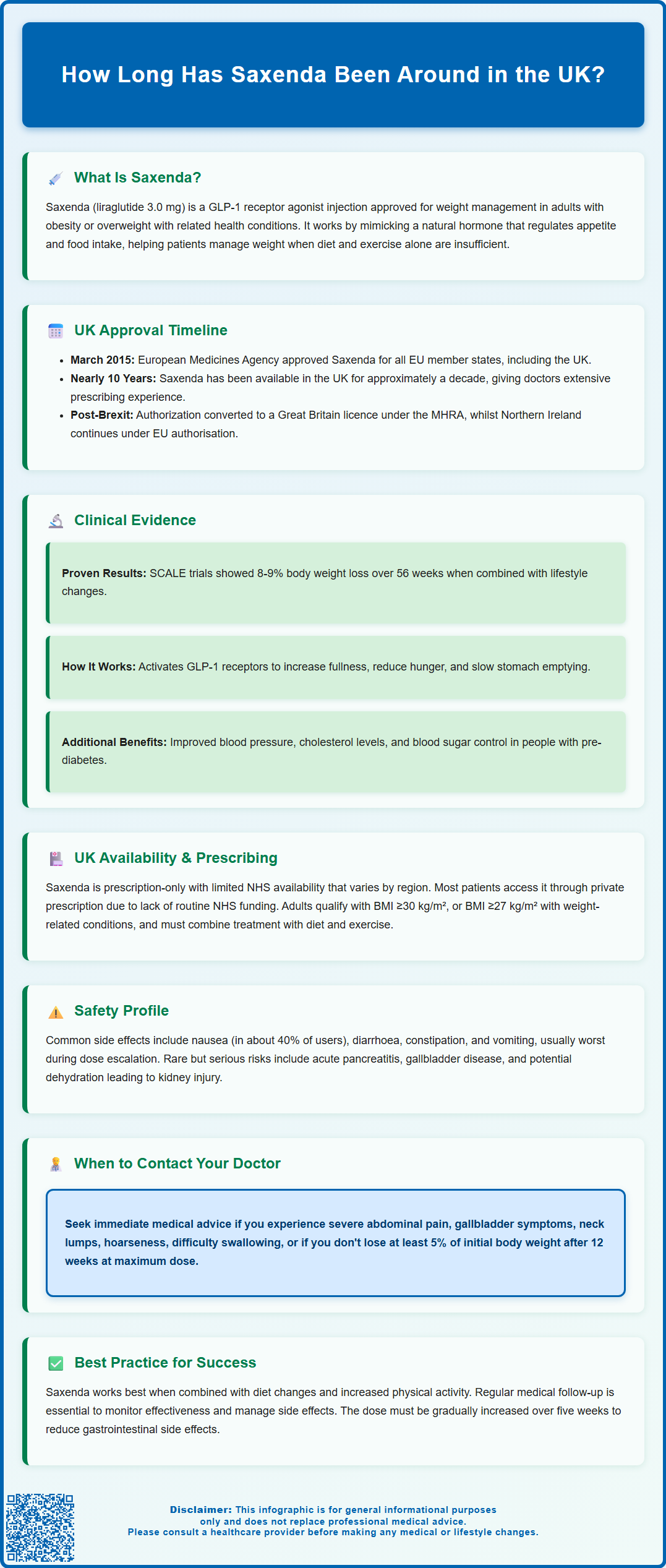
Saxenda (liraglutide 3.0 mg) has been available in the UK since 2015, providing nearly a decade of clinical experience in weight management. This glucagon-like peptide-1 (GLP-1) receptor agonist was first approved by the US FDA in December 2014, followed by European Medicines Agency authorisation in March 2015. Understanding Saxenda's regulatory timeline and accumulated safety data helps patients and clinicians make informed decisions about this prescription medicine for obesity. This article examines when Saxenda became available, the clinical research supporting its approval, UK prescribing patterns, and the real-world evidence gathered over ten years of use.
Summary: Saxenda has been available for approximately 10 years, receiving FDA approval in December 2014 and EMA approval in March 2015, making it available in the UK since 2015.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist that mimics a natural hormone regulating appetite and food intake.
- The medication was approved based on the SCALE clinical trial programme involving over 5,000 participants demonstrating significant weight loss.
- In the UK, Saxenda is prescription-only with variable NHS availability; many patients access it through private prescription.
- Common side effects include gastrointestinal symptoms (nausea, diarrhoea), typically most pronounced during dose escalation.
- Treatment requires monitoring for rare serious events including pancreatitis, gallbladder disease, and dehydration with renal impairment.
- A decade of post-market surveillance has confirmed the safety profile established in clinical trials without unexpected cardiovascular concerns.
Table of Contents
Introduction to Saxenda and Its History
Saxenda (liraglutide 3.0 mg) is an injectable prescription medicine used for weight management in adults with obesity or those who are overweight with weight-related health conditions. It is also licensed for use in adolescents aged 12 to <18 years with body weight above 60kg and obesity. Saxenda belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking a naturally occurring hormone that regulates appetite and food intake.
The active ingredient, liraglutide, was originally developed by Novo Nordisk for the treatment of type 2 diabetes under the brand name Victoza (at lower doses of up to 1.8 mg daily). Following extensive research demonstrating its effects on weight reduction, a higher-dose formulation was developed specifically for chronic weight management. Saxenda has now been available internationally for over a decade, representing an important pharmacological option for patients struggling with obesity when lifestyle interventions alone prove insufficient.
Understanding how long Saxenda has been available provides valuable context for both patients and healthcare professionals. The medication's history reflects the evolution of obesity treatment from a condition often managed solely through diet and exercise to one where evidence-based pharmacotherapy plays a recognised role. This article explores Saxenda's regulatory timeline, the clinical research underpinning its approval, its availability within the UK healthcare system, and the accumulating real-world safety data that has emerged since its launch.
Regulatory Approval Timeline: When Saxenda Became Available
Saxenda received its first regulatory approval from the United States Food and Drug Administration (FDA) in December 2014, marking a significant milestone in obesity pharmacotherapy. This approval was based on the comprehensive SCALE (Satiety and Clinical Adiposity – Liraglutide Evidence) clinical trial programme, which demonstrated clinically meaningful weight loss in adults with obesity.
In the European Union, the European Medicines Agency (EMA) granted marketing authorisation for Saxenda in March 2015. This approval covered all EU member states, including the United Kingdom (which was an EU member at the time). The EMA's positive opinion was similarly based on the robust clinical trial data showing that liraglutide 3.0 mg, when used alongside a reduced-calorie diet and increased physical activity, produced significant and sustained weight reduction.
Following Brexit, the EU marketing authorisation for Saxenda was converted to a Great Britain licence under the Medicines and Healthcare products Regulatory Agency (MHRA). In Northern Ireland, the medicine remains available under EU authorisation following the Windsor Framework arrangements. Therefore, Saxenda has been available in the UK for around 10 years (since 2015), providing clinicians with a decade of prescribing experience.
It is worth noting that regulatory approval does not automatically translate to widespread NHS availability, as funding and prescribing decisions involve additional considerations through bodies such as the National Institute for Health and Care Excellence (NICE).
Clinical Development and Research Behind Saxenda
The development of Saxenda was underpinned by the SCALE clinical trial programme, which comprised several large, randomised, double-blind, placebo-controlled studies involving over 5,000 participants across multiple countries. These pivotal trials examined liraglutide 3.0 mg in various populations, including adults with obesity, those with pre-diabetes, and individuals who had previously lost weight and required maintenance therapy.
Key findings from the SCALE Obesity and Prediabetes trial demonstrated that participants using Saxenda alongside lifestyle modification achieved an average weight loss of 8-9% of their initial body weight over 56 weeks, compared to approximately 2-3% in the placebo group. Importantly, a significantly higher proportion of Saxenda-treated patients achieved clinically meaningful weight loss thresholds of ≥5% and ≥10% body weight reduction. The trials also showed improvements in cardiovascular risk factors, including blood pressure, lipid profiles, and glycaemic control in those with pre-diabetes.
Additional research supported the extension of Saxenda's indication to include adolescents (12 to <18 years) with obesity, providing an important treatment option for this population.
Mechanism of action: Liraglutide works by activating GLP-1 receptors in the brain's appetite regulation centres, particularly in the hypothalamus. This activation leads to increased feelings of fullness (satiety), reduced hunger, and decreased food intake. Additionally, GLP-1 receptor agonists slow gastric emptying, which contributes to prolonged satiety after meals. The medication is administered once daily via subcutaneous injection, typically in the abdomen, thigh, or upper arm.
Cardiovascular safety has been an important consideration in liraglutide's development. While the LEADER trial examined cardiovascular outcomes with liraglutide 1.8 mg in type 2 diabetes (rather than the 3.0 mg dose used in obesity), it provides important safety information about the molecule, demonstrating cardiovascular safety and potential benefits.
Saxenda's Use in the UK: Availability and Prescribing
In the UK, Saxenda is available as a prescription-only medicine and can be prescribed by GPs, specialist weight management services, and private healthcare providers. There is currently no NICE technology appraisal recommending Saxenda for routine NHS use. NICE obesity guidance (CG189) addresses pharmacological interventions for obesity management, but NHS availability of Saxenda is subject to local commissioning decisions.
Consequently, NHS availability of Saxenda varies considerably across different regions and integrated care boards (ICBs). Some specialist NHS weight management services may prescribe Saxenda in specific circumstances, particularly for patients with significant obesity-related comorbidities where other interventions have been unsuccessful. However, many patients access Saxenda through private prescription, either via private GPs or online prescribing services. UK supply constraints may periodically affect availability.
Prescribing criteria follow the licensed indications: Saxenda is indicated for adults with a body mass index (BMI) of ≥30 kg/m² (obesity), or ≥27 kg/m² (overweight) in the presence of at least one weight-related comorbidity such as type 2 diabetes, hypertension, dyslipidaemia, or obstructive sleep apnoea. For adolescents aged 12 to <18 years, it is indicated for weight management in those with body weight above 60kg and BMI corresponding to ≥30 kg/m² for adults. It should be used as an adjunct to a reduced-calorie diet and increased physical activity.
Treatment should be discontinued if adults have not lost at least 5% of their initial body weight after 12 weeks at the maximum dose (3.0 mg daily). For adolescents, treatment should be re-evaluated if body weight has not decreased by at least 4% BMI after 12 weeks on the 3.0 mg dose.
Patient safety considerations include the need for dose escalation over five weeks to minimise gastrointestinal side effects, contraindications in pregnancy, caution in breastfeeding, and monitoring for dehydration or renal impairment with severe gastrointestinal adverse effects. Saxenda should not be used concurrently with other GLP-1 receptor agonists. Small increases in heart rate may occur. Regular monitoring and follow-up are essential components of safe prescribing practice.
Long-Term Safety Data and Post-Market Experience
With over a decade of post-market experience since 2015, substantial real-world safety data has accumulated for Saxenda, complementing the controlled clinical trial evidence. This extended observation period has provided valuable insights into the medication's safety profile in diverse patient populations and routine clinical practice settings.
Common adverse effects reported with Saxenda include gastrointestinal symptoms such as nausea (affecting approximately 40% of users), diarrhoea, constipation, vomiting, and abdominal discomfort. These effects are typically most pronounced during the dose-escalation phase and often diminish over time. Other frequently reported side effects include headache, dizziness, and injection-site reactions. Most adverse effects are mild to moderate in severity, though they can lead to treatment discontinuation in some patients.
Serious but rare adverse events that have been monitored through pharmacovigilance include acute pancreatitis, gallbladder disease (including cholelithiasis and cholecystitis), and hypoglycaemia (particularly in patients also taking other glucose-lowering medications). The MHRA and EMA continue to monitor safety signals, and product information is updated as new evidence emerges.
There is a theoretical concern about medullary thyroid carcinoma based on rodent studies, though no established link has been found in humans. Patients should be counselled about symptoms of thyroid tumours (such as a lump in the neck, hoarseness, or difficulty swallowing) and advised to seek medical attention if these occur.
Saxenda can cause small increases in heart rate. Severe gastrointestinal adverse reactions may lead to dehydration and potentially acute kidney injury, so patients should be monitored for fluid status, especially when initiating treatment.
Cardiovascular safety has been a particular focus of long-term monitoring. The LEADER trial (examining liraglutide in type 2 diabetes at 1.8 mg) demonstrated cardiovascular safety and potential benefits, providing reassurance about the medication's effects on heart health. Post-marketing surveillance has not identified unexpected cardiovascular safety concerns with Saxenda.
Patient advice: Individuals using Saxenda should contact their GP or healthcare provider if they experience severe or persistent abdominal pain (which could indicate pancreatitis), symptoms of gallbladder problems, signs of thyroid tumours, or any concerning symptoms. Patients should report suspected side effects via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app). Regular follow-up appointments are essential to monitor treatment response, manage side effects, and ensure ongoing appropriateness of therapy. The medication should always be used as part of a comprehensive weight management programme including dietary modification and increased physical activity for optimal outcomes.
Frequently Asked Questions
When was Saxenda first approved for use?
Saxenda received its first regulatory approval from the US FDA in December 2014, followed by European Medicines Agency approval in March 2015, making it available in the UK from 2015 onwards.
Is Saxenda available on the NHS?
NHS availability of Saxenda varies considerably across different regions and integrated care boards. There is no NICE technology appraisal recommending routine NHS use, so many patients access Saxenda through private prescription.
What safety data exists for Saxenda after 10 years of use?
Over a decade of post-market surveillance has confirmed Saxenda's safety profile, with common gastrointestinal side effects and rare serious events including pancreatitis and gallbladder disease. No unexpected cardiovascular safety concerns have emerged during this period.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript