Headaches are a commonly reported side effect when starting GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Understanding how to get rid of GLP-1 headache symptoms can significantly improve your treatment experience. Most headaches occur during initial weeks or following dose increases and typically diminish as your body adapts. This article provides evidence-based strategies for managing GLP-1-related headaches, from immediate relief measures to long-term prevention, whilst highlighting when medical review becomes necessary. Effective headache management allows you to continue benefiting from these important diabetes and weight management medicines.
Summary: GLP-1 headaches typically resolve with adequate hydration, over-the-counter painkillers like paracetamol, rest, and maintaining regular small meals during the initial treatment adjustment period.
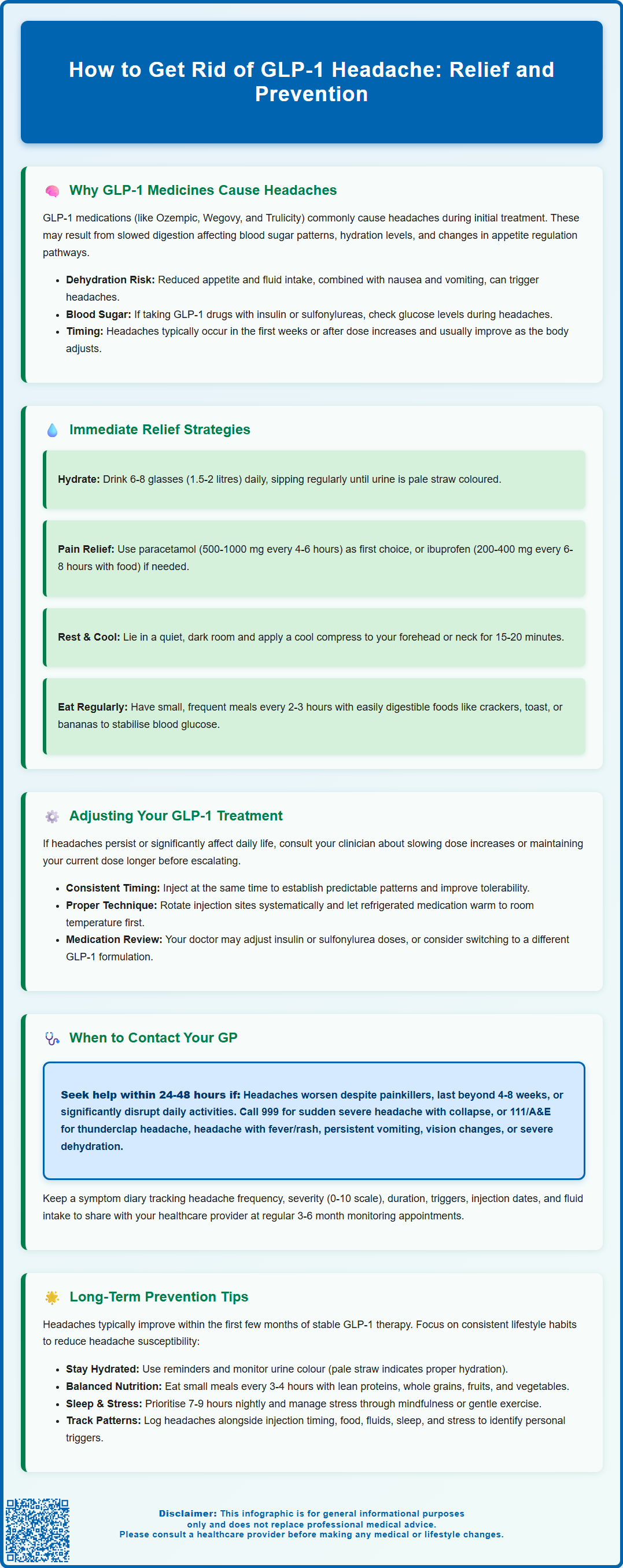
- GLP-1 receptor agonists (semaglutide, dulaglutide, liraglutide) commonly cause headaches during initial weeks or after dose escalation due to altered gastric emptying, hydration changes, and metabolic adjustments.
- First-line management includes drinking 1.5–2 litres of fluids daily, using paracetamol (maximum 4 g daily) or ibuprofen (maximum 1.2 g daily for over-the-counter use) as appropriate, and resting in a quiet environment.
- Slower dose titration, consistent injection timing, proper site rotation, and small frequent meals may reduce headache frequency and severity.
- Seek urgent medical attention for sudden severe headache, headache with fever or visual changes, persistent vomiting, or symptoms suggesting pancreatitis or severe dehydration.
- Most GLP-1 headaches improve within the first few months of stable therapy; persistent symptoms beyond 4–8 weeks warrant GP review to exclude other causes and optimise treatment.
Table of Contents
Why GLP-1 Medicines Cause Headaches
Glucagon-like peptide-1 (GLP-1) receptor agonists — including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda) — are increasingly prescribed for type 2 diabetes management and weight loss. Headaches are among the commonly reported side effects during the initial treatment phase, with frequency varying between different GLP-1 medicines according to their Summary of Product Characteristics.
The precise mechanism behind GLP-1-induced headaches remains incompletely understood, though several physiological factors may contribute. GLP-1 receptor agonists alter gastric emptying, slowing the rate at which food moves through the digestive system. This can lead to changes in blood glucose patterns and hydration status, both of which may trigger headache symptoms. Additionally, these medicines may influence central nervous system pathways involved in appetite regulation.
Changes in hydration may be a contributing factor. Many patients experience reduced appetite and fluid intake when starting GLP-1 therapy, whilst the medicine's gastrointestinal effects — including nausea and occasional vomiting — can further affect hydration status. The combination of altered eating patterns, potential fluid loss, and metabolic adjustments may create conditions conducive to headache development.
If you're taking GLP-1 medicines alongside insulin or sulfonylureas, it's important to check your blood glucose levels when experiencing headaches, as hypoglycaemia (low blood sugar) can also cause headache symptoms.
It is important to note that headaches typically emerge during the initial weeks of treatment or following dose escalation. Most patients find these symptoms diminish as their body adapts to the medicine, often during the titration period. However, persistent or severe headaches warrant medical review to exclude other causes and ensure appropriate management.
Immediate Relief Strategies for GLP-1 Headaches
When experiencing a GLP-1-related headache, several evidence-based approaches can provide prompt relief whilst maintaining treatment safety. Hydration should be your first priority. Aim to drink enough fluids throughout the day to keep your urine a pale straw colour. For most adults, this typically means 6-8 glasses (1.5-2 litres) of fluid daily, sipping regularly rather than consuming large volumes at once. If you have heart or kidney disease or are on fluid restriction, follow your healthcare professional's specific guidance about fluid intake.
Over-the-counter painkillers remain appropriate for managing GLP-1 headaches when used according to package instructions. Paracetamol (500–1000 mg every 4–6 hours, maximum 4 g daily) represents a safe first-line option for most patients. Use with caution if you have liver disease or regularly drink alcohol. Ibuprofen (200–400 mg every 6–8 hours with food, maximum 1.2 g daily for over-the-counter use) may be used if paracetamol proves insufficient, provided you have no contraindications such as kidney disease, cardiovascular conditions, gastric ulcer history, or pregnancy (especially after 20 weeks). Always check with your pharmacist about drug interactions with your other medicines, particularly if you take anticoagulants or have asthma. To avoid medication-overuse headache, limit regular use of painkillers to no more than 10 days per month.
Rest in a quiet, darkened environment can significantly alleviate headache intensity. Apply a cool compress to your forehead or the back of your neck for 15–20 minutes. Some patients find gentle neck stretches and shoulder rolls helpful for tension-related components of their headache.
Small, frequent meals may help stabilise blood glucose levels and reduce headache triggers. Even if your appetite is diminished, try consuming easily digestible foods such as plain crackers, toast, or bananas every 2–3 hours. Avoid skipping meals entirely, as this can exacerbate both headaches and other GLP-1 side effects. If you have diabetes and take insulin or sulfonylureas alongside your GLP-1 medicine, check your blood glucose levels during headaches to rule out hypoglycaemia. If nausea accompanies your headache, ginger tea or peppermint may provide additional symptomatic relief.
Adjusting Your GLP-1 Treatment to Reduce Headaches
If headaches persist beyond the initial adjustment period or significantly impact your quality of life, discuss dose modification strategies with your prescribing clinician. GLP-1 medicines typically follow a gradual titration schedule, but some patients benefit from a slower escalation. Your GP or diabetes specialist nurse may recommend delaying dose increases by an additional 4 weeks or maintaining your current dose for longer, following the specific guidance in your medicine's information leaflet.
Timing of administration can influence side effect profiles. Whilst most GLP-1 receptor agonists are administered weekly (semaglutide, dulaglutide) or daily (liraglutide), maintaining consistency with injection timing helps establish predictable patterns and may improve overall tolerability. Some patients anecdotally report differences in side effects based on time of day of injection, though this isn't established in clinical evidence.
Injection technique and site rotation warrant attention. Ensure you're following the manufacturer's instructions for injecting into subcutaneous tissue (typically the abdomen, thigh, or upper arm). Rotate injection sites systematically as recommended in your medicine's information leaflet. Follow the specific storage instructions for your GLP-1 medicine, including any recommendations about allowing refrigerated medicine to reach room temperature before injecting.
If you're taking insulin or sulfonylureas alongside your GLP-1 medicine, your healthcare provider may need to adjust these doses to reduce the risk of hypoglycaemia, which can itself cause headaches.
In some cases, switching between GLP-1 formulations may prove beneficial. Different medicines within this class have varying receptor binding profiles and pharmacokinetic properties. For instance, patients experiencing persistent headaches with one GLP-1 medicine might tolerate another differently. Such decisions require careful discussion with your healthcare provider, considering your diabetes control, weight management goals, and overall side effect profile. Never adjust your prescribed regimen without medical guidance.
When to Contact Your GP About GLP-1 Side Effects
Whilst mild headaches commonly accompany GLP-1 therapy initiation, certain presentations require prompt medical assessment. Contact your GP within 24–48 hours if you experience headaches that progressively worsen despite simple painkillers, persist beyond 4–8 weeks of stable dosing, or significantly interfere with daily activities. Headaches accompanied by visual disturbances, confusion, or neck stiffness warrant same-day medical review to exclude serious neurological conditions.
Call 999 for life-threatening symptoms such as sudden severe headache with collapse or focal neurological deficits.
Seek urgent medical attention (contact 111 or attend A&E) if you develop:
-
Severe, sudden-onset headache ("thunderclap" pattern) unlike any previous headache
-
Headache with fever, rash, or altered consciousness
-
Persistent vomiting preventing fluid intake or medicine absorption
-
Visual changes including double vision, blind spots, or temporary vision loss
-
Signs of severe dehydration (dark urine, dizziness on standing, reduced urination)
-
Symptoms suggesting pancreatitis (severe upper abdominal pain radiating to the back)
-
Symptoms suggesting gallbladder problems (right upper abdominal pain, fever, yellowing of skin/eyes)
Your healthcare provider needs to assess whether headaches represent a straightforward medicine side effect or indicate a more complex issue. Bring a symptom diary to your appointment, documenting headache frequency, severity (rated 0–10), duration, associated symptoms, and any relieving or aggravating factors. Note your injection dates, dose changes, and fluid intake patterns.
NICE guidance recommends regular monitoring for patients on GLP-1 therapy, typically including HbA1c measurements every 3–6 months and assessment of treatment tolerability. Use these scheduled reviews to discuss any persistent side effects. Your clinician may consider alternative diabetes or weight management strategies if headaches prove intractable despite optimisation efforts. Remember that effective diabetes management requires balancing glycaemic control benefits against quality of life considerations.
Long-Term Management and Prevention Tips
Establishing consistent hydration habits represents the cornerstone of headache prevention during GLP-1 therapy. Set regular reminders to drink water throughout the day, particularly if reduced thirst sensation accompanies your treatment. Keep a water bottle accessible and aim to consume fluids before you feel thirsty. Monitor your urine colour — pale straw indicates adequate hydration, whilst dark yellow suggests insufficient fluid intake. If you have heart or kidney disease or are on fluid restriction, follow your healthcare professional's specific guidance.
Nutritional strategies support headache prevention whilst accommodating GLP-1-induced appetite changes. Despite reduced hunger, maintain regular eating patterns with small, balanced meals every 3–4 hours. Focus on nutrient-dense foods including lean proteins, whole grains, fruits, and vegetables. Avoid prolonged fasting periods, as blood glucose fluctuations can trigger headaches. Some patients find that consuming a small protein-rich snack before their weekly injection helps minimise subsequent side effects, though this is based on personal experience rather than clinical evidence.
Lifestyle modifications complement pharmaceutical management. Ensure adequate sleep (7–9 hours nightly), as sleep deprivation independently increases headache susceptibility. Manage stress through evidence-based techniques such as mindfulness meditation, progressive muscle relaxation, or gentle exercise like walking or swimming. Regular physical activity improves overall GLP-1 treatment outcomes whilst potentially reducing headache frequency.
Keep a comprehensive symptom log tracking headaches alongside other variables: injection timing, food intake, fluid consumption, sleep quality, stress levels, and menstrual cycle (if applicable). Patterns often emerge that help identify personal triggers and effective prevention strategies. Share this information with your healthcare team to inform treatment optimisation.
Many patients find headaches improve over the first few months of stable GLP-1 therapy. The substantial benefits these medicines provide for diabetes control and weight management typically outweigh temporary side effects. However, individualised care remains paramount — your healthcare provider can help balance treatment efficacy against tolerability, ensuring your medicine regimen supports both metabolic health and quality of life. Regular follow-up enables timely adjustments and ensures you receive maximum benefit from your prescribed therapy.
If you suspect an adverse reaction to your GLP-1 medicine, you can report it through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
Scientific References
- GLP-1 receptor agonists: reports of diabetic ketoacidosis when concomitant insulin was rapidly reduced or discontinued.
- GLP-1 medicines for weight loss and diabetes: what you need to know.
- Ozempic: European Public Assessment Report.
- GLP-1 receptor agonists: reminder of the potential side effects and to be aware of the potential for misuse.
- Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain.
- Glucagon-Like Peptide-1 Receptor Agonists.
Frequently Asked Questions
How long do GLP-1 headaches typically last?
Most GLP-1 headaches occur during the initial weeks of treatment or following dose increases and typically diminish as your body adapts to the medicine, often within the first few months of stable therapy. Headaches persisting beyond 4–8 weeks of stable dosing warrant medical review.
Can I take paracetamol or ibuprofen for GLP-1 headaches?
Yes, over-the-counter painkillers are appropriate for managing GLP-1 headaches. Paracetamol (maximum 4 g daily) is a safe first-line option for most patients, whilst ibuprofen (maximum 1.2 g daily for over-the-counter use) may be used if paracetamol proves insufficient, provided you have no contraindications such as kidney disease or gastric ulcer history.
When should I contact my GP about GLP-1 headaches?
Contact your GP within 24–48 hours if headaches progressively worsen despite simple painkillers, persist beyond 4–8 weeks of stable dosing, or significantly interfere with daily activities. Seek urgent medical attention for sudden severe headache, headache with fever or visual changes, persistent vomiting, or symptoms suggesting serious complications.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript