titration is primarily designed to improve gastrointestinal tolerability rather than to prevent hypersensitivity reactions.
Additionally, liraglutide slows gastric emptying, which prolongs the sensation of satiety after meals, and modulates insulin secretion in a glucose-dependent manner. When used alone in non-diabetic patients, the risk of hypoglycaemia is minimal, though this risk increases if used alongside insulin or sulfonylureas in people with diabetes. Saxenda contains the same active substance as Victoza (liraglutide 1.8 mg), which is licensed for the treatment of type 2 diabetes, but Saxenda is used at a higher dose specifically for weight management.
The Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) have approved Saxenda based on clinical trial data demonstrating its efficacy and safety profile. However, like all medications, it carries potential risks and adverse effects that patients and healthcare professionals must be aware of, including rare but serious reactions such as angioedema.
What Is Acquired Angioedema and How Does It Differ from Hereditary Forms?
Angioedema is a condition characterised by rapid swelling of the deeper layers of the skin and mucous membranes, typically affecting the face, lips, tongue, throat, and sometimes the extremities or gastrointestinal tract. Unlike urticaria (hives), which involves the superficial layers of the skin, angioedema affects the subcutaneous and submucosal tissues, resulting in deeper, non-pitting swelling that can be disfiguring and, in severe cases, life-threatening if the airway becomes compromised.
Acquired angioedema refers to cases that develop during a person's lifetime due to external triggers, rather than being inherited. There are two main types:
-
Histaminergic acquired angioedema: Common causes include allergic reactions to foods, medications (particularly ACE inhibitors and NSAIDs), insect stings, or infections. Drug-induced angioedema is a well-recognised phenomenon and can occur with various classes of medication. This type often responds to antihistamines and corticosteroids. In some cases, it may be idiopathic, meaning no clear trigger is identified.
-
Acquired C1-inhibitor deficiency (AAE-C1-INH): A rarer bradykinin-mediated form often associated with lymphoproliferative disorders or autoimmune conditions. This type typically presents later in life, does not respond to antihistamines or corticosteroids, and requires specialist treatments similar to those used for hereditary angioedema.
Hereditary angioedema (HAE), by contrast, is a rare genetic disorder caused by a deficiency or dysfunction of C1-esterase inhibitor, a protein that regulates the complement and contact activation pathways. HAE typically presents in childhood or adolescence with recurrent episodes of swelling that are not associated with urticaria and do not respond to antihistamines or corticosteroids. Episodes may be triggered by stress, trauma, or hormonal changes.
The key differences lie in the underlying mechanism, age of onset, family history, and response to treatment. Acquired angioedema related to medications usually resolves once the offending agent is discontinued. For recurrent or unexplained angioedema without urticaria, investigations including C4 levels and C1-inhibitor level and function tests should be considered, with referral to an immunology specialist. Distinguishing between these forms is essential for appropriate management and prevention of future episodes.
The Link Between Saxenda and Angioedema: Evidence and Reported Cases
The association between Saxenda and angioedema is documented in the product's Summary of Product Characteristics (SmPC) and Patient Information Leaflet (PIL). According to the UK Saxenda SmPC, hypersensitivity reactions including angioedema have been reported during post-marketing use, with the frequency classified as "not known" (cannot be estimated from the available data).
The mechanism by which GLP-1 receptor agonists like liraglutide may trigger angioedema is not fully understood. It is hypothesised that the drug may induce hypersensitivity reactions in susceptible individuals, potentially mediated by immunological pathways or through effects on vascular permeability. However, this remains theoretical, and the exact pathophysiology is unknown. Unlike ACE inhibitor-induced angioedema, which is bradykinin-mediated, the pathophysiology of GLP-1 agonist-related angioedema appears to be different, though further research is needed.
Reported cases in the literature and pharmacovigilance databases describe patients who developed facial swelling, lip oedema, or tongue swelling within hours to days of initiating Saxenda therapy. In most instances, symptoms resolved following discontinuation of the medication and administration of antihistamines or corticosteroids. Rechallenge with liraglutide has generally not been recommended due to the risk of recurrence.
It is important to note that while there is an established link between Saxenda and angioedema, the absolute risk remains low. Healthcare professionals should be vigilant, particularly during the initial weeks of treatment, and patients should be counselled on recognising early symptoms. There is no official link suggesting that Saxenda causes hereditary angioedema, but it can trigger acquired angioedema in predisposed individuals.
Suspected adverse reactions to Saxenda, including angioedema, should be reported to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk). Ongoing pharmacovigilance continues to monitor the safety profile of liraglutide and other GLP-1 receptor agonists.
Recognising Symptoms and When to Seek Urgent Medical Attention
Early recognition of angioedema is critical to prevent potentially life-threatening complications, particularly airway obstruction. Patients prescribed Saxenda should be educated about the key symptoms of angioedema, which include:
-
Rapid swelling of the face, lips, tongue, or throat
-
Difficulty swallowing or speaking (dysphagia or dysphonia)
-
Sensation of throat tightness or a feeling that the airway is narrowing
-
Hoarseness or change in voice
-
Difficulty breathing (dyspnoea or stridor)
-
Swelling of the hands, feet, or genitals (less common but possible)
-
Abdominal pain, nausea, or vomiting (if gastrointestinal mucosa is affected)
Unlike urticaria, angioedema typically does not itch, and the swelling is deeper, firmer, and may be skin-coloured rather than red. Symptoms can develop rapidly, sometimes within minutes to hours of drug exposure, though delayed reactions are also possible.
When to seek urgent medical attention:
Patients should be advised to stop taking Saxenda immediately and seek emergency medical help (call 999 or attend A&E) if they experience any of the following:
-
Swelling of the tongue, throat, or face that is rapidly worsening
-
Difficulty breathing, shortness of breath, or wheezing
-
Difficulty swallowing or drooling
-
Feeling faint, dizzy, or experiencing a rapid heartbeat (which may indicate anaphylaxis)
Even if symptoms appear mild initially, they can progress quickly. Patients should not wait to see if symptoms resolve on their own. If the patient has been prescribed an adrenaline auto-injector for previous allergic reactions, they should use it as directed while awaiting emergency care if they develop signs of anaphylaxis or airway compromise.
In the emergency setting, treatment may include adrenaline (for anaphylaxis or airway involvement), antihistamines, and corticosteroids. Healthcare professionals should document the reaction and advise against restarting Saxenda or other GLP-1 receptor agonists without specialist consultation.
Risk Factors and Precautions for Patients Prescribed Saxenda
While angioedema associated with Saxenda is rare, certain risk factors may increase an individual's susceptibility to this adverse reaction. Healthcare professionals should conduct a thorough medical history and risk assessment before prescribing liraglutide for weight management.
Key risk factors include:
-
Previous history of angioedema from any cause, including drug-induced, allergic, or idiopathic episodes
-
Concurrent use of medications known to cause angioedema, particularly ACE inhibitors, which carry a stronger association with angioedema than angiotensin receptor blockers (ARBs) or NSAIDs
-
History of allergic reactions to other medications or severe hypersensitivity disorders
-
Family history of hereditary angioedema, though this does not directly increase risk of drug-induced angioedema
Precautions for prescribers:
Before initiating Saxenda, clinicians should:
-
Review the patient's medication list for potential drug interactions or concurrent angioedema-inducing agents, particularly ACE inhibitors
-
Counsel patients on the signs and symptoms of angioedema and provide clear instructions on when to seek emergency care
-
Follow the standard titration schedule (starting at 0.6 mg daily and increasing by 0.6 mg weekly to 3.0 mg) to improve gastrointestinal tolerability, though this does not prevent hypersensitivity reactions
-
Document the discussion and ensure patients understand the importance of reporting any unusual swelling or breathing difficulties immediately
-
Advise patients to carry information about their medication, particularly if they have a history of drug allergies
Monitoring during treatment:
Patients should be reviewed regularly, particularly in the first few weeks of therapy. Any reports of facial swelling, lip oedema, or respiratory symptoms should prompt immediate discontinuation of Saxenda and further investigation. Referral to an allergy specialist or immunologist may be appropriate for patients with recurrent or unexplained angioedema.
Patients should be encouraged to report suspected adverse reactions to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk).
Management and Alternative Treatment Options
If a patient develops angioedema while taking Saxenda, immediate management involves discontinuation of the medication and symptomatic treatment. In the acute setting, this may include:
-
Adrenaline (epinephrine) intramuscular injection if there are signs of anaphylaxis or airway compromise
-
Antihistamines (e.g., cetirizine, chlorphenamine) to reduce swelling and allergic response in histaminergic angioedema
-
Corticosteroids (e.g., prednisolone, hydrocortisone) to dampen inflammation, though their onset of action is slower
-
Airway management and oxygen therapy if respiratory distress is present
-
Observation in hospital until symptoms fully resolve, as angioedema can recur or worsen
It's important to note that antihistamines and corticosteroids may be ineffective for bradykinin-mediated angioedema (such as that caused by ACE inhibitors or in hereditary/acquired C1-inhibitor deficiency). In these cases, specialist treatments such as C1-esterase inhibitor concentrate or icatibant may be required under specialist care.
Patients should be advised not to restart Saxenda following an episode of angioedema. The reaction should be documented in their medical records, and the patient should be provided with information to share with other healthcare providers.
Alternative treatment options for weight management:
For patients who cannot tolerate Saxenda, several alternatives exist, depending on individual circumstances and comorbidities:
-
Orlistat (Xenical, Alli): A lipase inhibitor that reduces fat absorption; available over the counter at lower doses or on prescription
-
Naltrexone/bupropion (Mysimba): A combination therapy acting on the central nervous system to reduce appetite (availability may vary by local NHS commissioning policies)
-
Semaglutide (Wegovy): Another GLP-1 receptor agonist licensed for weight management; however, cross-reactivity is possible, and caution is advised
-
Lifestyle interventions: Referral to specialist weight management services, dietitians, or structured programmes such as NHS-supported behavioural therapy
-
Bariatric surgery: For patients with severe obesity (BMI ≥40 or ≥35 with comorbidities) who meet NICE criteria
NICE guidance (CG189) recommends a multicomponent approach to weight management, emphasising diet, physical activity, and behavioural support. Pharmacotherapy should be considered as an adjunct, not a replacement, for lifestyle modification. Shared decision-making is essential to identify the most appropriate and safe treatment pathway for each patient.
Frequently Asked Questions
Can Saxenda cause angioedema?
Yes, Saxenda (liraglutide) can cause acquired angioedema as a rare hypersensitivity reaction. This is documented in the UK Summary of Product Characteristics, though the exact frequency cannot be estimated from available data.
What should I do if I develop facial swelling whilst taking Saxenda?
Stop taking Saxenda immediately and seek emergency medical attention by calling 999 or attending A&E if you experience rapid facial, lip, or tongue swelling, difficulty breathing, or throat tightness. Do not wait to see if symptoms resolve on their own.
Is it safe to restart Saxenda after an episode of angioedema?
No, patients should not restart Saxenda following an episode of angioedema due to the risk of recurrence. Alternative weight management treatments should be discussed with your healthcare provider, and the reaction should be documented in your medical records.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript