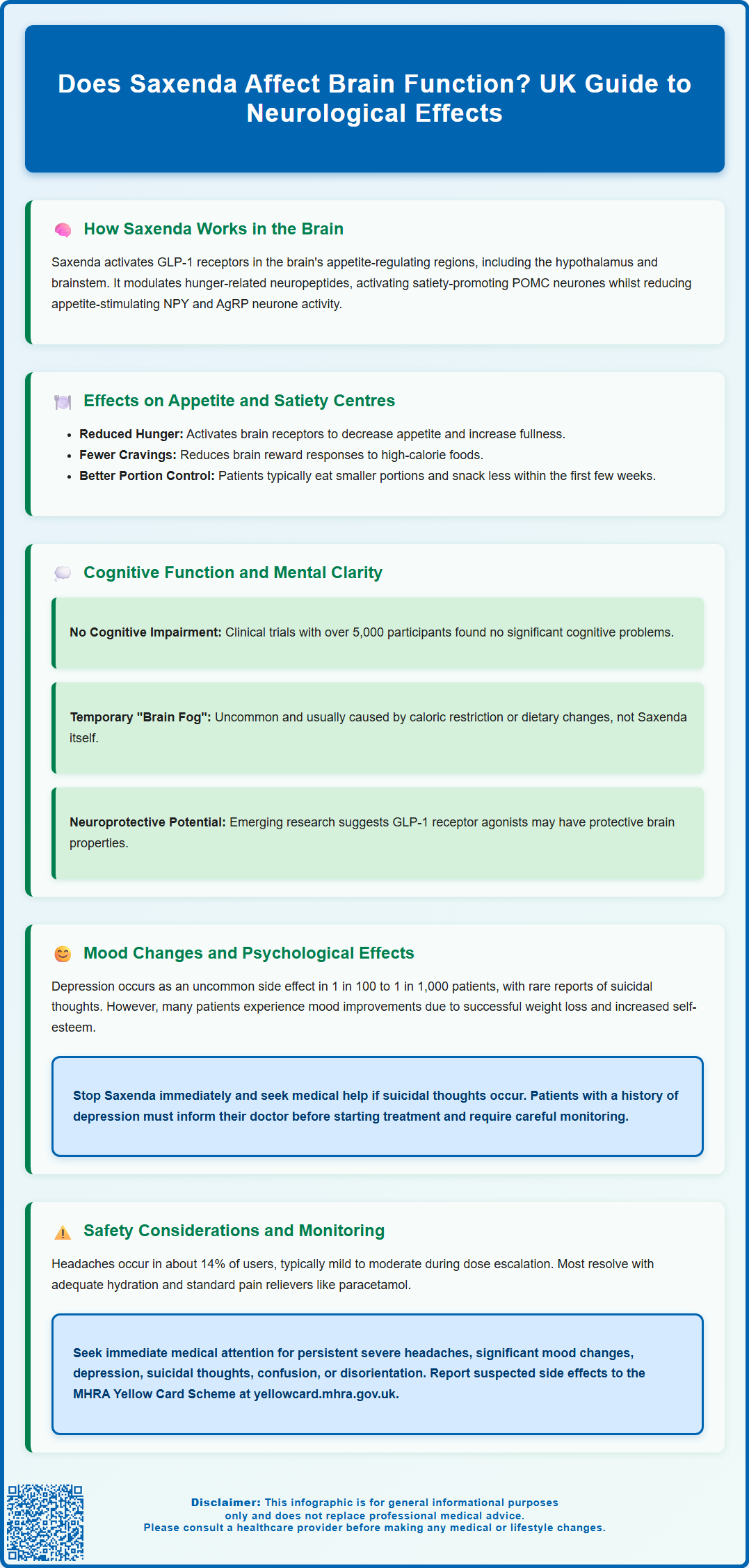
Does Saxenda affect brain function? Saxenda (liraglutide 3.0 mg), a GLP-1 receptor agonist licensed in the UK for weight management, does influence specific brain regions involved in appetite regulation and satiety. Whilst primarily a metabolic medication, Saxenda acts on GLP-1 receptors in the hypothalamus, brainstem, and reward pathways, helping to reduce hunger and promote fullness. These neurological effects are therapeutic rather than harmful, though patients may occasionally experience headaches or mood changes. Understanding how Saxenda interacts with the central nervous system helps patients and clinicians optimise treatment whilst monitoring for any concerning symptoms.
Summary: Saxenda affects specific brain regions involved in appetite regulation by activating GLP-1 receptors in the hypothalamus and brainstem, reducing hunger and promoting satiety as part of its therapeutic mechanism.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities.
- The medication acts on GLP-1 receptors in appetite-regulating brain regions including the hypothalamus, brainstem, and reward pathways to reduce hunger and increase fullness.
- Cognitive impairment is not a recognised adverse effect in clinical trials, though headaches occur in approximately 14% of patients, typically during dose escalation.
- Depression is reported as an uncommon adverse reaction; the MHRA advises careful monitoring of patients with a history of depression or suicidal thoughts.
- Treatment requires gradual dose titration over five weeks, regular monitoring, and discontinuation if less than 5% weight loss occurs after 12 weeks on the 3.0 mg maintenance dose.
Table of Contents
How Saxenda Works in the Brain
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities, and in certain adolescents aged 12-17 years. Whilst primarily recognised for its metabolic effects, research suggests Saxenda may influence the central nervous system, particularly in regions governing appetite regulation and energy homeostasis.
GLP-1 receptors are distributed throughout the brain, with concentrations in the hypothalamus, brainstem, and areas involved in reward processing. When liraglutide is administered subcutaneously, evidence suggests it may act on GLP-1 receptors on vagal afferent nerves and in circumventricular organs—brain regions where the blood-brain barrier is naturally more permeable. These actions appear to trigger neuronal pathways that communicate satiety signals to higher brain centres.
The hypothalamus, often described as the body's metabolic control centre, appears to respond to Saxenda by modulating neuropeptides involved in hunger and fullness. Research indicates the medication may influence pro-opiomelanocortin (POMC) neurons that promote satiety whilst potentially reducing the activity of neuropeptide Y (NPY) and agouti-related peptide (AgRP) neurons that stimulate appetite. This dual mechanism helps explain why patients taking Saxenda often report reduced hunger and earlier feelings of fullness after meals.
Key neurological mechanisms may include:
-
Activation of GLP-1 receptors in appetite-regulating brain regions
-
Modulation of hypothalamic neuropeptide signalling
-
Influence on reward pathways associated with food intake
-
Enhancement of satiety signals from the gastrointestinal tract to the brain
Understanding these potential central nervous system effects helps explain both the therapeutic benefits and neurological considerations associated with Saxenda treatment.
Effects of Saxenda on Appetite and Satiety Centres
The primary therapeutic benefit of Saxenda relates to its effects on appetite and satiety. Clinical trials such as the SCALE Obesity and Prediabetes study have demonstrated that liraglutide 3.0 mg reduces subjective feelings of hunger and increases post-meal fullness, effects that appear to be mediated through specific neuroanatomical pathways.
The arcuate nucleus of the hypothalamus serves as a critical integration point for metabolic signals. Research suggests Saxenda's activation of GLP-1 receptors in this region may shift the balance of neuronal activity towards satiety-promoting pathways. Some small functional neuroimaging studies have indicated that GLP-1 receptor agonists might alter brain responses to food cues, potentially reducing activation in reward-related areas when patients view images of high-calorie foods. This suggests that Saxenda may help diminish the hedonic drive to eat—the pleasure-seeking aspect of food consumption that often undermines weight management efforts.
The brainstem, particularly the area postrema and nucleus tractus solitarius, may also play a role in Saxenda's appetite-suppressing effects. These regions receive signals from the gastrointestinal tract via the vagus nerve and possess GLP-1 receptors. When activated, these brainstem centres may relay satiety information to higher cortical areas, creating an integrated sense of fullness.
Clinical implications for patients may include:
-
Reduced portion sizes at meals due to earlier satiety
-
Decreased frequency of snacking between meals
-
Diminished cravings for high-calorie, palatable foods
-
Improved ability to adhere to reduced-calorie dietary plans
These effects typically develop within the first few weeks of treatment. The 3.0 mg is the licensed maintenance dose, though individual tolerability varies. According to UK guidance, treatment should be discontinued if at least 5% of initial body weight has not been lost after 12 weeks on the 3.0 mg daily dose. Patients should be advised that appetite effects represent expected pharmacological actions rather than concerning neurological changes.
Cognitive Function and Mental Clarity During Saxenda Treatment
A common concern amongst patients considering or taking Saxenda relates to potential effects on cognitive function, memory, and mental clarity. According to the UK Summary of Product Characteristics (SmPC), cognitive impairment is not listed as a recognised adverse effect of Saxenda.
The pivotal SCALE clinical trial programme, which included over 5,000 participants treated with liraglutide 3.0 mg, did not identify cognitive impairment as a significant adverse effect. Some patients report subjective experiences of 'brain fog' or reduced mental sharpness, particularly during the initial titration phase, but these reports are relatively uncommon and may relate to concurrent factors such as caloric restriction, changes in eating patterns, or adjustment to the medication.
Emerging research into GLP-1 receptor agonists has suggested potential neuroprotective properties in preclinical studies. Some laboratory research indicates that GLP-1 receptor activation may support neuronal health and reduce neuroinflammation. Whilst these findings are preliminary and relate primarily to animal models or different clinical contexts (such as type 2 diabetes), they provide some reassurance regarding cognitive effects.
Factors that may influence mental clarity during treatment:
-
Rapid weight loss leading to temporary metabolic adjustment
-
Changes in dietary intake affecting blood glucose levels
-
Changes in sleep patterns associated with weight loss
-
Concurrent medications or underlying health conditions
It's worth noting that Saxenda alone rarely causes hypoglycaemia in people without diabetes, though the risk increases if combined with insulin or sulfonylureas in those with diabetes. Patients experiencing persistent cognitive difficulties should consult their GP to exclude other causes such as thyroid dysfunction, vitamin deficiencies (particularly B12), or mood disorders. In most cases, any initial mental fogginess resolves as the body adapts to treatment and a new dietary pattern becomes established.
Mood Changes and Psychological Effects
The relationship between Saxenda and mood represents a complex area where neurological, metabolic, and psychological factors intersect. GLP-1 receptors are present in brain regions involved in emotional regulation, including the hippocampus, amygdala, and prefrontal cortex, raising questions about potential mood-related effects.
Clinical trial data present a nuanced picture. The majority of patients do not experience significant mood changes on Saxenda. However, the UK Summary of Product Characteristics (SmPC) for Saxenda notes that depression has been reported as an uncommon adverse reaction (occurring in 1 in 100 to 1 in 1,000 patients). Additionally, suicidal ideation and behaviour have been reported rarely in post-marketing surveillance, though a direct causal relationship has not been definitively established. The MHRA advises that patients with a history of depression or suicidal thoughts should be monitored carefully during treatment.
Conversely, many patients report mood improvements during Saxenda treatment, which may relate to successful weight loss, improved metabolic health, enhanced self-esteem, and reduced weight-related stigma rather than direct neurological effects of the medication. Weight loss itself is associated with improvements in depressive symptoms in many individuals with obesity.
Important considerations regarding mood and mental health:
-
Patients with current or previous depression should inform their prescriber before starting Saxenda
-
Any emergence of suicidal thoughts or behaviour requires immediate discontinuation of treatment
-
Other significant mood changes warrant prompt medical review
-
Regular monitoring during the first few months of treatment is advisable for vulnerable individuals
Healthcare professionals should adopt a balanced approach, neither dismissing mood concerns nor creating undue alarm. The vast majority of patients tolerate Saxenda well from a psychological perspective, but individualised risk assessment and ongoing monitoring remain essential components of safe prescribing practice. Patients should be encouraged to report any mood changes promptly, and prescribers should maintain a low threshold for referral to mental health services when appropriate.
Safety Considerations and Monitoring Brain-Related Symptoms
Whilst Saxenda is generally well-tolerated, healthcare professionals and patients should remain vigilant for symptoms that may require medical attention. The UK SmPC and NICE guidance (TA664) emphasise the importance of appropriate patient selection, careful titration, and ongoing monitoring throughout treatment.
Symptoms requiring medical review include:
-
Persistent or severe headaches, particularly if different from usual headache patterns
-
Significant mood changes, depression, or suicidal thoughts
-
Confusion, disorientation, or marked changes in cognitive function
-
Any symptoms causing concern to the patient
The most commonly reported neurological adverse effect is headache, which occurs in approximately 14% of patients during clinical trials. These headaches are typically mild to moderate, occur most frequently during dose escalation, and often resolve spontaneously as treatment continues. Patients should be advised to maintain adequate hydration and may use standard analgesics such as paracetamol if needed. Persistent or worsening headaches warrant medical review to exclude other causes.
According to the UK SmPC, Saxenda is contraindicated during pregnancy and in patients with hypersensitivity to liraglutide or any of the excipients. Caution is advised in patients with a history of pancreatitis or gallbladder disease. Saxenda should not be used in combination with other GLP-1 receptor agonists and is not recommended for use with other weight-loss medications.
Monitoring recommendations for safe use:
-
Baseline assessment including mental health history and current medications
-
Gradual dose titration over five weeks to minimise adverse effects
-
Regular follow-up appointments, particularly during the first three months
-
Discontinuation if less than 5% weight loss after 12 weeks on the 3.0 mg dose
-
Patient education about symptoms requiring medical attention
Patients should be advised to contact their GP or prescribing clinician if they experience any concerning symptoms. In cases of severe symptoms or suicidal thoughts, immediate medical attention is appropriate. Patients and healthcare professionals can report suspected side effects to the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app. Overall, with appropriate patient selection, careful monitoring, and open communication between patients and healthcare providers, Saxenda can be used safely whilst minimising the risk of complications.
Frequently Asked Questions
Can Saxenda cause cognitive problems or brain fog?
Cognitive impairment is not a recognised adverse effect of Saxenda in clinical trials. Some patients report temporary mental fogginess during initial treatment, which typically relates to dietary changes or metabolic adjustment rather than direct neurological effects.
Does Saxenda affect mood or mental health?
Depression is reported as an uncommon adverse reaction (1 in 100 to 1 in 1,000 patients). The MHRA advises careful monitoring of patients with a history of depression, and any suicidal thoughts require immediate treatment discontinuation and medical attention.
Why does Saxenda reduce appetite?
Saxenda activates GLP-1 receptors in the hypothalamus and brainstem, modulating neuropeptides that control hunger and satiety. This promotes fullness after meals and reduces cravings, helping patients adhere to reduced-calorie dietary plans.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript