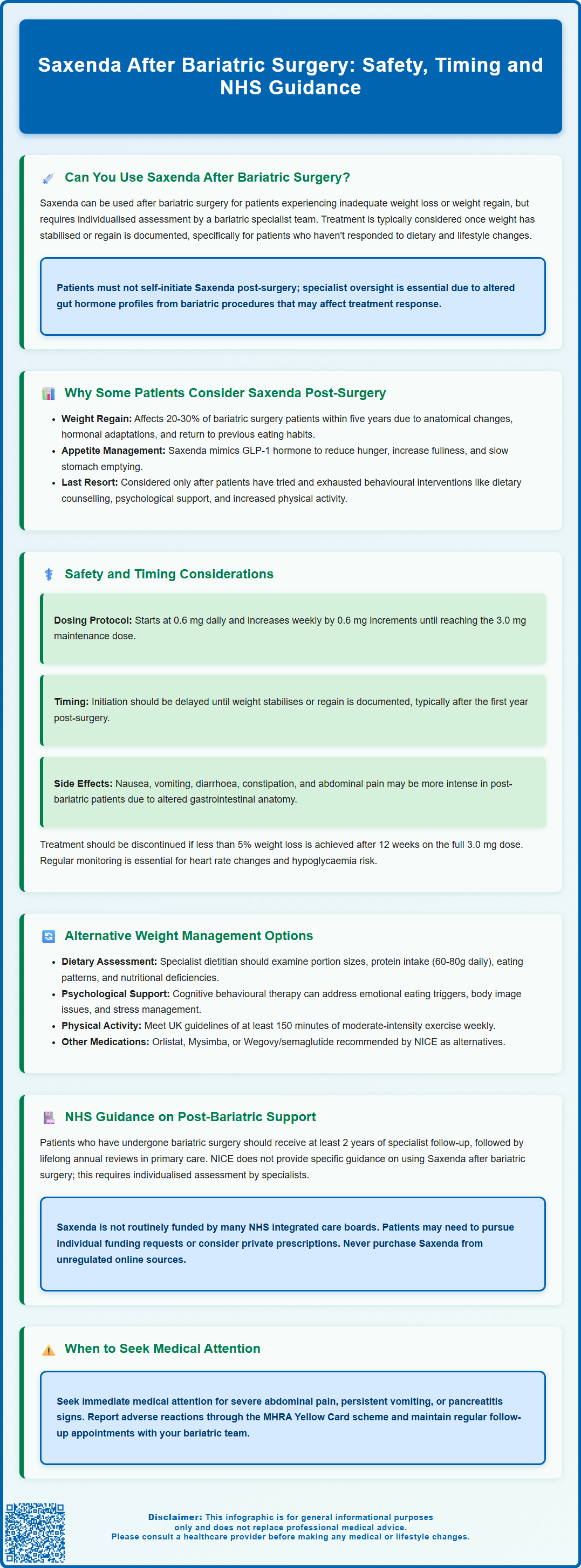
Saxenda after bariatric surgery may be considered for patients experiencing weight regain or inadequate initial weight loss following procedures such as gastric bypass or sleeve gastrectomy. Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed for weight management in adults with obesity or overweight with comorbidities. Whilst not contraindicated post-bariatric surgery, its use requires careful specialist assessment within a multidisciplinary team. This article examines the evidence, safety considerations, timing, and NHS guidance for using Saxenda in post-bariatric patients, alongside alternative weight management strategies.
Summary: Saxenda (liraglutide 3.0 mg) can be used after bariatric surgery for weight regain or inadequate loss, but requires specialist assessment and multidisciplinary team oversight.
- Saxenda is a GLP-1 receptor agonist licensed for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with comorbidities.
- Weight regain affects approximately 20–30% of bariatric patients within five years, prompting consideration of pharmacological support.
- Common adverse effects include nausea, vomiting, diarrhoea, and abdominal pain, which may be more problematic in patients with altered gastrointestinal anatomy.
- Saxenda is contraindicated in pregnancy, breastfeeding, and patients with a history of pancreatitis; it should not be combined with other GLP-1 receptor agonists.
- NICE does not provide specific guidance on Saxenda post-bariatric surgery; decisions require individualised specialist assessment and are not routinely NHS-funded.
- Treatment should be discontinued if less than 5% weight loss is achieved after 12 weeks on the 3.0 mg maintenance dose.
Table of Contents
Can You Use Saxenda After Bariatric Surgery?
Saxenda (liraglutide 3.0 mg) can be used after bariatric surgery, though this decision requires careful clinical assessment and specialist input. Saxenda is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed for weight management in adults with a body mass index (BMI) of 30 kg/m² or above, or 27 kg/m² with weight-related comorbidities. Following bariatric procedures such as gastric bypass or sleeve gastrectomy, some patients experience inadequate weight loss or weight regain, prompting consideration of pharmacological support.
The use of Saxenda post-bariatric surgery is not contraindicated, but requires individualised assessment. Bariatric surgery itself alters gut hormone profiles, including endogenous GLP-1 secretion, which may influence how patients respond to exogenous GLP-1 analogues like Saxenda. Clinical evidence specifically examining Saxenda use after bariatric procedures remains limited.
Key considerations include:
-
Timing – typically considered once weight has stabilised or regain is documented, with no universal UK standard timeframe
-
Specialist oversight – decisions should involve the bariatric multidisciplinary team
-
Patient selection – appropriate for those with documented weight regain or insufficient initial weight loss despite adherence to dietary and lifestyle modifications
-
Dosing – starting at 0.6 mg daily, with weekly increases of 0.6 mg to the maintenance dose of 3.0 mg as tolerated
-
Treatment review – discontinuation if less than 5% weight loss is achieved after 12 weeks on the 3.0 mg dose
Patients should not initiate Saxenda independently after bariatric surgery. A thorough assessment by a specialist with expertise in both bariatric care and obesity pharmacotherapy is essential to evaluate suitability, potential benefits, and safety considerations specific to the individual's surgical history and current metabolic status.
Why Some Patients Consider Saxenda Post-Surgery
Weight regain following bariatric surgery is a recognised clinical challenge, affecting approximately 20–30% of patients within five years of their procedure, though rates vary by surgical technique and how regain is defined. This phenomenon can be distressing for individuals who have undergone major surgery with the expectation of sustained weight loss. Several factors contribute to post-bariatric weight regain, including anatomical changes to the surgical pouch, hormonal adaptations, psychological factors, and gradual return to previous eating patterns.
Inadequate initial weight loss represents another scenario where pharmacological support may be considered. Whilst most bariatric patients achieve significant weight reduction, a subset experiences suboptimal results despite good surgical technique and adherence to post-operative protocols. These individuals may benefit from additional interventions to reach their health goals.
Saxenda works by mimicking the action of GLP-1, a naturally occurring hormone that regulates appetite and food intake. According to its licensed indications, it acts on receptors in the brain to reduce hunger, increase satiety, and slow gastric emptying. For post-bariatric patients, these mechanisms may help address:
-
Increased appetite that can develop months or years after surgery as hormonal adaptations occur
-
Loss of restriction if the gastric pouch has stretched or the sleeve has dilated
-
Grazing behaviours or frequent small meals that circumvent surgical restriction
-
Metabolic adaptation where the body becomes more efficient at conserving energy
Patients considering Saxenda after bariatric surgery typically have exhausted behavioural interventions, including dietary counselling, psychological support, and increased physical activity. The medication is viewed as an adjunct to, rather than replacement for, the comprehensive lifestyle modifications that form the foundation of post-bariatric care.
Safety and Timing Considerations
The safety profile of Saxenda in post-bariatric patients requires careful consideration, as this population has unique anatomical and physiological characteristics. Common adverse effects of Saxenda include nausea, vomiting, diarrhoea, constipation, and abdominal pain—symptoms that may be particularly problematic in individuals with altered gastrointestinal anatomy. Patients who have undergone gastric bypass or sleeve gastrectomy may experience these effects more intensely or have difficulty distinguishing them from surgery-related complications.
Timing of initiation is an important clinical decision. Most specialists recommend waiting until weight has stabilised or regain is clearly documented before considering Saxenda. This approach allows for:
-
Completion of the rapid weight loss phase that typically occurs in the first year
-
Stabilisation of nutritional status and resolution of any post-operative deficiencies
-
Establishment of sustainable eating patterns and lifestyle habits
-
Clear documentation of weight regain or inadequate loss despite optimal behavioural adherence
Specific safety considerations include:
-
Pregnancy and breastfeeding – Saxenda is contraindicated during pregnancy and breastfeeding
-
Pancreatitis – contraindicated in patients with a history of pancreatitis
-
Gallbladder disease – increased risk of cholelithiasis and cholecystitis
-
Dehydration and renal impairment – gastrointestinal side effects may increase dehydration risk
-
Increased heart rate – regular monitoring recommended, especially in patients with cardiovascular disease
-
Hypoglycaemia – primarily a risk when combined with insulin or sulfonylureas; these medications may need dose adjustment
-
Medication interactions – Saxenda should not be used with other GLP-1 receptor agonists
Patients should be monitored closely during initiation, with regular follow-up to assess efficacy, tolerability, and any complications. Immediate medical attention is warranted if severe abdominal pain, persistent vomiting, or signs of pancreatitis develop. Suspected adverse reactions should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Alternative Weight Management Options After Bariatric Surgery
Before considering pharmacological interventions like Saxenda, a comprehensive review of behavioural and lifestyle factors should be undertaken. The bariatric multidisciplinary team typically includes dietitians, psychologists, physiotherapists, and specialist nurses who can provide intensive support for weight regain or inadequate loss.
Dietary interventions remain the cornerstone of post-bariatric weight management. A specialist bariatric dietitian can assess:
-
Portion sizes and whether the patient has gradually increased intake beyond surgical restriction
-
Macronutrient composition – ensuring adequate protein intake (60–80g daily) whilst managing carbohydrate and fat consumption
-
Eating behaviours such as grazing, liquid calorie intake, or emotional eating patterns
-
Nutritional deficiencies that may affect metabolism or energy levels
Psychological support is equally important, as many patients experience complex relationships with food that surgery alone cannot resolve. Cognitive behavioural therapy (CBT) and other evidence-based psychological interventions can address:
-
Emotional eating triggers
-
Body image concerns
-
Unrealistic weight expectations
-
Stress management and coping strategies
Physical activity optimisation should be reviewed, with physiotherapy input if mobility limitations exist. UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity activity weekly, though post-bariatric patients may benefit from higher levels.
Alternative pharmacological options beyond Saxenda include:
-
Orlistat – a lipase inhibitor that reduces fat absorption, though less commonly used post-bariatric surgery due to gastrointestinal side effects
-
Naltrexone-bupropion (Mysimba) – a combination therapy affecting appetite and reward pathways; licensed in the UK but NHS commissioning varies by region
-
Semaglutide (Wegovy) – a once-weekly GLP-1 receptor agonist recommended by NICE (TA875) for weight management in specialist services for eligible patients
Revisional bariatric surgery represents another option for selected patients with significant weight regain and anatomical issues such as gastro-gastric fistula or pouch dilation. This decision requires careful risk-benefit analysis and is typically reserved for cases where conservative measures have failed.
NHS Guidance on Post-Bariatric Weight Loss Support
The NHS approach to post-bariatric care emphasises long-term, multidisciplinary follow-up to optimise outcomes and address complications, including weight regain. NICE guideline CG189 on obesity management recommends that patients who have undergone bariatric surgery receive at least 2 years of specialist follow-up, followed by lifelong annual review in primary care, with more frequent contact if problems arise.
NICE does not provide specific guidance on the use of Saxenda following bariatric surgery, as this represents a specialised clinical scenario requiring individualised assessment. However, NICE TA875 does recommend semaglutide (Wegovy) for weight management in specialist services for eligible patients, though not specifically for post-bariatric use. The general principles of obesity pharmacotherapy outlined in NICE guidance apply: medications should be used as part of a comprehensive weight management programme, not as standalone interventions.
NHS England commissioning policies for bariatric surgery include provisions for post-operative support, though the availability and intensity of services vary by region. Patients experiencing weight regain should:
-
Contact their bariatric surgical team or GP to request referral back to the specialist service
-
Request access to the multidisciplinary team, including dietetic and psychological support
-
Ensure regular monitoring of nutritional status, including vitamin and mineral levels
Funding considerations are relevant, as Saxenda is not routinely commissioned by many NHS integrated care boards (ICBs) for any indication, including post-bariatric use. Patients may need to:
-
Explore individual funding requests (IFRs) through their local ICB if clinical need is demonstrated
-
Consider private prescription options, though costs vary and patients should check current pricing with prescribers or pharmacies
-
Discuss clinical trial opportunities if available through their bariatric centre
Patient safety advice includes:
-
Never purchasing Saxenda from unregulated online sources
-
Ensuring proper training on injection technique and pen device use
-
Reporting suspected adverse effects promptly to the prescribing clinician and via the MHRA Yellow Card scheme
-
Maintaining regular follow-up appointments for monitoring and support
The decision to use Saxenda after bariatric surgery should always be made collaboratively between patient and specialist, with realistic expectations about potential benefits and a commitment to ongoing lifestyle modification as the foundation of long-term weight management success.
Frequently Asked Questions
How long after bariatric surgery can you start Saxenda?
There is no universal UK standard timeframe, but most specialists recommend waiting until weight has stabilised or regain is clearly documented, typically after the first year when rapid weight loss has completed and nutritional status has stabilised.
Is Saxenda effective for weight regain after gastric bypass or sleeve gastrectomy?
Clinical evidence specifically examining Saxenda use after bariatric procedures remains limited. Its effectiveness requires individualised assessment by specialists, as bariatric surgery alters gut hormone profiles which may influence response to GLP-1 analogues.
Does the NHS fund Saxenda for post-bariatric weight regain?
Saxenda is not routinely commissioned by many NHS integrated care boards for any indication, including post-bariatric use. Patients may explore individual funding requests through their local ICB or consider private prescription options.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript