Many people seek to accelerate their weight loss, but understanding safe, evidence-based approaches is essential for long-term success. Whilst rapid results may seem appealing, the NHS recommends losing 0.5 to 1 kilogram weekly to minimise health risks and maximise sustainability. This article explores medically sound strategies to optimise weight loss within safe parameters, including dietary modifications, exercise recommendations, and when medical interventions may be appropriate. Whether you're beginning your weight management journey or seeking to overcome a plateau, understanding the balance between effectiveness and safety will help you achieve lasting results whilst protecting your health.
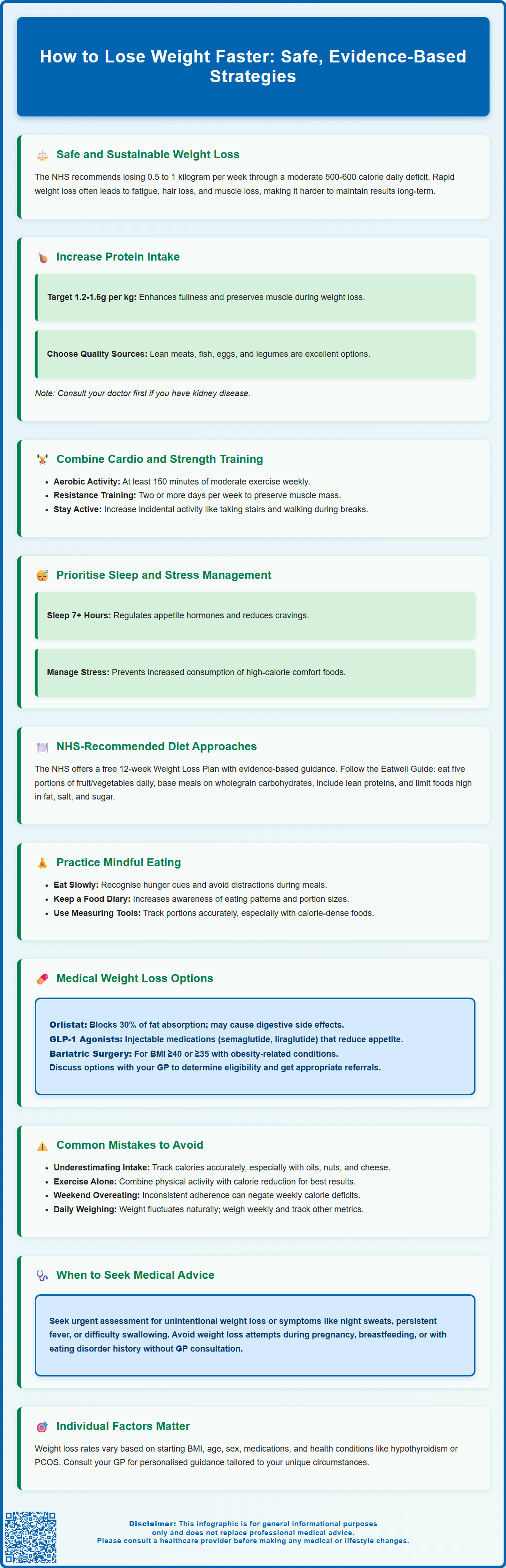
Summary: Safe weight loss acceleration involves creating a moderate calorie deficit (500-600 kcal daily), increasing protein intake, incorporating resistance training, optimising sleep, and practising mindful eating whilst maintaining the NHS-recommended rate of 0.5-1 kg weekly.
- The NHS recommends losing 0.5-1 kg weekly to minimise risks including nutritional deficiencies, muscle loss, and metabolic adaptation
- Higher protein intake (1.2-1.6g per kg body weight) combined with resistance training helps preserve lean muscle mass during calorie restriction
- Medical interventions including orlistat and GLP-1 receptor agonists may be appropriate for eligible individuals when lifestyle modifications prove insufficient
- Common obstacles include underestimating calorie intake, over-relying on exercise alone, inconsistent adherence, and expecting linear daily progress
- Unintentional weight loss with concerning symptoms (night sweats, persistent fever, rectal bleeding) requires urgent medical assessment
Table of Contents
Understanding Safe and Sustainable Weight Loss
Weight loss occurs when you consistently consume fewer calories than your body expends, creating an energy deficit. Whilst many people seek rapid results, the NHS recommends a gradual approach of losing 0.5 to 1 kilogram (1 to 2 pounds) per week. This rate is considered both safe and sustainable, minimising the risk of nutritional deficiencies, muscle loss, and metabolic adaptation that can occur with more aggressive calorie restriction.
Faster weight loss may seem appealing, but it often proves difficult to maintain long-term. Research demonstrates that individuals who lose weight gradually are more likely to keep it off compared to those who pursue crash diets or extreme calorie restriction. Rapid weight loss can also lead to adverse effects including fatigue, irritability, hair loss, gallstones, and loss of lean muscle mass, which is metabolically active tissue that helps maintain your resting energy expenditure.
Key principles of safe weight loss include:
-
Creating a moderate calorie deficit (typically 500-600 kcal per day)
-
Preserving lean muscle mass through adequate protein intake and resistance exercise
-
Ensuring nutritional adequacy across all food groups
-
Establishing sustainable behavioural changes rather than temporary restrictions
It is important to set realistic expectations. A person with a BMI over 30 may initially lose weight more quickly than someone closer to a healthy weight range. For people of South Asian, Black, and some other minority ethnic groups, health risks may occur at lower BMI thresholds (overweight at BMI ≥23 kg/m²; obesity at ≥27.5 kg/m²).
Individual factors such as age, sex, metabolic rate, medication use (including corticosteroids, antipsychotics, and some antidepressants), and underlying health conditions all influence the rate of weight loss. If you have concerns about your weight or underlying health conditions affecting your ability to lose weight, consult your GP for personalised advice and to rule out conditions such as hypothyroidism or polycystic ovary syndrome that may impact metabolism.
Important safety note: If you experience unintentional weight loss, night sweats, persistent fevers, rectal bleeding, difficulty swallowing, or persistent vomiting, seek urgent medical assessment. Weight loss approaches are not suitable during pregnancy or breastfeeding, and those with a history of eating disorders should seek GP advice before attempting weight loss.
Evidence-Based Strategies to Accelerate Weight Loss
Whilst maintaining safety parameters, certain evidence-based strategies can optimise the rate of weight loss within healthy limits. Increasing protein intake may help enhance satiety and preserve lean muscle mass during calorie restriction. Research suggests that higher protein intakes (around 1.2 to 1.6 grams of protein per kilogram of body weight) may support weight management efforts, though this exceeds the UK Reference Nutrient Intake of approximately 0.75g/kg/day. Good protein sources include lean meats, fish, eggs, legumes, and low-fat dairy products. If you have kidney disease or other health conditions, consult your GP or a dietitian before significantly increasing protein intake.
Incorporating resistance training alongside cardiovascular exercise is crucial for maintaining metabolic rate during weight loss. Muscle tissue is metabolically active, burning more calories at rest than fat tissue. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity aerobic activity weekly, combined with strength exercises on two or more days. High-intensity interval training (HIIT) has also demonstrated effectiveness in promoting fat loss whilst preserving muscle mass, though it may not be suitable for everyone, particularly those with cardiovascular conditions. Seek medical advice before starting vigorous exercise if you have significant health conditions or experience concerning symptoms such as chest pain, unexplained breathlessness, or dizziness.
Optimising sleep and managing stress may influence appetite and weight regulation. Research suggests that poor sleep (less than 7 hours nightly) may affect hormones that regulate appetite, potentially increasing hunger and cravings. Similarly, chronic stress may influence eating behaviours and food choices, often leading to consumption of energy-dense foods.
Mindful eating practices can help reduce overall calorie intake without feeling deprived. This includes eating slowly, recognising hunger and fullness cues, minimising distractions during meals, and being aware of emotional eating triggers. Keeping a food diary, whether written or using a smartphone application such as the NHS Better Health app, can improve awareness of eating patterns and portion sizes, supporting weight management efforts.
NHS-Recommended Diet and Exercise Approaches
The NHS promotes several structured approaches to weight management, with the NHS Weight Loss Plan being freely available online. This 12-week programme provides evidence-based guidance on creating a calorie deficit whilst maintaining nutritional balance. For most adults, this involves consuming approximately 1,900 kcal daily for men and 1,400 kcal for women, though individual requirements vary based on age, height, weight, and activity level.
The Eatwell Guide forms the foundation of NHS dietary recommendations, emphasising:
-
At least five portions of varied fruit and vegetables daily
-
Basing meals on wholegrain starchy carbohydrates (brown rice, wholemeal bread, oats)
-
Including lean proteins, fish, beans, and pulses
-
Choosing unsaturated fats in small amounts
-
Limiting foods high in fat, salt, and sugar
-
Staying well hydrated with water, lower-fat milk, and sugar-free drinks
Very low-calorie diets (VLCDs) of 800 kcal or fewer per day may be recommended by healthcare professionals for individuals with a BMI over 30, particularly those with type 2 diabetes or other obesity-related conditions. These programmes, such as those following the NHS Low Calorie Diet programme, must be medically supervised and typically involve total diet replacement products for 8 to 12 weeks, followed by gradual food reintroduction. VLCDs are not suitable during pregnancy or breastfeeding, for children, some older or frail adults, or those with certain medical conditions. NICE guidance supports this approach for appropriate candidates, as it can produce rapid initial weight loss and improvements in metabolic health markers.
Regarding physical activity, the NHS recommends building up gradually if you are currently inactive. Start with activities you enjoy, whether walking, swimming, cycling, or dancing. Incidental activity throughout the day—taking stairs, walking during lunch breaks, or doing household chores vigorously—contributes meaningfully to total energy expenditure. For those with mobility limitations or health conditions, chair-based exercises or water-based activities may be more appropriate. Seek medical advice before starting exercise if you have concerning symptoms (chest pain, unexplained breathlessness, dizziness) or significant long-term conditions.
Medical Support and Prescription Weight Loss Options
When lifestyle modifications alone prove insufficient, medical interventions may be appropriate for eligible individuals. NICE guidelines recommend considering pharmacological treatment for adults with obesity, with specific criteria for each medication.
Orlistat is available both on prescription and over-the-counter (as Alli at a lower dose, only for those with BMI ≥28 kg/m²). This medication works by inhibiting pancreatic lipase, an enzyme that breaks down dietary fats, thereby reducing fat absorption by approximately 30%. Common adverse effects include oily stools, faecal urgency, and flatulence, particularly when consuming high-fat meals. Orlistat may also reduce absorption of fat-soluble vitamins (A, D, E, K), so a multivitamin supplement taken at bedtime (at least two hours apart from the medication) is often recommended. Treatment should only continue beyond three months if at least 5% weight loss has been achieved (or six months for people with type 2 diabetes). Orlistat may interact with certain medications including ciclosporin and warfarin, so always inform your healthcare provider about all medicines you take.
GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda) represent newer pharmacological options. These medications mimic the action of glucagon-like peptide-1, a hormone that regulates appetite and food intake. They work by slowing gastric emptying, increasing satiety, and reducing hunger signals. Administered via weekly (semaglutide) or daily (liraglutide) subcutaneous injection, these medications have demonstrated significant weight loss in clinical trials. Common adverse effects include nausea, vomiting, diarrhoea, and constipation, which often improve over time. These medications are currently recommended by NICE for specific populations with restricted criteria and are prescribed through specialist weight management services. For liraglutide, treatment should be stopped if 5% weight loss is not achieved after 12 weeks at the 3mg dose. For semaglutide, reassessment typically occurs around 20 weeks. Cautions include risks of gallbladder disease, pancreatitis, and dehydration, and use during pregnancy or breastfeeding is not recommended.
Bariatric surgery may be considered for individuals with a BMI of 40 kg/m² or above, or 35 kg/m² with significant obesity-related conditions who have not achieved adequate weight loss through other methods. Lower BMI thresholds may apply for metabolic surgery in people with type 2 diabetes. Procedures such as gastric bypass or sleeve gastrectomy alter the digestive system to restrict food intake and, in some cases, reduce nutrient absorption. Referral to a specialist weight management service is essential for comprehensive assessment, as surgery requires lifelong dietary modifications, nutritional supplementation, and follow-up care.
If you believe you may benefit from medical weight loss interventions, discuss this with your GP, who can assess your eligibility and provide appropriate referrals. If you experience any suspected side effects from weight loss medications, report them through the MHRA Yellow Card Scheme.
Common Mistakes That Slow Weight Loss Progress
Understanding common pitfalls can help you avoid frustration and maintain steady progress. Underestimating calorie intake is perhaps the most frequent obstacle. Research suggests that people often underestimate their food consumption, particularly with calorie-dense foods like oils, nuts, cheese, and condiments. Portion sizes have increased substantially over recent decades, and what appears to be a single serving may actually constitute two or three. Using measuring cups, kitchen scales, or reliable tracking applications can provide more accurate awareness of actual intake.
Over-relying on exercise alone without addressing dietary habits rarely produces significant weight loss. Whilst physical activity is crucial for health and helps maintain weight loss, it is relatively easy to consume more calories than you burn through exercise. For example, a 30-minute jog might burn 300 calories, which can be quickly negated by a single chocolate bar or large latte. The most effective approach combines both increased physical activity and mindful calorie reduction.
Inconsistent adherence significantly impacts results. Many people maintain strict dietary control during weekdays but substantially increase intake at weekends, effectively negating much of their weekly deficit. Similarly, abandoning healthy habits during holidays, celebrations, or stressful periods can stall progress. Whilst occasional flexibility is important for sustainability, frequent "cheat days" or "treat meals" can substantially reduce your overall calorie deficit.
Expecting linear progress leads to unnecessary discouragement. Weight fluctuates daily due to factors including hydration status, sodium intake, hormonal changes (particularly in menstruating women), bowel movements, and glycogen storage. These fluctuations can mask fat loss on the scales. The NHS recommends weighing yourself no more than once a week, at the same time of day. Taking body measurements, noting how clothing fits, and tracking non-scale victories (improved energy, better sleep, enhanced fitness) provide a more complete picture of progress.
Neglecting adequate recovery through insufficient sleep, excessive training without rest days, or chronic stress can impair weight loss by disrupting hormonal balance and increasing inflammation. Alcohol consumption is another common obstacle, as alcoholic drinks can be high in calories and may reduce inhibitions around food choices.
If weight loss has stalled despite adherence to your plan, or if you experience symptoms such as persistent fatigue, hair loss, menstrual irregularities, or mood changes, consult your GP to rule out underlying conditions and receive personalised guidance. Remember that unintentional weight loss, particularly when accompanied by other symptoms, requires prompt medical assessment.
Frequently Asked Questions
What is the safest rate to lose weight?
The NHS recommends losing 0.5 to 1 kilogram (1 to 2 pounds) per week, which is considered both safe and sustainable whilst minimising risks of nutritional deficiencies and muscle loss.
Can exercise alone help me lose weight faster?
Exercise is crucial for health and maintaining weight loss, but dietary modifications are essential for creating the calorie deficit needed for weight loss. The most effective approach combines both increased physical activity and mindful calorie reduction.
When should I consider medical weight loss treatments?
Medical interventions such as orlistat or GLP-1 receptor agonists may be appropriate when lifestyle modifications alone prove insufficient, typically for individuals meeting specific BMI criteria. Discuss eligibility with your GP for proper assessment and referral.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












