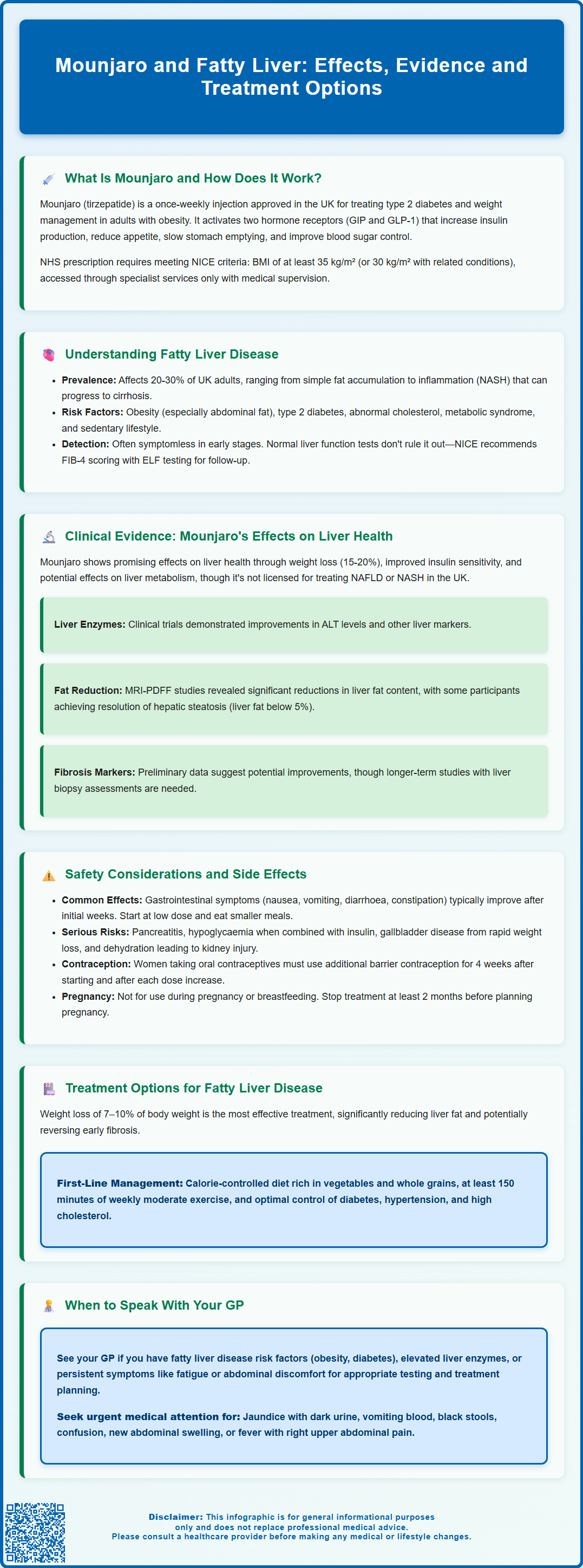
Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management. Emerging evidence suggests Mounjaro and fatty liver disease may be connected, with clinical trials showing improvements in liver enzyme levels and reductions in hepatic fat content among patients receiving this medication. Non-alcoholic fatty liver disease (NAFLD) affects up to 30% of UK adults and is closely linked to obesity and diabetes—conditions that Mounjaro is designed to address. Whilst not currently licensed specifically for liver disease treatment, tirzepatide's effects on weight loss and metabolic health may offer indirect hepatic benefits for eligible patients.
Summary: Mounjaro (tirzepatide) may improve liver health in patients with fatty liver disease through significant weight loss and enhanced insulin sensitivity, though it is not currently licensed in the UK specifically for treating NAFLD or NASH.
- Tirzepatide is a dual GIP and GLP-1 receptor agonist licensed for type 2 diabetes and weight management in adults meeting specific NICE criteria.
- Clinical trials show reductions in liver enzymes (ALT) and hepatic fat content in patients receiving Mounjaro, though these are surrogate markers.
- Non-alcoholic fatty liver disease affects 20–30% of UK adults and is closely associated with obesity, type 2 diabetes, and metabolic syndrome.
- Common side effects include gastrointestinal symptoms (nausea, vomiting, diarrhoea); serious risks include pancreatitis, gallbladder disease, and hypoglycaemia when combined with certain diabetes medications.
- Weight loss of 7–10% remains the cornerstone of NAFLD treatment according to NICE guidance, with lifestyle modification as first-line intervention.
- Patients with fatty liver disease or metabolic risk factors should discuss treatment options with their GP, who can arrange appropriate investigations and specialist referral if needed.
Table of Contents
What Is Mounjaro and How Does It Work?
Mounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. It is administered as a once-weekly subcutaneous injection and represents a novel class of medication known as a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist.
The mechanism of action of Mounjaro involves mimicking two naturally occurring incretin hormones that play crucial roles in glucose regulation and appetite control. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion in a glucose-dependent manner, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. This dual action distinguishes it from single GLP-1 receptor agonists and contributes to its effects on glycaemic control and body weight reduction.
Clinical trials have demonstrated that Mounjaro can lead to significant reductions in HbA1c levels (a measure of long-term blood glucose control) and substantial weight loss. In the SURPASS clinical trial programme, tirzepatide showed greater reductions in HbA1c and body weight compared to some other diabetes treatments. The weight loss effect is particularly relevant when considering metabolic conditions such as fatty liver disease, where excess body weight and insulin resistance are key contributing factors.
Understanding Fatty Liver Disease and Its Causes
Fatty liver disease, medically termed hepatic steatosis, occurs when excess fat accumulates in liver cells. The condition exists in two main forms: alcohol-related fatty liver disease (ARLD) and non-alcoholic fatty liver disease (NAFLD), with the latter being increasingly common in the UK population. NAFLD affects an estimated 20–30% of adults in the UK and is closely associated with obesity, type 2 diabetes, and metabolic syndrome. It's worth noting that medical terminology is evolving, with metabolic dysfunction-associated steatotic liver disease (MASLD) increasingly being used internationally, though NICE guidance still refers to NAFLD.
NAFLD encompasses a spectrum of liver conditions, ranging from simple steatosis (fat accumulation without significant inflammation) to non-alcoholic steatohepatitis (NASH), which involves inflammation and liver cell damage. If left untreated, NASH can progress to liver fibrosis, cirrhosis, and in some cases, hepatocellular carcinoma. The progression is not inevitable, and many individuals with simple steatosis remain stable without advancing to more severe disease.
Key risk factors for developing NAFLD include:
-
Obesity, particularly central adiposity (excess abdominal fat)
-
Type 2 diabetes mellitus and insulin resistance
-
Dyslipidaemia (abnormal cholesterol and triglyceride levels)
-
Metabolic syndrome (a cluster of conditions including hypertension, hyperglycaemia, and abnormal lipids)
-
Sedentary lifestyle and poor dietary habits
The underlying pathophysiology involves insulin resistance, which leads to increased delivery of free fatty acids to the liver, enhanced hepatic fat synthesis, and impaired fat oxidation. This metabolic dysfunction creates a pro-inflammatory environment that can trigger liver injury. Importantly, fatty liver disease is often asymptomatic in its early stages, with many cases detected incidentally through blood tests or imaging performed for other reasons.
It's important to note that liver function tests can be normal in NAFLD, and ultrasound alone cannot reliably assess fibrosis severity. According to NICE guidance (NG49), primary care assessment typically involves calculating a fibrosis risk score (FIB-4), with enhanced liver fibrosis (ELF) testing recommended as a second-line test for those with indeterminate or high FIB-4 scores. NICE emphasises the importance of identifying and managing modifiable risk factors, particularly weight reduction and improved glycaemic control in those with diabetes.
Clinical Evidence: Mounjaro's Effects on Liver Health
Emerging clinical evidence suggests that Mounjaro may have beneficial effects on liver health in patients with fatty liver disease, although it is important to note that tirzepatide is not currently licensed specifically for the treatment of NAFLD or NASH in the UK. The potential hepatic benefits appear to be mediated through multiple mechanisms, including significant weight loss, improved insulin sensitivity, and possible effects on hepatic metabolism.
In the SURPASS clinical trial programme, which evaluated tirzepatide for type 2 diabetes management, secondary analyses revealed improvements in liver enzyme levels (particularly alanine aminotransferase, or ALT) among participants receiving the medication. While reductions in ALT often correlate with decreased hepatic inflammation and fat content, it's important to recognise that these are surrogate markers and do not definitively confirm histological improvement. In the SURMOUNT trials for weight management, participants achieved substantial weight loss, with some individuals losing 15–20% of their body weight over the study period, which may indirectly benefit liver health.
More targeted research has examined tirzepatide's effects specifically on NAFLD and NASH. Studies using advanced imaging techniques, including magnetic resonance imaging proton density fat fraction (MRI-PDFF), have shown significant reductions in liver fat content among patients treated with tirzepatide compared to placebo. The SYNERGY-NASH phase 2 trial has investigated histological outcomes in patients with steatohepatitis and fibrosis, with preliminary data suggesting that a proportion of participants achieved resolution of hepatic steatosis, defined as liver fat content below 5%.
Additionally, data suggest potential improvements in markers of liver fibrosis, though longer-term studies with histological endpoints (liver biopsy assessment) are needed to confirm whether Mounjaro can prevent or reverse fibrosis progression. The mechanism behind these hepatic benefits likely involves the medication's effects on weight reduction, enhanced insulin sensitivity, and reduced hepatic glucose production. Hypotheses about direct anti-inflammatory actions on liver tissue require further investigation.
Whilst these findings are encouraging, it is essential to emphasise that there is no official indication for Mounjaro in treating fatty liver disease outside of clinical trials. Patients should not expect this medication to be prescribed solely for liver concerns without meeting the licensed criteria for type 2 diabetes or weight management.
Safety Considerations and Potential Side Effects
As with all medications, Mounjaro carries potential side effects that patients and healthcare professionals must consider. The most commonly reported adverse effects are gastrointestinal in nature and include nausea, vomiting, diarrhoea, constipation, abdominal pain, and reduced appetite. These symptoms are typically most pronounced during the initial weeks of treatment and following dose escalations, often improving with continued use as the body adapts.
To minimise gastrointestinal side effects, Mounjaro is initiated at a low dose (2.5 mg once weekly) with gradual titration every four weeks, allowing patients to develop tolerance. Eating smaller, more frequent meals and avoiding high-fat foods may help manage nausea. If side effects become intolerable, dose reduction or temporary treatment interruption may be necessary under medical guidance.
More serious but less common adverse effects include:
-
Pancreatitis: Patients should be advised to seek immediate medical attention if they experience severe, persistent abdominal pain that may radiate to the back, as this could indicate acute pancreatitis. If pancreatitis is suspected, tirzepatide should be discontinued and appropriate investigation undertaken.
-
Hypoglycaemia: Whilst tirzepatide alone rarely causes low blood glucose, the risk increases when used alongside insulin or sulfonylureas; dose adjustments of concomitant medications may be required.
-
Gallbladder disease: Rapid weight loss can increase the risk of gallstone formation and cholecystitis.
-
Diabetic retinopathy complications: Rapid improvement in glycaemic control has been associated with temporary worsening of diabetic eye disease in susceptible individuals.
-
Dehydration and acute kidney injury: Severe gastrointestinal side effects may lead to dehydration; patients should maintain adequate fluid intake and seek medical advice if unable to maintain hydration.
-
Hypersensitivity reactions: Including rash, pruritus and rarely, anaphylaxis.
-
Injection site reactions: Such as redness, swelling or itching at the injection site.
Tirzepatide may reduce the effectiveness of oral contraceptives due to delayed gastric emptying. The MHRA advises that women using oral contraceptives should use an additional barrier method for 4 weeks after starting tirzepatide and for 4 weeks after each dose increase.
Tirzepatide is not recommended during pregnancy or breastfeeding. Women of childbearing potential should use effective contraception during treatment and discuss with their healthcare provider if planning pregnancy, as tirzepatide should be discontinued at least 2 months before a planned pregnancy.
Regarding liver-specific safety, clinical trials have not identified significant hepatotoxicity concerns with tirzepatide. In fact, as discussed, liver enzyme levels typically improve rather than worsen during treatment. However, patients with pre-existing liver disease should be monitored appropriately, and any unexplained symptoms such as jaundice, dark urine, or persistent right upper quadrant pain warrant prompt medical evaluation.
The MHRA continues to monitor the safety profile of Mounjaro through post-marketing surveillance, and healthcare professionals and patients are encouraged to report any suspected adverse reactions via the Yellow Card Scheme (yellowcard.mhra.gov.uk).
Treatment Options and When to Speak With Your GP
Management of fatty liver disease primarily focuses on addressing underlying metabolic risk factors through lifestyle modification and, where appropriate, pharmacological intervention. NICE guidance (NG49) emphasises that weight loss remains the cornerstone of NAFLD treatment, with evidence showing that losing 7–10% of body weight can significantly reduce liver fat, and greater weight loss may improve or resolve NASH and even reverse early fibrosis.
First-line interventions include:
-
Dietary modification: Adopting a balanced, calorie-controlled diet rich in vegetables, fruits, whole grains, and lean proteins whilst limiting processed foods, saturated fats, and added sugars
-
Regular physical activity: Aiming for at least 150 minutes of moderate-intensity exercise weekly, which improves insulin sensitivity independent of weight loss
-
Alcohol reduction: Even in NAFLD (non-alcohol-related), minimising alcohol consumption supports liver health
-
Management of comorbidities: Optimising control of diabetes, hypertension, and dyslipidaemia through appropriate medications
For patients with type 2 diabetes and NAFLD, medications such as pioglitazone (a thiazolidinedione) have shown benefits for liver health in addition to glycaemic control, though this is an off-label use in the UK and carries risks including fluid retention, weight gain and potential heart failure exacerbation. Vitamin E may be considered in select non-diabetic patients with biopsy-proven NASH, though this is also off-label and requires specialist input. Mounjaro, whilst not licensed specifically for fatty liver disease, may be an appropriate option for eligible patients with type 2 diabetes or obesity who meet NICE criteria, potentially offering dual benefits for metabolic and hepatic health.
You should speak with your GP if you:
-
Have been diagnosed with fatty liver disease and wish to discuss treatment options
-
Have risk factors for NAFLD (obesity, diabetes, metabolic syndrome) and are concerned about liver health
-
Experience symptoms that may indicate liver disease, such as persistent fatigue, abdominal discomfort, or unexplained weight loss
-
Are taking Mounjaro and develop concerning side effects or have questions about its effects on your liver
-
Have elevated liver enzymes on blood tests and need further investigation
Seek urgent medical attention if you develop jaundice (yellowing of the skin/eyes) with dark urine and pale stools, vomit blood, have black tarry stools, experience confusion or drowsiness, develop new swelling of the abdomen (ascites), or have fever with right upper abdominal pain.
Your GP can arrange appropriate investigations, including liver function tests, fibrosis risk assessment (FIB-4 score), and imaging studies (such as ultrasound). If your FIB-4 score is indeterminate or high, an enhanced liver fibrosis (ELF) test may be arranged. Depending on findings, referral to a hepatologist or specialist metabolic clinic may be warranted. For those meeting NICE criteria, discussion about Mounjaro or other weight management medications can be initiated, with careful consideration of individual circumstances, contraindications, and treatment goals. Remember that managing fatty liver disease is a long-term commitment requiring sustained lifestyle changes, and your healthcare team is there to support you throughout this journey.
Frequently Asked Questions
Can Mounjaro treat fatty liver disease?
Mounjaro is not currently licensed in the UK specifically for treating fatty liver disease. However, clinical evidence suggests it may improve liver health through significant weight loss and enhanced insulin sensitivity in patients who meet criteria for type 2 diabetes or weight management treatment.
How does Mounjaro affect liver enzymes?
Clinical trials show that Mounjaro typically improves liver enzyme levels, particularly alanine aminotransferase (ALT), which often correlates with reduced hepatic inflammation and fat content. Studies using advanced imaging have demonstrated significant reductions in liver fat among patients treated with tirzepatide.
Who is eligible for Mounjaro treatment in the UK?
According to NICE guidance, Mounjaro is available for adults with type 2 diabetes meeting specific criteria, or for weight management in specialist services for those with BMI ≥35 kg/m² (or ≥30 kg/m² with weight-related comorbidities) and additional qualifying factors. Your GP can assess eligibility and arrange appropriate referral.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript