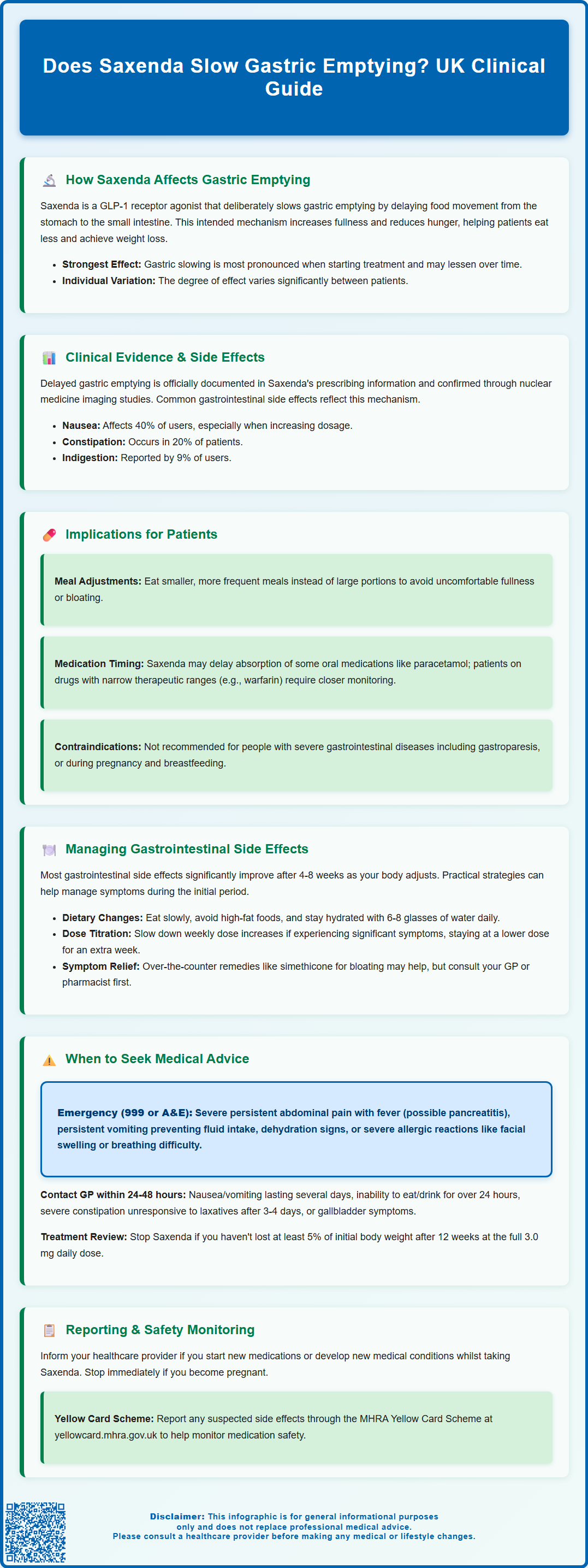
Does Saxenda slow gastric emptying? Yes, Saxenda (liraglutide 3.0 mg) deliberately slows gastric emptying as a key mechanism for weight management. This GLP-1 receptor agonist delays the rate at which food moves from the stomach into the small intestine, increasing feelings of fullness and reducing hunger. Licensed in the UK for adults with obesity or overweight with comorbidities, Saxenda's effect on gastric motility contributes to both its therapeutic benefits and common gastrointestinal side effects. Understanding this mechanism helps patients and healthcare professionals optimise treatment outcomes whilst managing tolerability.
Summary: Yes, Saxenda (liraglutide) deliberately slows gastric emptying by delaying food movement from the stomach to the small intestine, which increases satiety and reduces hunger as part of its weight-loss mechanism.
- Saxenda is a GLP-1 receptor agonist that binds to receptors in the gastrointestinal tract to reduce gastric motility.
- Delayed gastric emptying is most pronounced during initial treatment and may partially attenuate over time with continued use.
- Clinical trials report nausea in approximately 40% of patients, constipation in 20%, and dyspepsia in 9%, particularly during dose escalation.
- Saxenda is contraindicated in patients with severe gastrointestinal disease including gastroparesis, and caution is advised with narrow therapeutic index medications.
- Gradual dose escalation from 0.6 mg to 3.0 mg daily over several weeks improves gastrointestinal tolerability and long-term adherence.
- Patients should seek urgent medical attention for severe persistent abdominal pain, persistent vomiting, or signs of dehydration whilst taking Saxenda.
Table of Contents
How Saxenda Affects Gastric Emptying
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults aged 18 years and over with a BMI ≥30 kg/m² (obesity) or ≥27 kg/m² with at least one weight-related comorbidity. One of its key mechanisms of action involves slowing gastric emptying, which contributes to its weight-loss effects.
GLP-1 is a naturally occurring incretin hormone that regulates appetite and glucose metabolism. When Saxenda binds to GLP-1 receptors in the gastrointestinal tract, it delays the rate at which food moves from the stomach into the small intestine. This physiological effect is an intended therapeutic mechanism that also contributes to common gastrointestinal side effects. By prolonging gastric emptying, Saxenda increases feelings of fullness (satiety) and reduces hunger, helping patients consume fewer calories throughout the day.
The slowing of gastric emptying occurs through several pathways, including effects on the stomach wall and vagal nerve signalling, which coordinates digestive processes. This results in reduced gastric motility. The effect is most pronounced during initial treatment and may attenuate somewhat over time with continued use.
It is important to understand that this delayed gastric emptying is a predictable pharmacological effect of GLP-1 receptor agonists. However, the degree of slowing varies between individuals, and some patients may experience more pronounced effects than others. This variability can influence both the therapeutic benefits and the gastrointestinal tolerability of the medication. Healthcare professionals should counsel patients about this mechanism when initiating Saxenda therapy, as understanding the drug's action can help patients anticipate and manage associated symptoms.
Clinical Evidence on Saxenda and Delayed Gastric Emptying
Clinical evidence confirms that liraglutide delays gastric emptying in both diabetic and non-diabetic populations. Pharmacodynamic studies using techniques such as scintigraphy (a nuclear medicine technique that tracks food movement through the digestive system) have demonstrated measurable reductions in gastric emptying rates following liraglutide administration.
Research shows that liraglutide slows gastric emptying, with the effect being most pronounced during the initial weeks of treatment. Interestingly, some studies suggest that the gastric emptying delay may attenuate over time, though the appetite-suppressing effects often persist. This phenomenon, known as tachyphylaxis, may occur as the body partially adapts to the medication.
The SCALE (Satiety and Clinical Adiposity – Liraglutide Evidence) clinical trial programme, which supported Saxenda's licensing, documented gastrointestinal side effects consistent with delayed gastric emptying. Nausea was reported in approximately 40% of participants, constipation in 20%, and dyspepsia in 9%, particularly during dose escalation. These symptoms typically reflect the medication's effect on gastric motility.
Comparative studies with other GLP-1 receptor agonists suggest that the degree of gastric emptying delay may vary across different agents in this class. Shorter-acting GLP-1 agonists may have more pronounced effects on gastric emptying, whilst longer-acting formulations like liraglutide may have relatively greater effects on appetite centres in the brain.
Regulatory bodies including the MHRA and EMA have reviewed this evidence extensively. The delayed gastric emptying is clearly documented in the Summary of Product Characteristics (SmPC), and healthcare professionals are advised to consider this when prescribing Saxenda to patients with pre-existing gastrointestinal conditions.
Implications for Patients Taking Saxenda
Understanding how Saxenda affects gastric emptying helps patients set realistic expectations and optimise their treatment experience. The delayed stomach emptying contributes directly to weight loss by promoting earlier satiety during meals and reducing between-meal hunger, but it also has practical implications for daily life.
Patients often notice that they feel fuller more quickly when eating and may struggle to finish portion sizes they previously consumed comfortably. This is a desired therapeutic effect, but it requires adjustment. Eating smaller, more frequent meals rather than large portions can help manage this change. Some patients report feeling uncomfortably full or bloated if they eat too quickly or consume large volumes, as the stomach empties more slowly than before treatment.
Saxenda can be injected at any time of day, but consistent timing is recommended to establish a routine. Individual responses vary, and patients should follow their healthcare provider's guidance regarding administration.
Some medications may be affected by delayed gastric emptying. According to the SmPC, Saxenda has minimal effect on the overall absorption of oral medications including paracetamol, though the rate of absorption may be delayed. However, caution is advised with medicines that have a narrow therapeutic index, such as warfarin, where monitoring of INR (International Normalised Ratio) is recommended when starting liraglutide treatment.
For patients with severe gastrointestinal disease including gastroparesis, Saxenda is not recommended as stated in the SmPC. Patients with other gastrointestinal conditions should discuss their full medical history with their healthcare provider before starting treatment to ensure Saxenda is suitable for their circumstances. Saxenda is not recommended during pregnancy or breastfeeding.
Managing Gastrointestinal Side Effects
Gastrointestinal side effects are the most common reason for Saxenda discontinuation, but many can be effectively managed with appropriate strategies. Understanding that these symptoms often relate to delayed gastric emptying helps guide practical interventions.
Dietary modifications form the cornerstone of symptom management:
-
Eat smaller, more frequent meals rather than three large meals daily
-
Chew food thoroughly and eat slowly to reduce the volume entering an already slow-emptying stomach
-
Avoid high-fat foods, which naturally delay gastric emptying further and may exacerbate bloating
-
Gradually increase fibre intake if constipation occurs, while ensuring adequate hydration
-
Stay well hydrated, aiming for 6-8 glasses of fluid daily (unless advised otherwise by your healthcare provider)
-
Limit carbonated beverages, which can increase bloating and discomfort
The dose escalation schedule is specifically designed to improve tolerability. Saxenda treatment begins at 0.6 mg daily, increasing by 0.6 mg weekly until reaching the maintenance dose of 3.0 mg. Patients experiencing significant gastrointestinal symptoms may benefit from slowing this escalation, remaining at a lower dose for an additional week before increasing. This approach, whilst delaying achievement of the full therapeutic dose, often improves long-term adherence.
Pharmacological interventions may occasionally be appropriate. Over-the-counter remedies such as simethicone for bloating or laxatives for constipation can provide symptomatic relief. However, patients should consult their GP or pharmacist before starting additional medications. Anti-emetics are rarely necessary but may be considered for persistent nausea under medical supervision.
Common gastrointestinal side effects include nausea, vomiting, diarrhoea and constipation. Diarrhoea can lead to dehydration, so maintaining fluid intake is particularly important if this occurs.
Most gastrointestinal side effects diminish significantly after 4–8 weeks of treatment as the body adapts. Patients should be encouraged to persist through initial discomfort if symptoms are tolerable, as premature discontinuation may prevent them from experiencing the full weight-loss benefits.
When to Seek Medical Advice
Whilst mild gastrointestinal symptoms are expected with Saxenda, certain situations require prompt medical evaluation. Patients should be educated about warning signs that indicate potentially serious complications rather than typical side effects.
Seek urgent medical attention (contact 999 or attend A&E) if experiencing:
-
Severe, persistent abdominal pain, particularly if accompanied by fever, as this may indicate pancreatitis (a rare but serious adverse effect)
-
Persistent vomiting preventing fluid intake, risking dehydration
-
Signs of dehydration including dizziness, reduced urination, or confusion
-
Severe allergic reactions such as facial swelling, difficulty breathing, or widespread rash
Contact your GP or prescriber within 24–48 hours if experiencing:
-
Nausea or vomiting lasting more than a few days despite dietary modifications
-
Inability to tolerate any food or fluids for more than 24 hours
-
Severe constipation not responding to over-the-counter laxatives after 3–4 days
-
Rapid or unexpected weight loss, which may indicate excessive caloric restriction
-
Persistent heartburn or acid reflux not controlled by antacids
-
Gallbladder problems: sudden pain in the right upper abdomen, fever, yellowing of skin or eyes (jaundice), dark urine, or pale stools
Regular follow-up is essential for all patients taking Saxenda. Treatment should be discontinued if patients have not lost at least 5% of initial body weight after 12 weeks at the maintenance dose of 3.0 mg daily. Follow-up schedules will be determined by your healthcare provider according to local pathways and services.
Patients should also inform their healthcare provider if they develop new medical conditions or start new medications whilst taking Saxenda, as these may interact with the drug's effects on gastric emptying. Women who become pregnant should stop Saxenda immediately and contact their GP, as safety in pregnancy has not been established.
Report suspected side effects through the MHRA's Yellow Card Scheme (yellowcard.mhra.gov.uk). This helps regulatory authorities monitor the safety profile of Saxenda in real-world use beyond clinical trials.
Frequently Asked Questions
How long does Saxenda's effect on gastric emptying last?
The gastric emptying delay is most pronounced during the initial weeks of Saxenda treatment and may partially attenuate over time, though appetite-suppressing effects often persist throughout continued use.
Can I take other medications whilst Saxenda slows my gastric emptying?
Saxenda has minimal effect on overall absorption of most oral medications, though the rate of absorption may be delayed. Caution is advised with narrow therapeutic index medications such as warfarin, where INR monitoring is recommended when starting treatment.
What dietary changes help manage Saxenda's gastric emptying effects?
Eating smaller, more frequent meals, chewing food thoroughly, avoiding high-fat foods, staying well hydrated, and limiting carbonated beverages can significantly reduce gastrointestinal discomfort associated with delayed gastric emptying.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript