Mounjaro®
Dual-agonist support that helps curb appetite, hunger, and cravings to drive substantial, sustained weight loss.
- ~22.5% average body weight loss
- Significant weight reduction
- Improves blood sugar levels
- Clinically proven weight loss
Many patients prescribed Saxenda (liraglutide) for weight management wonder whether this medication will be detected during routine blood tests, particularly when undergoing medical investigations or employment screening. Saxenda does not typically appear on standard blood panels such as full blood counts, liver function tests, or kidney function tests. As a glucagon-like peptide-1 (GLP-1) receptor agonist, liraglutide mimics a naturally occurring hormone and is not identified by conventional drug screening. However, whilst the medication itself remains undetected, it can influence certain blood test results, including glucose levels and pancreatic enzyme markers. Understanding how Saxenda interacts with medical testing helps patients make informed decisions about their treatment.
Summary: Saxenda (liraglutide) does not appear on standard blood tests or routine drug screening panels.
Saxenda (liraglutide) is a prescription medicine licensed in the UK for weight management in adults with obesity or those who are overweight with weight-related health conditions. Many patients wonder whether Saxenda will appear on routine blood tests, particularly when undergoing medical investigations or employment screening.
The straightforward answer is that Saxenda does not typically show up on standard blood tests. Liraglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist, which is a synthetic version of a naturally occurring hormone in your body. Standard blood panels—including full blood counts, liver function tests, kidney function tests, lipid profiles, and glucose measurements—do not specifically test for the presence of liraglutide or its metabolites.
However, whilst Saxenda itself is not detected by routine blood work, the medication can influence certain blood test results. For instance, liraglutide affects blood glucose levels and may impact markers related to metabolic function. It's also worth noting that Saxenda can cause increases in serum lipase and amylase levels, even in the absence of pancreatitis, which might appear on certain blood tests. These physiological changes reflect the medication's effects rather than direct detection of the drug itself.
It is worth noting that specialised laboratory assays can measure GLP-1 analogues if specifically requested, though such tests are rarely performed outside of research settings or specific clinical investigations. For the vast majority of patients taking Saxenda, routine medical blood tests will not identify the medication unless healthcare professionals are specifically looking for it through targeted analysis.
Saxenda contains liraglutide, which is titrated weekly to a maintenance dose of 3 mg once daily. Treatment starts at 0.6 mg daily, with the dose increased by 0.6 mg increments each week until reaching the 3 mg maintenance dose. Lower maintenance doses may be used if the full dose is not tolerated. Saxenda is administered via subcutaneous injection.
As a GLP-1 receptor agonist, liraglutide mimics the action of naturally occurring GLP-1, a hormone released by the intestines in response to food intake. This mechanism of action helps regulate appetite, food intake, and body weight through several interconnected pathways.
The primary mechanisms include:
Appetite regulation – Liraglutide acts on receptors in the brain's appetite centres, particularly the hypothalamus, reducing feelings of hunger and increasing satiety after meals
Delayed gastric emptying – The medication slows the rate at which food leaves the stomach, promoting prolonged fullness and reducing the desire to eat
Glucose regulation – Liraglutide enhances insulin secretion when blood glucose levels are elevated and suppresses inappropriate glucagon release, helping to stabilise blood sugar levels
After subcutaneous injection, liraglutide is absorbed slowly, reaching maximum concentration in the blood approximately 11 hours post-injection. The medication has a half-life of around 13 hours, which allows for once-daily dosing. Liraglutide is metabolised similarly to large proteins, broken down into smaller components by enzymatic processes.
The body eliminates liraglutide through metabolic degradation, with approximately 6% of metabolites excreted in urine and 5% in faeces. No intact liraglutide is recovered in urine or faeces. This metabolic profile means that Saxenda does not accumulate in the body in a way that would be detected by standard toxicology or drug screening tests.
It's important to note that Saxenda is not recommended during pregnancy or breastfeeding, and should be discontinued if pregnancy occurs. In the UK, Saxenda is also licensed for use in adolescents aged 12-17 years with obesity, under specialist supervision.
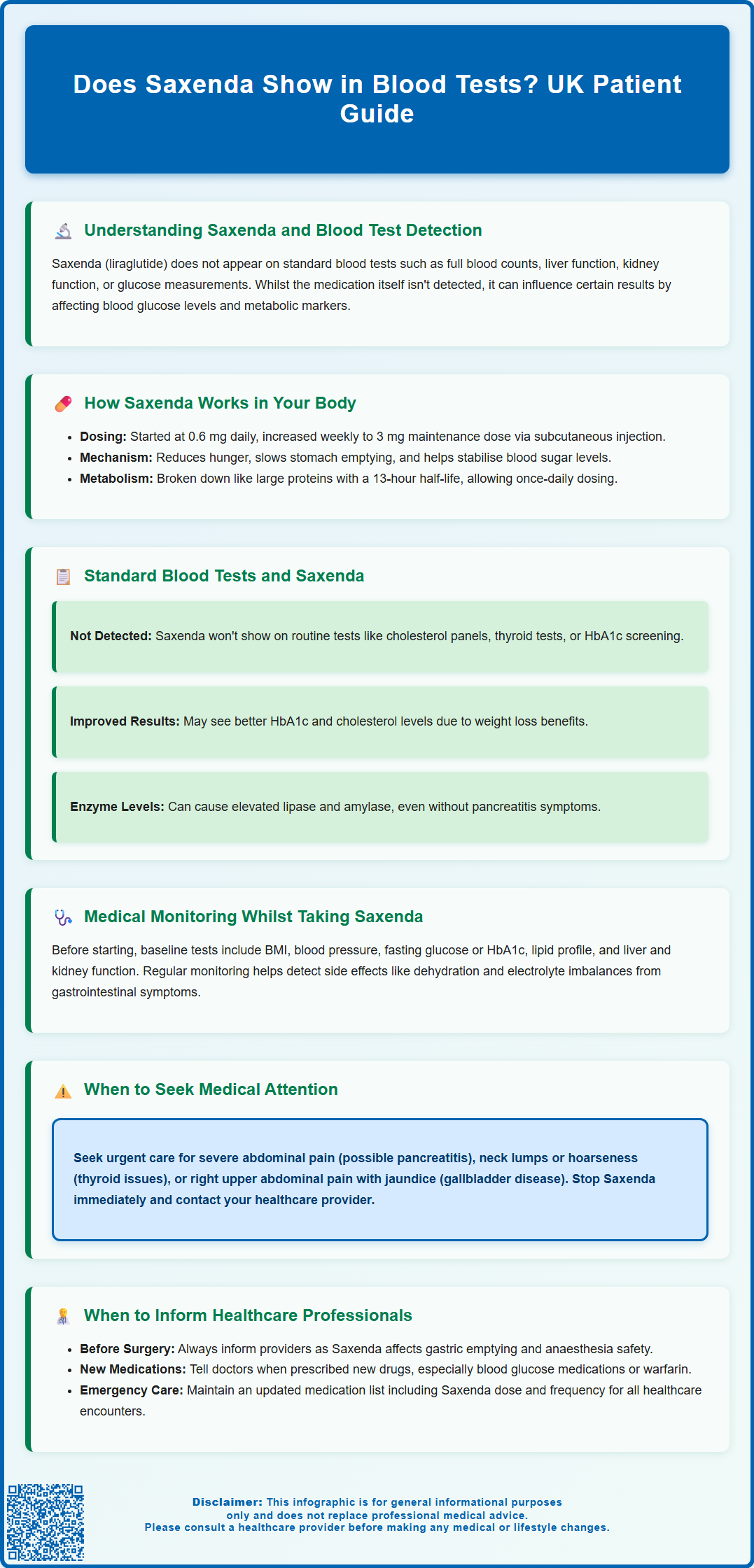
Routine blood tests ordered by GPs or hospital doctors serve various purposes, from monitoring chronic conditions to investigating symptoms or conducting pre-operative assessments. Standard blood panels do not include testing for Saxenda or liraglutide, and the medication will not appear on typical screening tests.
Common blood tests that do not detect Saxenda include:
Full blood count (FBC) – Measures red cells, white cells, and platelets
Urea and electrolytes (U&Es) – Assesses kidney function and electrolyte balance
Liver function tests (LFTs) – Evaluates liver enzymes and function
Lipid profile – Measures cholesterol and triglycerides
Thyroid function tests – Checks thyroid hormone levels
HbA1c – Measures average blood glucose over three months
Whilst Saxenda itself is not detected, the medication may influence some test results. Clinical trials have shown that patients taking Saxenda may experience improvements in metabolic markers such as reduced HbA1c levels, improved lipid profiles, and better blood pressure readings. These changes reflect the beneficial effects of weight loss and improved metabolic health rather than direct drug interference with test accuracy.
It's worth noting that Saxenda can cause increases in serum lipase and amylase levels, even without symptoms of pancreatitis. These elevations may appear on blood tests if these enzymes are measured.
Drug screening tests, whether for employment, sports, or legal purposes, do not typically include GLP-1 receptor agonists. These screens usually focus on substances of abuse, controlled medications, or performance-enhancing drugs. Saxenda is not a controlled substance under the Misuse of Drugs Act 1971. GLP-1 receptor agonists are not currently on the World Anti-Doping Agency (WADA) Prohibited List; however, athletes should check the latest list and seek advice from their sport's governing body.
If you require specialised testing that might be affected by Saxenda, your healthcare provider will advise you accordingly. In most cases, continuing your Saxenda treatment will not interfere with diagnostic blood tests or their interpretation.
Although Saxenda does not appear on standard blood tests, appropriate medical monitoring is essential for patient safety and treatment optimisation. The MHRA and NICE provide guidance on monitoring requirements for patients prescribed liraglutide for weight management.
Before starting Saxenda, your prescriber should conduct baseline assessments including:
Body mass index (BMI) and weight measurements
Blood pressure recording
Assessment of cardiovascular risk factors
Fasting glucose or HbA1c measurement
Lipid profile
Liver and kidney function tests
Thyroid function tests may be considered if clinically indicated based on your medical history.
During treatment, regular monitoring helps identify both therapeutic benefits and potential adverse effects. Common side effects that may warrant blood test monitoring include gastrointestinal symptoms (nausea, vomiting, diarrhoea), which can occasionally lead to dehydration and electrolyte disturbances. If you experience persistent vomiting or diarrhoea, your GP may request blood tests to check kidney function and electrolyte levels.
Patients should be aware of symptoms requiring urgent medical attention:
Severe abdominal pain (potentially indicating pancreatitis) – If pancreatitis is suspected, stop Saxenda immediately and seek urgent medical care
Symptoms of thyroid problems (neck lump, hoarseness, difficulty swallowing) – requires thyroid function assessment
Signs of gallbladder disease (right upper abdominal pain, jaundice) – may need liver function tests and imaging
NICE recommends reviewing treatment response at specific intervals. According to NICE Technology Appraisal 664, Saxenda should be discontinued if weight loss of at least 5% of initial body weight has not been achieved after 12 weeks on the maximum tolerated dose. Treatment is provided within specialist weight management services and is time-limited according to NICE guidance.
If you are of childbearing potential, pregnancy testing and advice on contraception may be appropriate before starting treatment. Saxenda is not recommended during pregnancy or breastfeeding.
If you experience any suspected side effects while taking Saxenda, report them to your healthcare professional or directly to the MHRA Yellow Card Scheme.
Transparency about Saxenda use is crucial for safe medical care. You should always inform healthcare professionals that you are taking Saxenda in several important situations, even though the medication does not appear on standard blood tests.
Essential disclosure situations include:
Before any surgical procedure – Saxenda affects gastric emptying, which has implications for anaesthesia. Your anaesthetist needs to know about all medications, including Saxenda, to plan safe anaesthetic management. Management (whether to continue or temporarily withhold) will be individualised based on UK perioperative guidance
When prescribed new medications – Saxenda may interact with certain drugs, particularly those affecting blood glucose levels. The delayed gastric emptying caused by Saxenda may affect the absorption of some oral medicines. If you take warfarin, more frequent INR monitoring may be needed when starting or adjusting Saxenda
During emergency medical care – Paramedics, emergency department staff, and acute care teams should be informed of all current medications
When undergoing diagnostic procedures – Some investigations requiring fasting or bowel preparation may need adjustment of your Saxenda dosing schedule
At diabetes clinic appointments – If you have type 2 diabetes, your diabetes team must know about Saxenda to adjust other glucose-lowering medications appropriately
Maintaining an up-to-date medication list is good practice for all patients. Include Saxenda on any medication lists you provide to healthcare professionals, pharmacists, or during hospital admissions. The NHS recommends keeping a written record of all prescribed medications, including the dose and frequency.
If you experience any concerning symptoms whilst taking Saxenda, contact your GP promptly. If you develop severe, persistent abdominal pain (which could indicate pancreatitis), stop taking Saxenda immediately and seek urgent medical attention. For other side effects, do not discontinue the medication without medical advice, as sudden cessation may affect your weight management progress. Your healthcare team can provide guidance on whether blood tests or other investigations are necessary based on your individual circumstances and symptoms.
No, Saxenda will not appear on pre-employment drug screening tests. These tests typically focus on substances of abuse and controlled medications, and Saxenda is not a controlled substance under UK law.
Whilst Saxenda itself is not detected, it may influence certain blood test results including glucose levels, HbA1c, lipid profiles, and pancreatic enzymes such as lipase and amylase. These changes reflect the medication's therapeutic effects rather than direct drug interference.
Yes, you should always inform healthcare professionals that you are taking Saxenda, particularly before surgery, when prescribed new medications, or during emergency care. This ensures safe medical management even though the medication does not appear on standard blood tests.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
Unordered list
Bold text
Emphasis
Superscript
Subscript