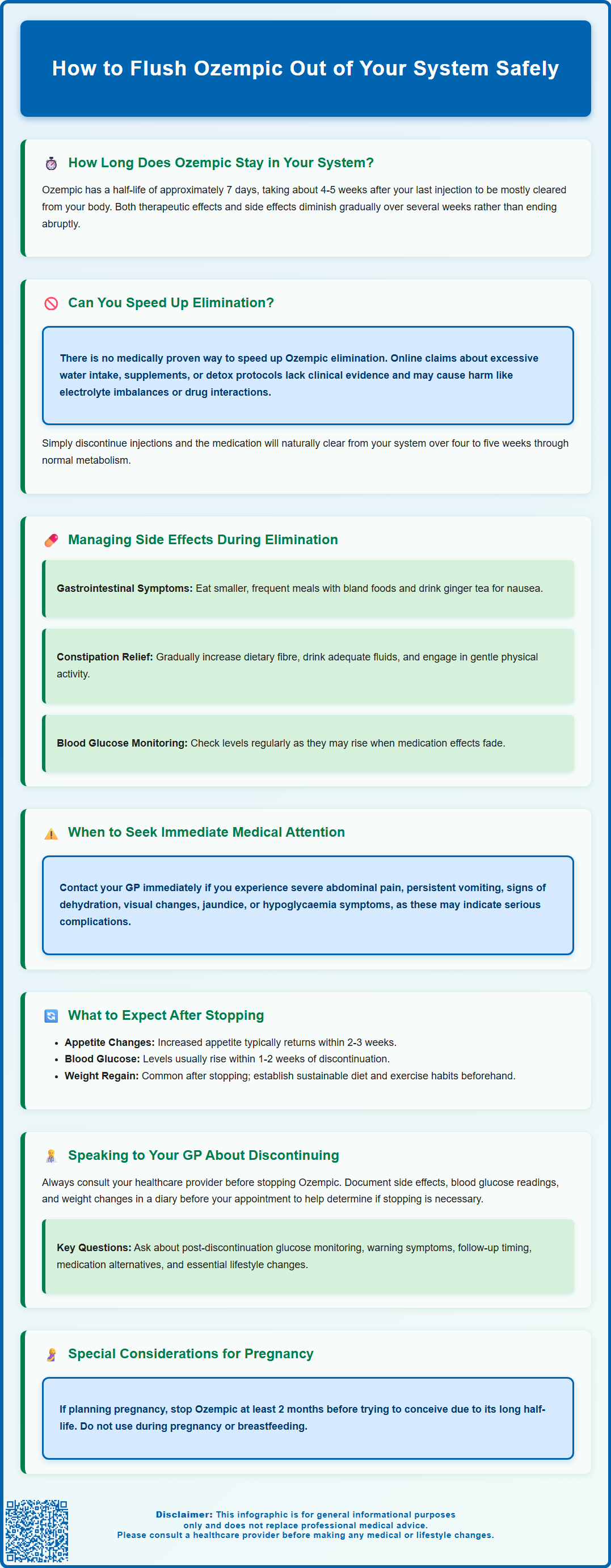
Ozempic (semaglutide) is a once-weekly injectable medication used to treat type 2 diabetes in the UK. If you're wondering how to flush Ozempic out of your system, it's important to understand that there is no medical method to accelerate its elimination. Semaglutide has a long half-life of approximately one week, meaning it takes around four to five weeks after your last injection for the medication to be mostly cleared from your body through natural metabolic processes. This article explains how Ozempic is eliminated, what to expect when stopping treatment, and how to manage the transition safely under medical supervision.
Summary: Ozempic cannot be flushed out of your system quickly; it must be eliminated naturally over approximately four to five weeks after your last injection.
- Semaglutide is a GLP-1 receptor agonist with a one-week half-life, requiring natural metabolic breakdown through proteolytic degradation.
- No clinical evidence supports methods to accelerate elimination; hydration and unproven supplements do not meaningfully alter clearance rates.
- Side effects may persist for several weeks during elimination, with blood glucose levels typically rising within one to two weeks of stopping.
- Discontinuation should be discussed with your GP to adjust diabetes management, monitor blood glucose, and prevent complications.
- Pregnant women or those planning pregnancy should stop semaglutide at least two months before conception due to its extended half-life.
Table of Contents
How Long Does Ozempic Stay in Your System?
Ozempic (semaglutide) has a notably long half-life, which determines how long the medication remains active in your body. The half-life of Ozempic is approximately one week (around 7 days), meaning it takes this amount of time for half of the drug to be eliminated from your system. Due to this extended half-life, it typically takes about 4-5 weeks after your last injection for Ozempic to be mostly cleared from your body, though this can vary between individuals.
Several factors can influence elimination time, including your individual physiology, age, and the dose you were taking. According to the UK product information, no dose adjustment is required for patients with renal or hepatic impairment, or based on age or body weight, as these factors have no clinically relevant effect on semaglutide's pharmacokinetics.
The gradual decline in semaglutide levels means that both the therapeutic effects and any side effects will diminish progressively over several weeks rather than stopping abruptly. This pharmacokinetic profile is important when planning discontinuation, as you'll need to account for this extended washout period when considering alternative diabetes management strategies or if you're experiencing adverse effects.
It's worth noting that in the UK, Ozempic is licensed specifically for the treatment of type 2 diabetes, while Wegovy (also semaglutide, but at different doses) is licensed for weight management.
Can You Speed Up Ozempic Elimination from Your Body?
There is no official medical method to 'flush' Ozempic out of your system more quickly. Unlike some medications, semaglutide must be metabolised and eliminated naturally through your body's normal processes. The drug is broken down into smaller amino acid components through proteolytic degradation, with the resulting metabolites eliminated via urine and faeces.
Claims about accelerating elimination should be viewed with caution. You may encounter suggestions online about drinking excessive water, taking certain supplements, or following detox protocols, but there is no clinical evidence supporting these approaches for Ozempic elimination. Staying well-hydrated is always sensible for general health, but it won't meaningfully alter the drug's half-life or clearance rate.
Your liver and kidneys naturally process the medication at a rate determined by your individual physiology. Semaglutide is highly protein-bound and is not expected to be removed by dialysis. Attempting to interfere with this process could potentially be harmful. For instance, excessive fluid intake can lead to electrolyte imbalances, whilst unproven supplements may interact with other medications or cause adverse effects of their own.
If you're experiencing troublesome side effects and wish to stop Ozempic, the most appropriate approach is to simply discontinue the injections and allow the natural elimination process to occur. The medication will gradually leave your system over the subsequent four to five weeks. During this time, you should work closely with your GP or diabetes specialist to:
-
Monitor your blood glucose levels carefully
-
Adjust other diabetes medications as needed
-
Implement alternative management strategies
-
Address any persistent side effects
Patience is essential, as rushing the process isn't medically possible and attempting unproven methods may introduce additional risks.
Managing Side Effects While Ozempic Leaves Your System
As Ozempic gradually leaves your system, you may continue experiencing side effects for several weeks, though these typically diminish in intensity over time. The most common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These occur because semaglutide slows gastric emptying, and this effect persists whilst the drug remains in your circulation.
Practical strategies can help manage lingering side effects during the elimination period. For nausea and gastrointestinal upset, consider eating smaller, more frequent meals rather than large portions. Bland, easily digestible foods may be better tolerated. Ginger tea may provide natural relief for nausea. If considering any supplements, always check with your GP or pharmacist first as they may interact with other medications. Staying well-hydrated is particularly important if you're experiencing vomiting or diarrhoea, as dehydration can worsen how you feel and affect blood glucose control.
For constipation, which affects some patients, increasing dietary fibre gradually, maintaining adequate fluid intake, and gentle physical activity can be beneficial. If symptoms are severe, your GP may recommend appropriate laxatives. Conversely, if diarrhoea is problematic, anti-diarrhoeal medications may be suggested, but avoid self-medicating without professional advice.
Monitor for more serious symptoms that require prompt medical attention. Contact your GP urgently, call NHS 111, or go to A&E if you experience:
-
Severe, persistent abdominal pain (potential pancreatitis)
-
Right upper abdominal pain, fever or jaundice (possible gallbladder disease)
-
Persistent vomiting preventing fluid intake
-
Signs of dehydration or reduced urine output (possible acute kidney injury)
-
Visual changes or eye symptoms (especially if you have diabetic retinopathy)
-
Symptoms of hypoglycaemia (particularly if taking insulin or sulfonylureas)
Your blood glucose levels may rise as Ozempic's effects wane, particularly if you have type 2 diabetes. Regular monitoring becomes crucial during this transition period, and your healthcare team should provide guidance on adjusting other medications or implementing lifestyle modifications to maintain glycaemic control.
If you experience any adverse effects, you can report them through the MHRA Yellow Card scheme.
When to Stop Ozempic and What to Expect
The decision to discontinue Ozempic should ideally be made in consultation with your healthcare provider, though there are circumstances where stopping may be necessary or appropriate. Valid reasons for discontinuation include intolerable side effects, pregnancy or planning pregnancy, development of certain medical conditions, inadequate therapeutic response, or personal choice.
If you're planning pregnancy, the UK product information recommends stopping semaglutide at least 2 months before trying to conceive due to its long half-life. Semaglutide should not be used during pregnancy or breastfeeding.
If you're stopping due to side effects, it's worth noting that many gastrointestinal symptoms improve over time as your body adjusts. The product information recommends starting at a lower dose and titrating slowly to minimise adverse effects. However, if side effects remain unacceptable despite dose adjustments, discontinuation is reasonable. Some patients find that symptoms which were tolerable initially become more burdensome over time, and this is a valid reason to reconsider treatment.
When you stop Ozempic, expect gradual changes rather than immediate effects. The medication's glucose-lowering and appetite-suppressing effects will diminish progressively over four to five weeks. Many patients notice increased appetite returning within two to three weeks, which can be challenging if weight management was a treatment goal. Blood glucose levels typically begin rising within one to two weeks after the last dose, though the timeline varies individually.
Weight regain may occur after stopping Ozempic, particularly if lifestyle modifications haven't been established. Research from clinical trials of semaglutide for obesity (at the higher 2.4mg dose used in Wegovy) indicates that patients may regain a significant portion of lost weight within months of discontinuation. This isn't a failure—it reflects the medication's physiological effects on appetite regulation and metabolism. To mitigate weight regain:
-
Establish sustainable dietary changes before stopping
-
Maintain regular physical activity
-
Consider working with a dietitian
-
Discuss alternative weight management strategies with your GP
For diabetes management, your healthcare team will need to adjust your treatment plan. This might involve optimising other oral medications, considering alternative injectable therapies, or intensifying lifestyle interventions. Regular HbA1c monitoring will help assess whether your revised management strategy maintains adequate glycaemic control.
Speaking to Your GP About Discontinuing Ozempic
Open communication with your GP is essential when considering stopping Ozempic. Rather than discontinuing abruptly without medical input, scheduling a consultation allows for proper planning and ensures continuity of care for your diabetes or weight management. Your GP needs to understand your reasons for wanting to stop, whether due to side effects, lifestyle factors, or treatment goals being met.
Prepare for your appointment by documenting specific concerns. Keep a symptom diary noting the frequency and severity of any side effects, record your recent blood glucose readings if you have diabetes, and note any changes in weight or eating patterns. This information helps your GP assess whether discontinuation is appropriate or if alternative solutions might address your concerns. For instance, dose reduction rather than complete cessation might resolve side effects whilst maintaining some therapeutic benefit.
Your GP will need to discuss several important considerations with you. These include how to monitor for rising blood glucose levels after stopping, what alternative diabetes medications might be appropriate, strategies to prevent weight regain if that's a concern, and the timeline for follow-up appointments. If you have type 2 diabetes, your GP may need to adjust other medications—potentially increasing doses of metformin or other oral agents, or considering different injectable options.
Questions to ask your GP include:
-
How should I monitor my blood glucose after stopping?
-
What symptoms should prompt me to seek urgent advice?
-
When should I schedule follow-up appointments?
-
Are there alternative medications we should consider?
-
What lifestyle modifications are most important now?
-
Should I see a diabetes specialist nurse or dietitian?
Be honest about your concerns and expectations. If side effects are the problem, there may be management strategies you haven't tried. If you're concerned about continuing treatment, your GP can explain the NHS prescribing guidelines, availability of alternatives, and any applicable prescription charges or exemptions.
Remember that stopping Ozempic doesn't mean abandoning your health goals—it simply means finding an approach that works better for your individual circumstances. Your GP is there to support you in making informed decisions about your treatment and ensuring safe transitions between therapies.
If you experience concerning symptoms after stopping Ozempic, contact your GP, call NHS 111 for urgent advice, or go to A&E/call 999 for severe symptoms.
Frequently Asked Questions
How long does it take for Ozempic to completely leave your body?
It takes approximately four to five weeks after your last injection for Ozempic to be mostly cleared from your system, as semaglutide has a half-life of about one week and must be eliminated through natural metabolic processes.
Can drinking more water help flush Ozempic out faster?
No, drinking excessive water will not speed up Ozempic elimination. Semaglutide is highly protein-bound and metabolised through proteolytic degradation at a rate determined by your individual physiology, which cannot be meaningfully altered by hydration.
What should I do if I want to stop taking Ozempic?
Consult your GP before stopping Ozempic to discuss alternative diabetes management strategies, monitor blood glucose levels during the transition, and manage any side effects safely. Simply discontinuing injections allows natural elimination over four to five weeks.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript