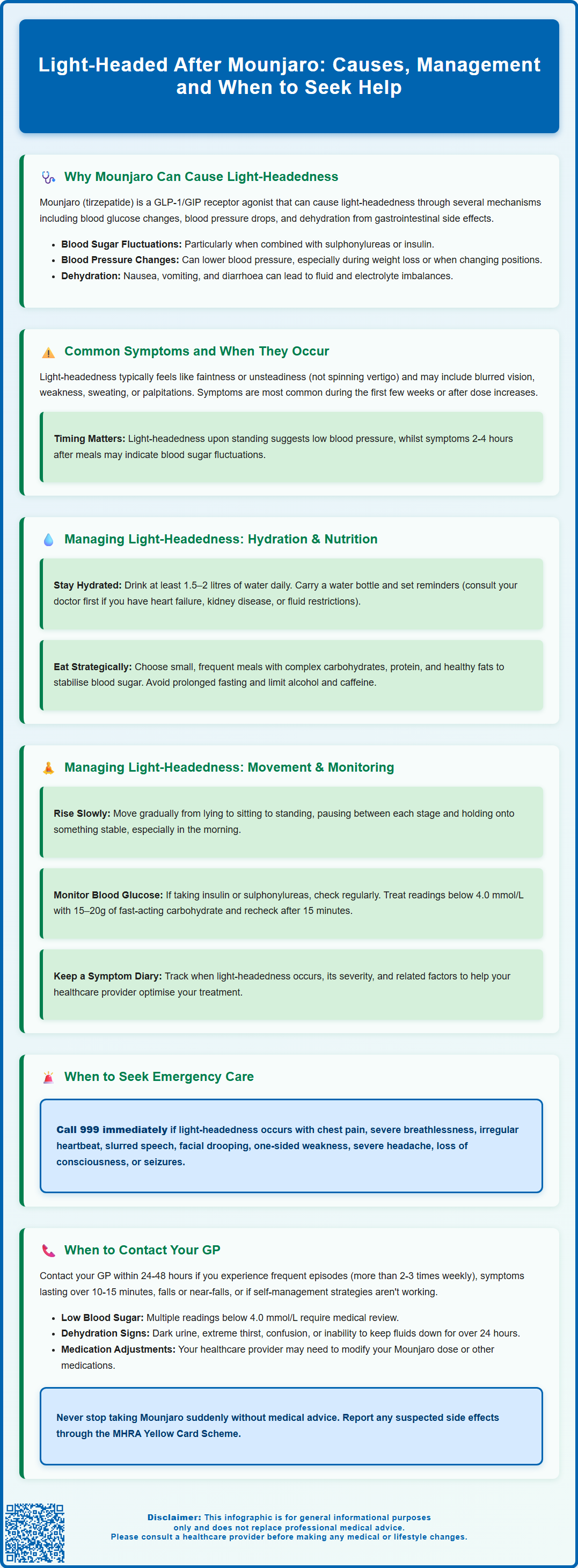
Feeling light-headed after taking Mounjaro (tirzepatide) is a recognised side effect that affects some patients, particularly during the initial weeks of treatment or following dose increases. This dual GLP-1 and GIP receptor agonist, licensed in the UK for type 2 diabetes and weight management, can cause dizziness through several mechanisms including blood glucose fluctuations, blood pressure changes, and gastrointestinal effects leading to dehydration. Understanding why light-headedness occurs, recognising warning signs, and knowing when to seek medical advice are essential for safe and effective treatment. Most cases can be managed with practical strategies, though persistent or severe symptoms require professional assessment.
Summary: Light-headedness after Mounjaro occurs through blood glucose changes, blood pressure reductions, and dehydration from gastrointestinal side effects, typically during initial treatment or dose escalation.
- Tirzepatide is a dual GLP-1 and GIP receptor agonist licensed in the UK for type 2 diabetes and weight management in adults with obesity or overweight with comorbidities.
- Light-headedness results from glucose-dependent insulin enhancement, gastric emptying delay, modest blood pressure reductions, and gastrointestinal effects causing dehydration.
- Hypoglycaemia risk increases significantly when Mounjaro is combined with sulphonylureas or insulin, requiring blood glucose monitoring and potential dose adjustment of concurrent medications.
- Self-management includes adequate hydration (1.5–2 litres daily), small frequent meals, slow postural changes, and maintaining a symptom diary to identify patterns.
- Seek emergency care (999) for light-headedness with chest pain, breathlessness, irregular heartbeat, neurological symptoms, loss of consciousness, or seizures.
- Contact your GP within 24–48 hours for recurrent episodes, confirmed hypoglycaemia, persistent symptoms despite self-care, or inability to maintain hydration for over 24 hours.
Table of Contents
Why Mounjaro Can Cause Light-Headedness
Mounjaro (tirzepatide) is a glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Tirzepatide is also licensed for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, as part of a reduced-calorie diet and increased physical activity programme. Light-headedness or dizziness is a recognised adverse effect that can occur through several mechanisms related to the drug's pharmacological action.
The primary mechanism involves changes in blood glucose levels. Tirzepatide enhances insulin secretion in a glucose-dependent manner and suppresses glucagon release. When used as monotherapy, hypoglycaemia is uncommon. However, the risk increases significantly when combined with other glucose-lowering medications, particularly sulphonylureas or insulin. Even mild drops in blood glucose can trigger symptoms of light-headedness, dizziness, or feeling faint. Additionally, Mounjaro significantly slows gastric emptying, which alters the rate at which nutrients are absorbed and can affect postprandial blood glucose patterns.
Cardiovascular effects may also contribute to light-headedness. Tirzepatide can cause modest reductions in blood pressure, which may be more pronounced in patients taking antihypertensive medications, diuretics, or those experiencing significant weight loss. These blood pressure changes may occasionally manifest as symptoms of dizziness or light-headedness, particularly when changing position.
Furthermore, the gastrointestinal adverse effects commonly associated with Mounjaro, including nausea, vomiting, and diarrhoea, can lead to dehydration and electrolyte imbalances. Reduced fluid volume and electrolyte disturbances can compromise circulatory function and contribute to feelings of light-headedness. These effects are typically most pronounced during the initial weeks of treatment or following dose escalation, as the body adjusts to the medication. Persistent vomiting or diarrhoea may increase the risk of acute kidney injury, particularly in patients taking diuretics or SGLT2 inhibitors.
Common Symptoms and When Light-Headedness Occurs
Light-headedness associated with Mounjaro typically presents as a sensation of feeling faint, unsteady, or dizzy, often described by patients as though they might lose balance or consciousness. This differs from vertigo, which involves a spinning sensation. Accompanying symptoms may include visual disturbances such as blurred vision, weakness, confusion, sweating, palpitations, or a feeling of disconnection from one's surroundings.
The timing of light-headedness is clinically significant and can provide clues to the underlying cause. Many patients report symptoms during the first few weeks of treatment or immediately following a dose increase, when gastrointestinal side effects are most prominent and the body is adapting to the medication's metabolic effects. Light-headedness occurring shortly after standing up (within seconds to minutes) suggests orthostatic hypotension (a drop of ≥20 mmHg systolic or ≥10 mmHg diastolic blood pressure within 3 minutes of standing), whilst symptoms appearing 2–4 hours after meals may indicate postprandial blood glucose fluctuations, particularly in patients taking additional glucose-lowering agents.
Morning light-headedness upon waking can reflect overnight fasting, dehydration, or medication effects, especially if gastrointestinal symptoms have been prominent. Some patients experience symptoms during or after physical activity, when increased metabolic demands may unmask borderline hypoglycaemia or inadequate hydration status.
The severity and frequency of light-headedness vary considerably between individuals. Mild, transient episodes lasting seconds to a few minutes are relatively common and often resolve spontaneously. If you experience dizziness, it's advisable to sit or lie down immediately to reduce the risk of falls, and to check your blood glucose level if you have monitoring equipment available. You should not drive or operate machinery while experiencing symptoms. Recurrent episodes, prolonged symptoms lasting more than several minutes, or light-headedness severe enough to cause falls or loss of consciousness require prompt medical evaluation. Patients should maintain awareness of patterns and triggers, as this information assists healthcare professionals in determining whether dose adjustment, additional investigation, or modification of concurrent medications is necessary.
Managing Light-Headedness While Taking Mounjaro
Practical self-management strategies can significantly reduce the frequency and severity of light-headedness whilst taking Mounjaro. Adequate hydration is paramount—patients should aim for at least 1.5–2 litres of fluid daily, increasing this during hot weather or if experiencing gastrointestinal symptoms. However, if you have heart failure, kidney disease, or have been advised to restrict fluids, consult your healthcare professional about appropriate fluid intake. Carrying a water bottle and setting regular reminders can help maintain consistent fluid intake throughout the day.
Dietary modifications play a crucial role in managing symptoms. Eating small, frequent meals rather than large portions helps stabilise blood glucose levels and reduces the burden on delayed gastric emptying. Including complex carbohydrates, adequate protein, and healthy fats in each meal provides sustained energy release. Patients should avoid prolonged fasting periods and consider having a small snack before bedtime if morning light-headedness is problematic. Reducing alcohol and caffeine intake is advisable, as both can contribute to dehydration and blood pressure fluctuations.
To prevent postural symptoms, patients should adopt careful postural changes—rising slowly from lying to sitting, pausing briefly, then standing gradually whilst holding onto a stable surface. Avoiding sudden movements, particularly first thing in the morning, reduces the risk of symptomatic blood pressure drops. If you're considering compression stockings, discuss this with your healthcare professional first to ensure they're appropriate for you.
Monitoring blood glucose is particularly important for patients taking insulin or sulphonylureas alongside Mounjaro. If you experience symptoms of light-headedness, check your blood glucose if possible. If levels are below 4.0 mmol/L, take 15–20g of fast-acting carbohydrate (such as glucose tablets, fruit juice or sugary drink), recheck after 15 minutes, and repeat if necessary. Once your glucose is above 4.0 mmol/L, have a starchy snack if your next meal is more than an hour away. Discuss with your GP or diabetes specialist nurse whether adjustment of concurrent medications is appropriate.
Medication timing and titration can also be optimised—taking Mounjaro at a consistent time each week, preferably when able to rest if needed, may help manage initial side effects. If side effects are troublesome, discuss with your prescriber about slowing the dose escalation or temporarily reverting to a lower dose. Patients should maintain a symptom diary recording episodes of light-headedness, their timing, severity, and any associated factors, which provides valuable information for healthcare professionals to guide management decisions. Do not drive or operate machinery if you are experiencing dizziness or are at risk of hypoglycaemia.
When to Seek Medical Advice About Dizziness
Whilst mild, transient light-headedness may be manageable with self-care measures, certain red flag symptoms warrant urgent medical attention. Patients should seek immediate emergency care (call 999 or attend A&E) if light-headedness is accompanied by chest pain, severe breathlessness, palpitations with irregular heartbeat, slurred speech, facial drooping, weakness or numbness on one side of the body, severe headache, loss of consciousness, or seizures. These symptoms may indicate serious cardiovascular or neurological events requiring immediate assessment.
Contact your GP or diabetes care team within 24–48 hours if you experience recurrent episodes of light-headedness (more than 2–3 times weekly), symptoms lasting longer than 10–15 minutes, light-headedness severe enough to cause falls or near-falls, persistent symptoms despite implementing self-management strategies, or if light-headedness is significantly impacting daily activities or quality of life. Additionally, seek advice if you notice confirmed hypoglycaemia (blood glucose below 4.0 mmol/L) on multiple occasions, particularly if you are not taking sulphonylureas or insulin, or if you experience symptoms of dehydration such as reduced urine output, dark urine, extreme thirst, or confusion. If you are unable to keep fluids down for more than 24 hours due to vomiting or diarrhoea, seek medical advice promptly to prevent dehydration and potential kidney problems.
If you cannot reach your GP and need advice, contact NHS 111 for guidance. Your healthcare professional may need to review your medication regimen, potentially adjusting the dose of Mounjaro or modifying concurrent medications such as antihypertensives or other glucose-lowering agents. They may arrange investigations including blood pressure monitoring (including postural readings), blood glucose profiling, full blood count to exclude anaemia, urea and electrolytes to assess hydration and renal function, and thyroid function tests if clinically indicated.
NICE guidance for tirzepatide emphasises the importance of individualised treatment approaches and regular monitoring when initiating or titrating GLP-1 receptor agonists. Patients should never discontinue Mounjaro abruptly without medical advice, as this may affect glycaemic control. Open communication with your healthcare team ensures that any adverse effects are appropriately managed whilst maintaining the therapeutic benefits of treatment. If you suspect you are experiencing side effects from Mounjaro, you can report these through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
How long does light-headedness from Mounjaro typically last?
Light-headedness is typically most pronounced during the first few weeks of treatment or following dose escalation, often improving as the body adjusts to the medication. Individual episodes usually last seconds to a few minutes, though persistent or recurrent symptoms require medical review.
Can I continue taking Mounjaro if I feel light-headed?
Mild, transient light-headedness can often be managed with hydration, dietary adjustments, and careful postural changes. However, you should contact your GP or diabetes care team if symptoms are recurrent, severe, or significantly impact daily activities, as dose adjustment or medication review may be necessary.
Should I check my blood glucose when feeling light-headed on Mounjaro?
Yes, particularly if you are taking insulin or sulphonylureas alongside Mounjaro. If your blood glucose is below 4.0 mmol/L, take 15–20g of fast-acting carbohydrate, recheck after 15 minutes, and contact your healthcare team if hypoglycaemia occurs repeatedly.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript