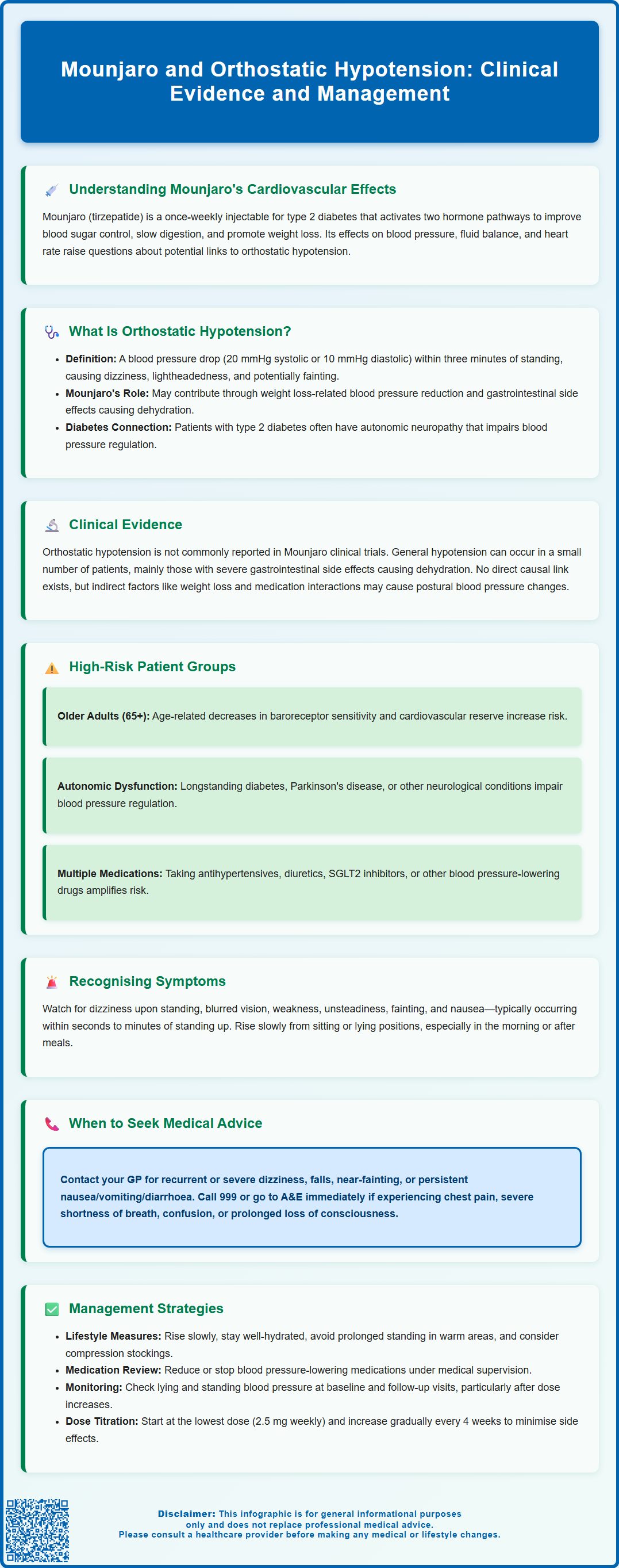
Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst orthostatic hypotension is not a commonly reported adverse effect, indirect mechanisms—including weight loss, gastrointestinal side effects causing dehydration, and interactions with concurrent medications—may contribute to postural blood pressure changes in susceptible individuals. Understanding the relationship between Mounjaro and orthostatic hypotension is essential for safe prescribing, particularly in older adults, those with autonomic neuropathy, and patients taking multiple antihypertensive agents. This article examines the clinical evidence, risk factors, symptom recognition, and practical management strategies to optimise patient safety.
Summary: Mounjaro (tirzepatide) is not directly associated with orthostatic hypotension, but weight loss, gastrointestinal side effects causing dehydration, and interactions with concurrent medications may contribute to postural blood pressure changes in susceptible patients.
- Tirzepatide is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus.
- Orthostatic hypotension is not commonly reported in clinical trials, though hypotension and dehydration are recognised adverse reactions.
- Risk factors include older age, autonomic neuropathy, polypharmacy (especially antihypertensives and diuretics), and volume depletion from gastrointestinal side effects.
- Patients should be monitored with lying and standing blood pressure measurements, particularly during dose titration.
- Management includes slow postural changes, adequate hydration, medication review, and specialist referral if symptoms persist despite conservative measures.
Table of Contents
- Understanding Mounjaro (Tirzepatide) and Its Cardiovascular Effects
- What Is Orthostatic Hypotension and How Does It Relate to Mounjaro?
- Clinical Evidence: Does Mounjaro Cause Orthostatic Hypotension?
- Risk Factors and Patient Populations at Higher Risk
- Recognising Symptoms and When to Seek Medical Advice
- Managing Orthostatic Hypotension While Taking Mounjaro
- Frequently Asked Questions
Understanding Mounjaro (Tirzepatide) and Its Cardiovascular Effects
Mounjaro (tirzepatide) is a once-weekly injectable medication licensed in the UK for the treatment of type 2 diabetes mellitus. It represents a novel class of medicines known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. By activating both incretin pathways simultaneously, tirzepatide enhances insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite—mechanisms that collectively improve glycaemic control and promote weight loss.
From a cardiovascular perspective, some GLP-1 receptor agonists (such as liraglutide, semaglutide and dulaglutide) have demonstrated favourable effects in large-scale trials, including reductions in major adverse cardiovascular events (MACE) in patients with established cardiovascular disease. Tirzepatide's dual mechanism may confer additional metabolic benefits, though cardiovascular outcome trials are still ongoing to provide definitive evidence. Like other incretin-based therapies, tirzepatide can influence blood pressure and fluid balance and may cause a small increase in heart rate. These effects have prompted questions about its potential association with orthostatic hypotension—a condition characterised by a significant drop in blood pressure upon standing.
Understanding the interplay between Mounjaro's pharmacological actions and cardiovascular physiology is essential for clinicians and patients alike. While the medication's primary effects target glucose metabolism, secondary effects on the autonomic nervous system, intravascular volume, and vascular tone may have implications for blood pressure regulation, particularly in vulnerable populations. This article examines the evidence linking Mounjaro to orthostatic hypotension and provides practical guidance for safe prescribing and monitoring.
What Is Orthostatic Hypotension and How Does It Relate to Mounjaro?
Orthostatic hypotension (also known as postural hypotension) is defined as a sustained reduction in systolic blood pressure of at least 20 mmHg or diastolic blood pressure of at least 10 mmHg within three minutes of standing or head-up tilt. This drop in blood pressure occurs because the body's compensatory mechanisms—primarily involving the autonomic nervous system and baroreceptor reflexes—fail to maintain adequate cerebral perfusion when moving from a supine or seated position to standing.
Common symptoms include dizziness, light-headedness, blurred vision, weakness, fatigue, and in severe cases, syncope (fainting). These symptoms typically occur shortly after standing and may resolve upon sitting or lying down. Orthostatic hypotension is particularly prevalent in older adults, individuals with diabetes (due to autonomic neuropathy), and those taking multiple antihypertensive medications.
The potential relationship between Mounjaro and orthostatic hypotension is multifactorial. Firstly, tirzepatide promotes weight loss, which can lead to reductions in blood pressure—a generally beneficial effect, but one that may unmask or exacerbate postural hypotension in predisposed individuals. Secondly, GLP-1 receptor agonists can cause gastrointestinal side effects such as nausea, vomiting, and diarrhoea, particularly during dose escalation. These symptoms may lead to reduced oral intake and dehydration, further compromising intravascular volume and blood pressure stability.
Additionally, patients with type 2 diabetes often have underlying cardiovascular autonomic neuropathy, which impairs the body's ability to regulate blood pressure dynamically. When combined with the blood pressure-lowering effects of weight loss and potential volume depletion, the risk of orthostatic symptoms may increase. Concomitant medications, particularly SGLT2 inhibitors, can further increase the risk of volume depletion and hypotension.
While orthostatic hypotension is not specifically listed in the UK Summary of Product Characteristics (SmPC) for Mounjaro, hypotension and dehydration are recognised as potential adverse reactions, particularly in patients experiencing gastrointestinal side effects.
Clinical Evidence: Does Mounjaro Cause Orthostatic Hypotension?
Current clinical trial data and post-marketing surveillance do not identify orthostatic hypotension as a commonly reported adverse effect of tirzepatide. In the pivotal SURPASS clinical trial programme, which evaluated tirzepatide across various doses in patients with type 2 diabetes, orthostatic hypotension was not highlighted as a significant safety signal. The most frequently reported adverse events were gastrointestinal in nature—nausea, diarrhoea, vomiting, and constipation—consistent with the known side-effect profile of GLP-1 receptor agonists.
However, hypotension (low blood pressure in general) has been documented in a small proportion of patients, particularly in those experiencing significant gastrointestinal side effects leading to dehydration. The UK Summary of Product Characteristics (SmPC) for Mounjaro advises caution in patients at risk of dehydration and recommends appropriate fluid management, especially during dose titration.
Real-world evidence and pharmacovigilance data continue to accumulate as Mounjaro's use expands beyond clinical trial populations. Clinicians should remain vigilant for reports of dizziness, syncope, or falls—particularly in older adults or those with pre-existing autonomic dysfunction. It is also important to consider that many patients prescribed tirzepatide are concurrently taking other medications that can affect blood pressure, such as antihypertensives, diuretics, or SGLT2 inhibitors, which may compound the risk of postural hypotension.
In summary, while there is no established direct causal relationship between Mounjaro and orthostatic hypotension, indirect mechanisms—including weight loss, volume depletion from gastrointestinal side effects, and interactions with concomitant medications—may contribute to postural blood pressure changes in susceptible individuals. Ongoing monitoring and individualised risk assessment are essential components of safe prescribing.
Healthcare professionals and patients are encouraged to report any suspected adverse reactions to Mounjaro via the MHRA Yellow Card Scheme.
Risk Factors and Patient Populations at Higher Risk
Certain patient groups are at higher risk of developing orthostatic hypotension while taking Mounjaro, and clinicians should exercise particular caution when initiating or titrating the medication in these populations.
Older adults (aged 65 years and above) are inherently more susceptible to postural hypotension due to age-related changes in baroreceptor sensitivity, reduced cardiovascular reserve, and higher prevalence of polypharmacy. Additionally, older patients are more likely to have comorbidities such as heart failure, chronic kidney disease, or autonomic neuropathy, all of which impair blood pressure regulation.
Patients with longstanding type 2 diabetes are at increased risk due to cardiovascular autonomic neuropathy, a common microvascular complication that disrupts the autonomic control of heart rate and vascular tone. This condition predisposes individuals to both resting hypotension and exaggerated postural drops in blood pressure.
Individuals taking multiple antihypertensive agents—particularly alpha-blockers, vasodilators, diuretics, SGLT2 inhibitors, tricyclic antidepressants, antipsychotics, nitrates, PDE5 inhibitors, or centrally acting antihypertensives—are at heightened risk, as the blood pressure-lowering effects of these medications may be potentiated by weight loss and volume changes associated with tirzepatide therapy. Regular medication review and blood pressure monitoring are essential in this group.
Patients with neurological conditions such as Parkinson's disease, multiple system atrophy, or pure autonomic failure may have impaired autonomic function, increasing their susceptibility to orthostatic hypotension.
Patients with a history of dehydration or eating disorders may be more vulnerable to volume depletion, especially if they experience significant nausea or vomiting during Mounjaro initiation. Similarly, those with renal impairment may have altered fluid and electrolyte balance, further complicating blood pressure homeostasis. Gastroparesis, while a caution for GLP-1 receptor agonist use, may also contribute to fluid balance issues.
Finally, individuals with a prior history of syncope or falls should be carefully assessed before starting tirzepatide, as recurrent episodes could lead to serious injury. A thorough baseline assessment, including lying and standing blood pressure measurements, is recommended in all at-risk patients.
Recognising Symptoms and When to Seek Medical Advice
Patients prescribed Mounjaro should be educated about the signs and symptoms of orthostatic hypotension to enable early recognition and appropriate action. Common symptoms include:
-
Dizziness or light-headedness upon standing, particularly after prolonged sitting or lying down
-
Blurred or tunnel vision
-
Weakness, fatigue, or feeling faint
-
Unsteadiness or loss of balance, increasing fall risk
-
Syncope (fainting), which may occur suddenly and without warning
-
Nausea or clamminess, sometimes accompanying the drop in blood pressure
These symptoms typically occur within seconds to minutes of standing and often improve upon sitting or lying down. Patients should be advised to rise slowly from sitting or lying positions, particularly in the morning or after meals, when postural hypotension is more likely.
When to contact a GP or healthcare professional:
Patients should seek medical advice if they experience recurrent or severe dizziness, especially if accompanied by falls, near-fainting episodes, or syncope. Any episode of loss of consciousness warrants urgent medical assessment to exclude serious underlying causes such as cardiac arrhythmias or significant volume depletion.
Additionally, patients should report persistent nausea, vomiting, or diarrhoea, as these may lead to dehydration and exacerbate hypotension. If symptoms coincide with the initiation or dose escalation of Mounjaro, a medication review may be necessary.
For urgent but non-emergency advice, patients can contact NHS 111.
Immediate medical attention (999 or A&E) is required if a patient experiences chest pain, severe shortness of breath, confusion, or prolonged loss of consciousness, as these may indicate more serious cardiovascular or neurological events.
Driving advice: Patients experiencing syncope or near-syncope should be advised not to drive and to check the DVLA guidance on 'Assessing fitness to drive' regarding blackouts. They should inform the DVLA about their condition if required and follow their doctor's advice about when it is safe to resume driving.
Managing Orthostatic Hypotension While Taking Mounjaro
Effective management of orthostatic hypotension in patients taking Mounjaro involves a combination of non-pharmacological strategies, medication review, and individualised monitoring.
Non-pharmacological measures form the cornerstone of management. Patients should be advised to:
-
Rise slowly from lying or sitting positions, pausing briefly in a seated position before standing
-
Maintain adequate hydration, particularly during periods of gastrointestinal side effects
-
Avoid prolonged standing, especially in warm environments or after large meals
-
Wear compression stockings (if appropriate and tolerated) to improve venous return—these should be properly fitted and avoided in patients with significant peripheral arterial disease
-
Elevate the head of the bed by 10–20 degrees to reduce nocturnal diuresis and morning hypotension
-
Consider dietary salt intake only under clinician supervision and if not contraindicated by heart failure, hypertension or renal disease
Medication review is essential. Clinicians should assess all concurrent medications, particularly antihypertensives, diuretics, SGLT2 inhibitors, and other agents that may lower blood pressure. Dose reduction or discontinuation of non-essential blood pressure-lowering drugs may be warranted, guided by regular blood pressure monitoring both seated and standing.
Monitoring and follow-up: Patients at higher risk should have lying and standing blood pressure measurements performed at baseline and during follow-up visits, particularly after dose escalations. A structured titration schedule for Mounjaro—starting at the lowest dose (2.5 mg weekly for 4 weeks), then increasing to 5 mg, with further increases by 2.5 mg every 4 weeks or more as tolerated—can help minimise gastrointestinal side effects and associated volume depletion.
In cases where orthostatic hypotension persists despite conservative measures, specialist referral to endocrinology, cardiology, or geriatric medicine may be appropriate for further assessment and management. For persistent symptomatic orthostatic hypotension, specialists may consider medications such as midodrine (licensed in the UK) or fludrocortisone (often used off-label). In rare cases, discontinuation of tirzepatide may be necessary if symptoms are severe or refractory.
Overall, with careful patient selection, education, and monitoring, the benefits of Mounjaro in improving glycaemic control can be realised safely, even in patients at risk of orthostatic hypotension.
Frequently Asked Questions
Does Mounjaro directly cause orthostatic hypotension?
Mounjaro (tirzepatide) is not directly associated with orthostatic hypotension in clinical trials. However, indirect mechanisms such as weight loss, dehydration from gastrointestinal side effects, and interactions with concurrent antihypertensive medications may contribute to postural blood pressure changes in susceptible individuals.
Who is at higher risk of orthostatic hypotension when taking Mounjaro?
Higher-risk groups include older adults, patients with longstanding diabetes and autonomic neuropathy, those taking multiple antihypertensive agents or diuretics, individuals with neurological conditions affecting autonomic function, and patients with a history of syncope or falls.
What should I do if I experience dizziness when standing whilst taking Mounjaro?
Rise slowly from sitting or lying positions, maintain adequate hydration, and contact your GP if you experience recurrent or severe dizziness, near-fainting, or falls. Seek immediate medical attention (999 or A&E) if you experience loss of consciousness, chest pain, or severe shortness of breath.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript