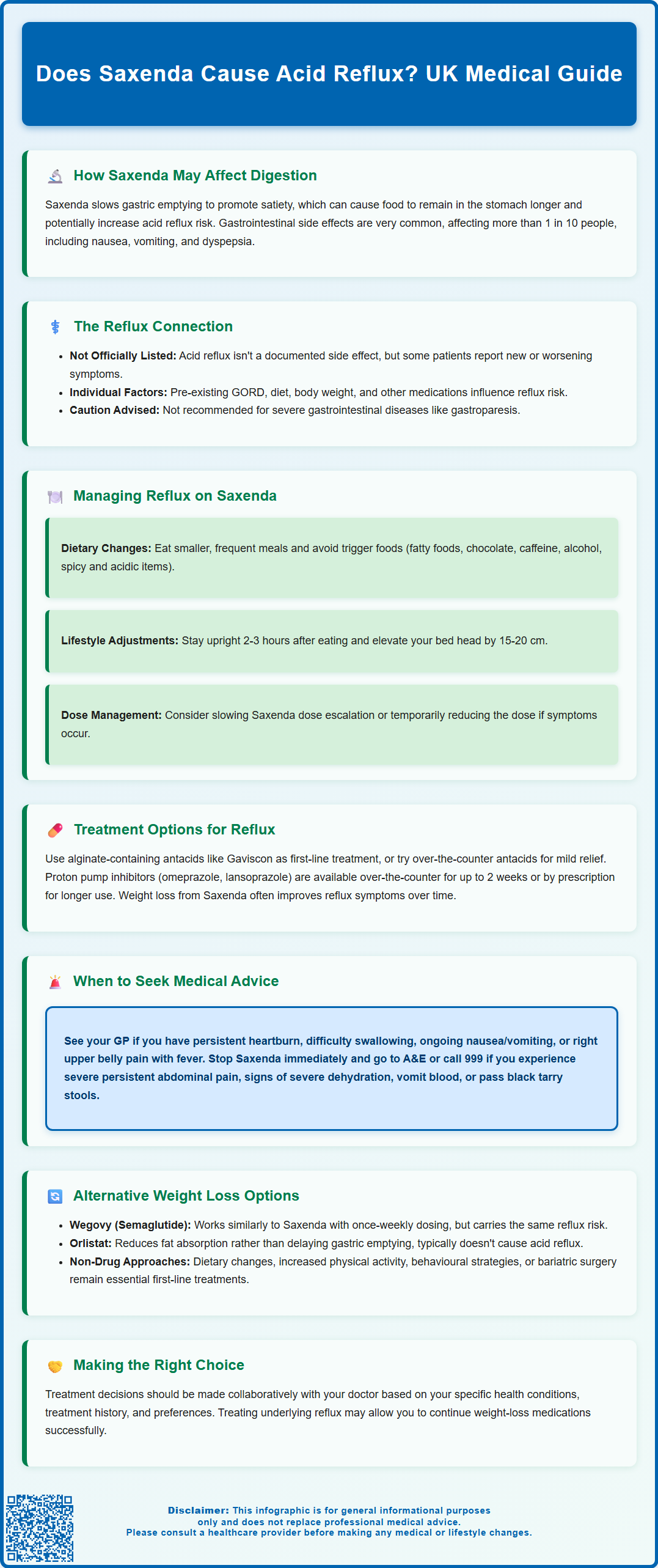
Does Saxenda cause acid reflux? Whilst acid reflux is not explicitly listed as a side effect in the Summary of Product Characteristics, gastrointestinal symptoms are amongst the most common adverse effects reported with Saxenda (liraglutide 3.0 mg). This GLP-1 receptor agonist, licensed in the UK for weight management, works partly by slowing gastric emptying—a mechanism that may increase the likelihood of reflux symptoms in some individuals. Understanding the relationship between Saxenda and digestive symptoms, alongside practical management strategies, is essential for patients considering or currently using this medication.
Summary: Saxenda may contribute to acid reflux symptoms through its mechanism of slowing gastric emptying, though reflux is not specifically listed as an adverse effect in UK prescribing information.
- Saxenda (liraglutide) is a GLP-1 receptor agonist that delays gastric emptying to promote satiety and reduce appetite.
- Gastrointestinal side effects including nausea, vomiting, and dyspepsia are very common, affecting more than 1 in 10 patients.
- Delayed gastric emptying may increase intra-gastric pressure and the likelihood of gastro-oesophageal reflux in susceptible individuals.
- Lifestyle modifications, dietary adjustments, and medications such as alginates or proton pump inhibitors can help manage reflux symptoms.
- Seek urgent medical attention for severe abdominal pain, persistent vomiting, difficulty swallowing, or signs of gastrointestinal bleeding.
- Alternative weight management medications like orlistat have different mechanisms and may be considered if reflux symptoms prove intolerable.
Table of Contents
Does Saxenda Cause Acid Reflux?
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Whilst acid reflux is not specifically listed as an adverse effect in the Summary of Product Characteristics (SmPC), gastrointestinal symptoms are amongst the most frequently reported side effects of Saxenda treatment.
The mechanism by which Saxenda may contribute to reflux symptoms relates to its pharmacological action. Liraglutide slows gastric emptying, which is one of the ways it promotes satiety and reduces appetite. This delayed emptying means food remains in the stomach for longer periods, potentially increasing intra-gastric pressure and the likelihood of gastro-oesophageal reflux. This gastric emptying delay is most pronounced early in treatment and may diminish with continued use.
Clinical trial data and post-marketing surveillance indicate that nausea, vomiting, diarrhoea, and constipation are very common (affecting more than 1 in 10 people), while dyspepsia is common (affecting up to 1 in 10 people). It's important to note that dyspepsia (indigestion) and gastro-oesophageal reflux disease (GORD) are distinct conditions, though they may overlap. Patient reports and clinical experience suggest that some individuals do experience new-onset or worsening reflux symptoms when initiating Saxenda.
It is important to note that there is no definitive causal link established between Saxenda and acid reflux in all patients. Individual susceptibility varies considerably, and pre-existing GORD, dietary factors, body weight, and concurrent medications all influence reflux risk. The SmPC advises that Saxenda is not recommended for patients with severe gastrointestinal disease (such as gastroparesis). Patients with a history of any gastrointestinal disorders should discuss these concerns with their prescriber before starting treatment.
Managing Acid Reflux While Taking Saxenda
If you experience acid reflux whilst taking Saxenda, several practical strategies may help manage symptoms without necessarily discontinuing treatment. NICE guidance emphasises the importance of lifestyle modifications alongside pharmacological interventions for both weight management and reflux control.
Dietary adjustments can significantly reduce reflux symptoms:
-
Eat smaller, more frequent meals rather than large portions, as this reduces gastric distension and pressure
-
Avoid known trigger foods such as fatty or fried foods, chocolate, caffeine, alcohol, spicy foods, and acidic items like citrus fruits and tomatoes
-
Remain upright for at least 2–3 hours after eating and avoid lying down immediately post-meal
-
Elevate the head of your bed by 15–20 cm using blocks or a wedge pillow to reduce nocturnal reflux
-
Avoid eating within 3 hours of bedtime to allow adequate gastric emptying before sleep
Medication timing and dosing considerations are important. Saxenda is typically administered once daily at any time, independent of meals. If gastrointestinal side effects occur, consider slowing the dose escalation schedule or temporarily stepping down to a lower dose, as rapid increases may exacerbate side effects.
For symptom relief, NICE recommends:
-
Alginate-containing antacids (such as Gaviscon) as first-line, as-needed treatment for reflux symptoms
-
Over-the-counter antacids containing magnesium or aluminium salts for short-term relief of mild, occasional symptoms
-
Proton pump inhibitors (PPIs) such as omeprazole or lansoprazole, available over the counter for short-term use (up to 2 weeks) or prescribed by your GP for longer courses if clinically indicated
-
H2-receptor antagonists like famotidine may be prescribed if PPIs are unsuitable (note that ranitidine remains unavailable in the UK)
If symptoms persist, your GP may consider testing for Helicobacter pylori infection, which can contribute to upper gastrointestinal symptoms.
Weight loss itself often improves reflux symptoms over time, so persisting with Saxenda under medical supervision may ultimately benefit both conditions. However, if you experience persistent vomiting or diarrhoea, seek medical advice promptly as there is a risk of dehydration and potential kidney problems.
When to Seek Medical Advice About Digestive Symptoms
Whilst mild gastrointestinal symptoms are common when starting Saxenda, certain features warrant prompt medical assessment. Understanding when symptoms require professional evaluation is essential for patient safety and appropriate management.
Contact your GP or prescribing clinician if you experience:
-
Persistent or severe heartburn that does not respond to lifestyle measures or over-the-counter treatments within 2 weeks
-
Difficulty swallowing (dysphagia) or pain when swallowing, which may indicate oesophageal inflammation or other issues
-
Unintentional weight loss beyond that expected from Saxenda treatment, or loss of appetite unrelated to the medication's intended effect
-
Persistent nausea or vomiting lasting more than a few days, particularly if preventing adequate fluid or food intake
-
Vomiting blood or passing black, tarry stools, which may indicate gastrointestinal bleeding
-
Right upper abdominal pain, fever or yellowing of the skin/eyes, which could indicate gallbladder disease (cholelithiasis or cholecystitis) – a known risk with GLP-1 medications and weight loss
Stop taking Saxenda and seek urgent medical attention (A&E or call 999) if you develop:
-
Severe, persistent abdominal pain with or without vomiting, which could suggest pancreatitis—a rare but serious adverse effect of GLP-1 agonists
-
Signs of severe dehydration including reduced urine output, dizziness, confusion, or rapid heartbeat
-
Chest pain (always requires urgent assessment regardless of cause)
NICE guidance recommends urgent specialist referral (typically within 2 weeks) for patients with alarm features such as dysphagia, unexplained weight loss (especially in those aged 55 and over with additional upper GI symptoms), persistent vomiting, gastrointestinal bleeding, or iron-deficiency anaemia. Your GP will assess whether your symptoms warrant investigation or whether they can be managed whilst continuing Saxenda treatment.
If you believe you have experienced a side effect from Saxenda, you can report this through the MHRA Yellow Card scheme (website or app), which helps monitor medication safety.
Alternative Weight Loss Medications and Acid Reflux Risk
If acid reflux symptoms prove intolerable with Saxenda, or if you have pre-existing severe GORD, alternative weight management medications may be considered. Each option has a distinct mechanism of action and side effect profile, including varying impacts on gastrointestinal symptoms.
Wegovy (semaglutide 2.4 mg) is another GLP-1 receptor agonist licensed for weight management in the UK. As it shares the same mechanism as Saxenda—including delayed gastric emptying—it carries a similar risk profile for gastrointestinal side effects. Patients who experience reflux with Saxenda may also experience it with Wegovy, though individual responses vary. Semaglutide is administered once weekly rather than daily, which some patients find more convenient, but this does not necessarily reduce reflux risk.
Orlistat (Xenical, Alli) works by inhibiting pancreatic lipase, thereby reducing dietary fat absorption by approximately 30%. Its side effect profile is distinctly different from GLP-1 agonists, predominantly featuring gastrointestinal effects related to malabsorbed fat (steatorrhoea, oily stools, faecal urgency). Orlistat does not delay gastric emptying and is not typically associated with increased acid reflux. For patients with problematic reflux on Saxenda, orlistat may represent a suitable alternative, though its efficacy is generally more modest (average weight loss 3–5% of body weight).
Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist currently licensed in the UK for type 2 diabetes management. While it is being evaluated for weight management, it is not yet licensed for this indication in the UK. Like other incretin-based therapies, it delays gastric emptying and carries similar gastrointestinal side effect risks to GLP-1 agonists.
Non-pharmacological approaches remain fundamental to weight management and should not be overlooked. NICE recommends multicomponent interventions including dietary modification, increased physical activity, and behavioural strategies as first-line treatment for obesity. Referral to specialist weight management services, consideration of very-low-calorie diets under supervision, or evaluation for bariatric surgery may be appropriate for some patients.
The decision regarding alternative treatments should be made collaboratively with your GP or specialist, considering your individual circumstances, comorbidities, previous treatment responses, and personal preferences. If reflux symptoms are severe or persistent, addressing the underlying GORD with appropriate investigation and treatment may allow successful continuation of weight management medication.
Frequently Asked Questions
Can I take antacids whilst using Saxenda for reflux symptoms?
Yes, alginate-containing antacids such as Gaviscon are recommended as first-line treatment for reflux symptoms. Over-the-counter proton pump inhibitors may be used for short-term relief, or your GP can prescribe longer courses if clinically indicated.
Will acid reflux from Saxenda improve over time?
Gastrointestinal side effects, including reflux symptoms, are often most pronounced early in treatment and may diminish with continued use. Additionally, weight loss itself frequently improves reflux symptoms over time.
Should I stop Saxenda if I develop acid reflux?
Mild reflux symptoms can often be managed with lifestyle modifications and over-the-counter treatments without discontinuing Saxenda. However, if symptoms are severe, persistent, or accompanied by alarm features such as difficulty swallowing or gastrointestinal bleeding, contact your GP for assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript