Does Saxenda make you constipated? Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults and adolescents with obesity. Constipation is a recognised side effect, occurring in approximately 1 in 100 to 1 in 10 people. This happens because Saxenda slows gastric emptying and reduces gut motility to promote satiety, which can lead to harder stools and reduced bowel frequency. Whilst less common than nausea or diarrhoea, constipation can be uncomfortable but is generally manageable with lifestyle modifications. Understanding the causes and management strategies can help you continue treatment safely and effectively.
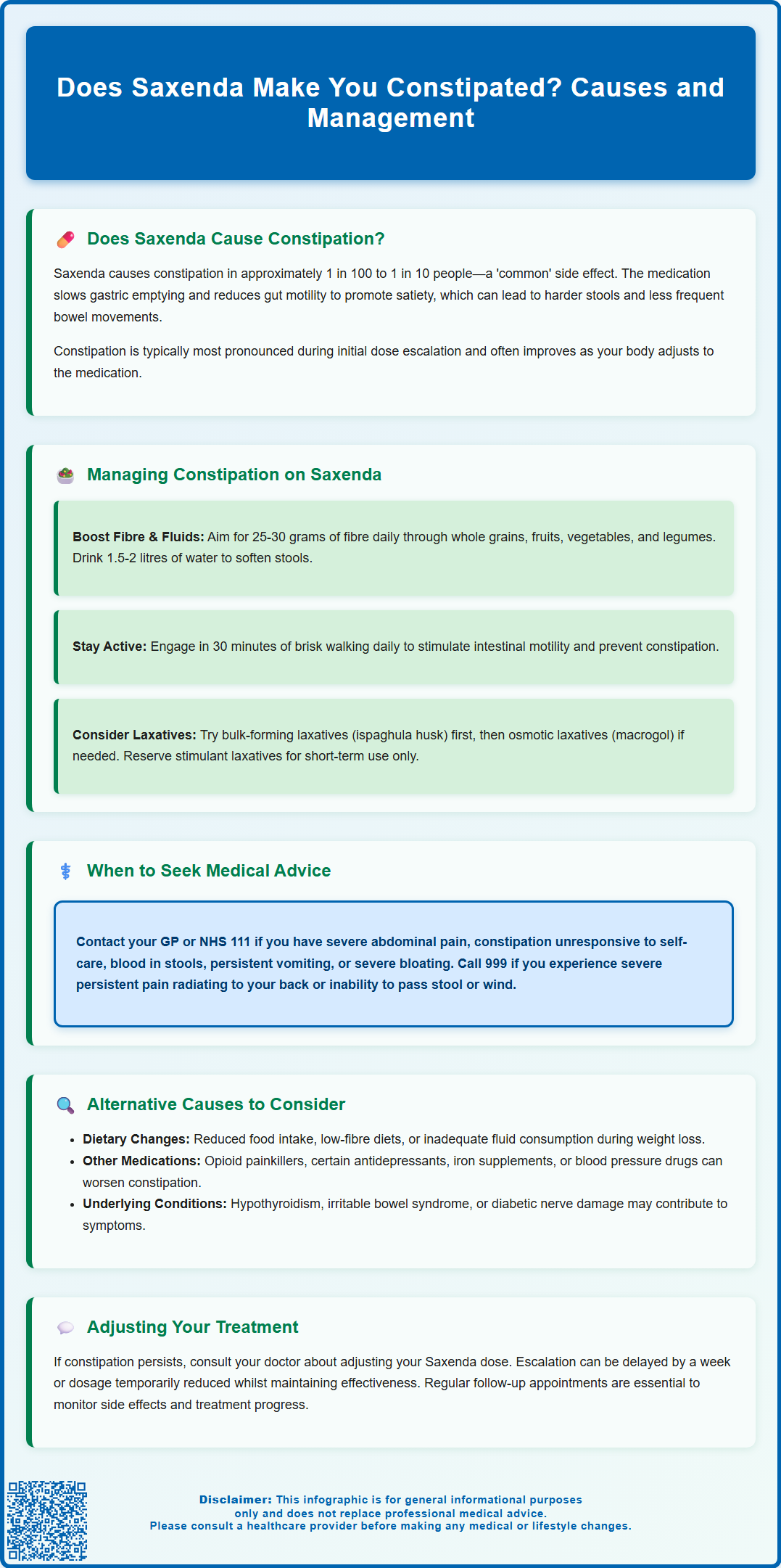
Summary: Saxenda can cause constipation in approximately 1 in 100 to 1 in 10 people, as it slows gastric emptying and reduces gut motility.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults and adolescents with obesity.
- Constipation is classified as a 'common' adverse effect, typically most pronounced during initial dose escalation.
- The mechanism involves delayed gastrointestinal transit, which promotes satiety but can lead to harder stools and reduced bowel frequency.
- Management includes increasing fibre intake to 25–30 grams daily, adequate hydration, regular physical activity, and over-the-counter laxatives if needed.
- Seek medical advice for severe abdominal pain, blood in stools, persistent symptoms unresponsive to self-care, or signs of bowel obstruction.
- Other factors such as dietary changes, concurrent medications, hypothyroidism, or reduced physical activity may also contribute to constipation during treatment.
Table of Contents
Does Saxenda Cause Constipation?
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities, and in adolescents aged 12-17 years with obesity. Constipation is recognised as a potential adverse effect of Saxenda, although it is less common than other gastrointestinal symptoms such as nausea, vomiting, and diarrhoea.
According to the MHRA-approved Summary of Product Characteristics (SmPC), constipation occurs in approximately 1 in 100 to 1 in 10 people taking Saxenda, placing it in the 'common' adverse effect category. The mechanism by which Saxenda may contribute to constipation relates to its action on the gastrointestinal tract. As a GLP-1 receptor agonist, liraglutide slows gastric emptying and reduces gut motility, which helps promote satiety and reduce appetite. This delayed transit through the digestive system can, in some individuals, lead to harder stools and reduced bowel frequency. This effect is often most pronounced during the initial dose escalation phase.
It is important to note that not everyone taking Saxenda will experience constipation, and the severity can vary considerably between individuals. Clinical trial data suggest that gastrointestinal side effects, including constipation, are often most pronounced during the initial dose escalation phase and may improve as the body adjusts to the medication. Patients should be reassured that constipation, whilst uncomfortable, is generally manageable with appropriate lifestyle modifications. However, persistent or severe symptoms may require delaying dose escalation, temporary dose reduction, or in some cases, discontinuation of treatment. If you are concerned about bowel changes whilst taking Saxenda, it is advisable to discuss these symptoms with your GP or prescribing clinician.
Managing Constipation While Taking Saxenda
Effective management of constipation during Saxenda treatment typically begins with simple lifestyle and dietary modifications. These conservative measures are often sufficient to alleviate symptoms without the need for medication.
Dietary strategies include:
-
Increasing fibre intake – Aim for 25–30 grams of fibre daily through wholegrain cereals, fruits, vegetables, pulses, and nuts. Introduce fibre gradually to avoid bloating.
-
Adequate hydration – Drink at least 1.5–2 litres of water daily. Proper hydration helps soften stools and facilitates bowel movements.
-
Regular meal patterns – Eating at consistent times can help regulate bowel function.
-
Prunes and prune juice – These contain sorbitol, a natural laxative that can gently stimulate bowel movements.
Physical activity plays a crucial role in maintaining healthy bowel function. Regular exercise, even moderate activities such as brisk walking for 30 minutes daily, can stimulate intestinal motility and help prevent constipation.
If dietary and lifestyle measures prove insufficient after about a week, over-the-counter laxatives may be considered. Bulk-forming laxatives (such as ispaghula husk or methylcellulose) are generally the first-line option, as they work naturally by increasing stool bulk. These must be taken with plenty of fluid (at least 200ml per dose) to avoid intestinal obstruction. Osmotic laxatives like macrogol (polyethylene glycol) preparations or lactulose may be used if bulk-forming agents are ineffective. Stimulant laxatives (such as senna or bisacodyl) are typically used for short-term initial treatment; longer-term use should only occur under medical supervision.
It is advisable to consult your GP or pharmacist before starting any laxative, particularly if you are taking other medications or have underlying health conditions. If constipation persists despite self-care measures, your healthcare provider can review your Saxenda dosing schedule. According to the SmPC, dose escalation may be delayed by at least a week if gastrointestinal symptoms are not tolerated, or a temporary dose reduction may be considered while maintaining therapeutic efficacy.
When to Seek Medical Advice About Bowel Changes
Whilst mild constipation during Saxenda treatment can often be managed with self-care measures, certain symptoms warrant prompt medical evaluation. It is important to recognise when bowel changes may indicate a more serious underlying condition or complication.
Contact your GP or NHS 111 if you experience:
-
Severe or persistent abdominal pain – Particularly if persistent or worsening, as this may indicate bowel obstruction or other complications.
-
Constipation that fails to respond to self-care measures and over-the-counter treatments.
-
Blood in your stools – This may appear as bright red blood or dark, tar-like stools (melaena) and requires assessment.
-
Unexplained weight loss beyond what is expected from Saxenda treatment, or loss of appetite.
-
Persistent nausea and vomiting – Especially if you cannot keep down fluids, as this increases the risk of dehydration.
-
Abdominal distension or bloating that is severe or accompanied by inability to pass wind.
-
Right upper abdominal pain, fever or yellowing of the skin/eyes – These may indicate gallbladder problems, which can occur with Saxenda.
Stop taking Saxenda and seek immediate medical attention (call 999 or attend A&E) if you develop:
-
Severe, persistent abdominal pain, possibly radiating to the back (may indicate pancreatitis)
-
Signs of bowel obstruction (inability to pass stool or wind, severe bloating, vomiting)
-
Symptoms of dehydration (dizziness, reduced urination, confusion)
Patients taking weight-loss medications should have regular follow-up appointments to monitor both efficacy and adverse effects. Your prescribing clinician should review your symptoms at each visit and can adjust your treatment plan accordingly. If constipation becomes persistent or significantly impacts your quality of life, your doctor may consider dose adjustment, temporary treatment interruption, or alternative weight management strategies.
If you believe you are experiencing side effects from Saxenda, you can report these through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Alternative Causes of Constipation During Weight Loss Treatment
When experiencing constipation whilst taking Saxenda, it is important to consider that the medication may not be the sole contributing factor. Weight loss treatment often involves multiple lifestyle changes and other factors that can independently affect bowel function.
Dietary changes associated with weight loss are a common cause of constipation. Many people reduce their overall food intake when trying to lose weight, which naturally results in less stool bulk. Additionally, some popular weight-loss diets (such as low-carbohydrate or ketogenic diets) may be low in fibre if not carefully planned. Inadequate fluid intake, particularly when increasing protein consumption, can also contribute to harder stools and constipation.
Other medications may interact with or compound the constipating effects of Saxenda. Common culprits include opioid painkillers (particularly strong opioids), certain antidepressants (particularly tricyclics), iron supplements, calcium channel blockers for blood pressure, and antihistamines. The BNF lists numerous medications that can cause constipation as a side effect. If you are taking multiple medications, discuss with your GP or pharmacist whether any could be contributing to your symptoms.
Underlying medical conditions should also be considered. Hypothyroidism (underactive thyroid) commonly causes constipation and can coexist with obesity. Irritable bowel syndrome (IBS), particularly the constipation-predominant subtype, may be exacerbated by dietary changes. Diabetes, which is common in people prescribed Saxenda, can affect gut motility through diabetic autonomic neuropathy.
Reduced physical activity due to joint pain or other obesity-related limitations can slow intestinal transit. Conversely, as weight loss progresses and mobility improves, bowel function often normalises.
If constipation symptoms are severe, persistent, or accompanied by concerning features (such as rectal bleeding, unexplained weight loss, or change in bowel habit in people over 50), your GP may arrange investigations such as thyroid function tests, coeliac screening, or referral for further assessment in line with NICE guidance. A comprehensive assessment considering all potential contributing factors ensures appropriate management and optimal outcomes during your weight loss journey.
Frequently Asked Questions
How common is constipation with Saxenda?
Constipation occurs in approximately 1 in 100 to 1 in 10 people taking Saxenda, making it a 'common' side effect according to the MHRA-approved Summary of Product Characteristics. It is typically most pronounced during the initial dose escalation phase and may improve as the body adjusts to the medication.
What can I do to relieve constipation whilst taking Saxenda?
Start with lifestyle modifications including increasing fibre intake to 25–30 grams daily, drinking 1.5–2 litres of water, and engaging in regular physical activity such as 30 minutes of brisk walking. If symptoms persist after a week, consider over-the-counter bulk-forming laxatives like ispaghula husk, taken with plenty of fluid.
When should I contact my GP about constipation on Saxenda?
Contact your GP if you experience severe or persistent abdominal pain, blood in your stools, constipation that fails to respond to self-care measures, unexplained weight loss, persistent vomiting, or severe bloating. Seek immediate medical attention for severe abdominal pain radiating to the back, signs of bowel obstruction, or symptoms of dehydration.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript