Does Rybelsus cause itching? Itching is not listed as a common side effect of Rybelsus (semaglutide) in UK regulatory documentation. This GLP-1 receptor agonist primarily causes gastrointestinal symptoms such as nausea and diarrhoea. However, hypersensitivity reactions can occur with any medication and may manifest as pruritus, rash, or urticaria. Serious allergic reactions including anaphylaxis have been reported in post-marketing surveillance. If you develop itching whilst taking Rybelsus, it's essential to determine whether this represents a drug reaction, an allergic response, or an unrelated condition, as many factors can cause pruritus in people with type 2 diabetes.
Summary: Itching is not a common side effect of Rybelsus, though hypersensitivity reactions causing pruritus can occur rarely.
- Rybelsus (semaglutide) is an oral GLP-1 receptor agonist licensed for type 2 diabetes treatment in the UK
- Common side effects are gastrointestinal (nausea, vomiting, diarrhoea), not dermatological
- Serious hypersensitivity reactions including anaphylaxis and angioedema have been reported in post-marketing surveillance
- Seek immediate medical attention if itching accompanies breathing difficulty, facial swelling, or widespread rash
- Multiple diabetes-related factors can cause itching including poor glycaemic control, neuropathy, and kidney disease
- Report suspected adverse reactions to the MHRA Yellow Card Scheme
Table of Contents
Does Rybelsus Cause Itching?
Itching is not listed as a common side effect of Rybelsus (semaglutide) in the official Summary of Product Characteristics (SmPC) or Patient Information Leaflet (PIL) approved by the Medicines and Healthcare products Regulatory Agency (MHRA). The most frequently reported adverse effects of this GLP-1 receptor agonist relate primarily to the gastrointestinal system, including nausea, vomiting, diarrhoea, and abdominal discomfort. These occur as the medication slows gastric emptying and affects gut motility.
However, allergic reactions and hypersensitivity responses can occur with any medication, and these may manifest as skin symptoms including itching (pruritus), rash, or urticaria. The SmPC for Rybelsus notes that serious hypersensitivity reactions including anaphylaxis and angioedema have been reported in post-marketing surveillance. If you develop signs of a hypersensitivity reaction, you should withhold further doses and seek urgent medical advice.
There is no established direct pharmacological mechanism by which Rybelsus would routinely cause itching through its action on GLP-1 receptors. The medication works by mimicking the incretin hormone GLP-1, which enhances insulin secretion in a glucose-dependent manner, suppresses glucagon release, and slows gastric emptying. None of these mechanisms typically produce pruritus as a direct consequence.
If you experience itching whilst taking Rybelsus, it is essential to consider whether this represents a true drug reaction, an allergic response, or an unrelated condition. Many factors can cause itching in people with type 2 diabetes, and correlation does not necessarily indicate causation. A thorough clinical assessment is warranted to determine the underlying cause and appropriate management strategy.
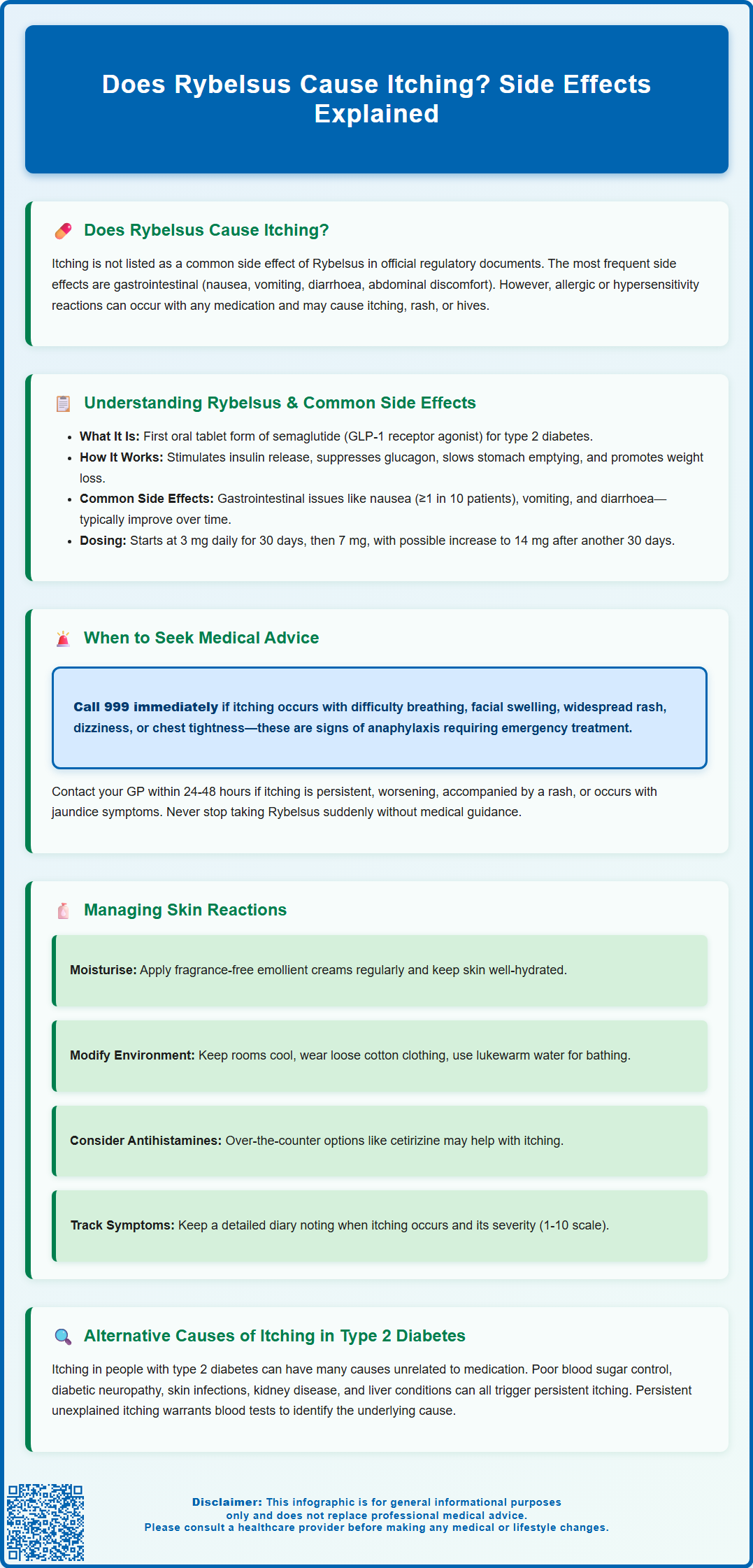
Understanding Rybelsus and Its Common Side Effects
Rybelsus is the first oral formulation of semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Unlike injectable semaglutide preparations (Ozempic, Wegovy), Rybelsus is administered as a daily tablet, offering convenience for patients who prefer oral medication. The formulation includes an absorption enhancer (SNAC) that facilitates uptake of the peptide through the gastric mucosa.
The mechanism of action involves multiple pathways that improve glycaemic control. Semaglutide binds to and activates GLP-1 receptors on pancreatic beta cells, stimulating insulin secretion only when blood glucose levels are elevated. This glucose-dependent mechanism reduces the risk of hypoglycaemia compared to some other antidiabetic agents, though the risk increases when used with insulin or sulfonylureas. The medication suppresses inappropriate glucagon secretion, slows gastric emptying, and acts on appetite centres in the brain to promote satiety and weight reduction.
The most common adverse effects are gastrointestinal in nature and include:
-
Nausea (very common, affecting ≥1/10 patients)
-
Vomiting and diarrhoea (common, affecting ≥1/100 to <1/10 patients)
-
Abdominal pain and dyspepsia
-
Constipation
-
Decreased appetite
These effects typically diminish over time as the body adapts to the medication. According to the SmPC, Rybelsus should be initiated at 3 mg once daily for 30 days, then increased to 7 mg daily; after at least another 30 days, it may be increased to 14 mg if needed. This gradual titration helps minimise gastrointestinal symptoms.
For proper absorption, Rybelsus must be taken on an empty stomach with no more than 120 ml of water, at least 30 minutes before eating, drinking, or taking other oral medicines.
Dermatological reactions are uncommon but can occur as part of hypersensitivity responses. Animal studies have shown effects on thyroid C-cells, though the clinical relevance in humans remains uncertain according to the SmPC.
When to Seek Medical Advice About Itching on Rybelsus
Immediate medical attention is required if itching is accompanied by any signs of a serious allergic reaction (anaphylaxis). These warning signs include:
-
Difficulty breathing or swallowing
-
Swelling of the face, lips, tongue, or throat (angioedema)
-
Widespread rash or hives developing rapidly
-
Dizziness, light-headedness, or feeling faint
-
Rapid heart rate or chest tightness
In such circumstances, call 999 or attend A&E immediately, as anaphylaxis constitutes a medical emergency requiring urgent treatment with adrenaline and supportive care. If you suspect an allergic reaction to Rybelsus, do not take any further doses until you have been assessed by a healthcare professional.
Contact your GP or diabetes specialist nurse within 24-48 hours if you experience:
-
Persistent or worsening itching that affects your quality of life or sleep
-
Development of a rash, blistering, or skin changes alongside itching
-
Itching accompanied by jaundice (yellowing of skin or eyes), dark urine, or pale stools, which may indicate liver dysfunction
-
Localised itching with pain, redness, or warmth, suggesting possible infection
For urgent but non-emergency concerns, you can contact NHS 111 for advice.
Routine review is appropriate for mild, intermittent itching without other concerning features. Document when the itching occurs, its severity, location, and any potential triggers or relieving factors. This information helps your healthcare provider determine whether the symptom relates to Rybelsus or another cause.
Do not stop taking Rybelsus abruptly without medical advice, as this may affect your diabetes control. Your doctor can assess whether the medication should be continued, the dose adjusted, or an alternative treatment considered. They may also arrange investigations such as liver function tests or allergy assessments if clinically indicated.
Managing Skin Reactions While Taking Rybelsus
If you develop itching whilst taking Rybelsus, several practical measures may provide relief whilst you await medical assessment. Maintain good skin hydration by applying emollient creams or ointments regularly, particularly after bathing. Choose fragrance-free, hypoallergenic products to minimise the risk of further irritation. The NHS recommends emollients as first-line management for many causes of pruritus.
Environmental modifications can reduce itching intensity:
-
Keep your home cool, as heat often exacerbates itching
-
Wear loose-fitting, cotton clothing that allows skin to breathe
-
Avoid hot baths or showers; use lukewarm water instead
-
Pat skin dry gently rather than rubbing vigorously
-
Keep fingernails short to minimise skin damage from scratching
Over-the-counter antihistamines such as cetirizine or loratadine may help if itching is related to histamine release, though evidence for their effectiveness in non-allergic pruritus is limited. Sedating antihistamines like chlorphenamine may be useful at night if itching disrupts sleep, but be aware they can cause significant drowsiness – avoid driving or operating machinery when taking them. Always discuss with your pharmacist first, particularly if you take other medications, as interactions can occur.
Avoid potential irritants including:
-
Harsh soaps, bubble baths, or shower gels
-
Biological washing detergents and fabric softeners
-
Perfumes or scented products applied directly to skin
-
Excessive alcohol consumption, which can worsen itching
Document your symptoms carefully. Keep a diary noting when itching occurs, its severity (using a scale of 1-10), and any associated factors. This information proves valuable during medical consultations.
If your doctor confirms the itching relates to Rybelsus, management will depend on the nature and severity of the reaction. For mild symptoms, they may recommend continuing treatment with supportive measures. For suspected hypersensitivity reactions (rash, urticaria, angioedema), Rybelsus should be discontinued and not restarted without specialist input. Your doctor may consider an alternative GLP-1 receptor agonist or a different class of diabetes medication, depending on your individual circumstances and glycaemic control requirements.
If you suspect an adverse reaction to Rybelsus, you or your healthcare professional can report it to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Alternative Causes of Itching in People with Type 2 Diabetes
Multiple factors unrelated to Rybelsus can cause itching in people with type 2 diabetes, and it is essential to consider these possibilities before attributing symptoms to medication. Poor glycaemic control itself frequently causes pruritus through several mechanisms. Elevated blood glucose levels lead to dehydration and dry skin (xerosis), which commonly triggers itching. High glucose also impairs skin barrier function and may promote fungal or bacterial skin infections.
Diabetic neuropathy affects many people with longstanding diabetes and can manifest as abnormal skin sensations including itching, burning, or tingling. Small nerve fibre damage disrupts normal sensory processing, sometimes producing pruritus without visible skin changes. This neuropathic itch typically affects the lower legs but can occur anywhere.
Common dermatological conditions associated with diabetes include:
-
Fungal infections (candidiasis, tinea) thriving in warm, moist areas
-
Bacterial infections including folliculitis
-
Diabetic dermopathy causing light brown, scaly patches
-
Necrobiosis lipoidica producing itchy, discoloured shin lesions
-
Generalised pruritus from dry skin
Kidney disease (diabetic nephropathy) is a common complication of diabetes and can cause uraemic pruritus, particularly in advanced stages. Liver conditions including non-alcoholic fatty liver disease (NAFLD), which frequently coexists with type 2 diabetes, can produce cholestatic itching.
Other medications used in diabetes management may cause itching, including certain blood pressure medications, statins, or other oral antidiabetic agents. Unrelated conditions such as eczema, psoriasis, urticaria, or systemic diseases (thyroid disorders, lymphoma) should also be considered.
NICE Clinical Knowledge Summaries recommend investigating persistent unexplained itching with blood tests including full blood count, renal and liver function (including alkaline phosphatase and bilirubin), thyroid function, glucose/HbA1c, ferritin, calcium, and inflammatory markers (CRP/ESR). Your GP may also examine your skin thoroughly and consider referral to dermatology if the cause remains unclear or symptoms persist despite initial management strategies.
Frequently Asked Questions
Is itching a common side effect of Rybelsus?
No, itching is not listed as a common side effect in the official UK regulatory documentation for Rybelsus. The most frequent adverse effects are gastrointestinal, including nausea, vomiting, and diarrhoea.
When should I seek medical help for itching whilst taking Rybelsus?
Seek immediate medical attention (call 999) if itching is accompanied by difficulty breathing, facial swelling, widespread rash, or dizziness, as these may indicate anaphylaxis. Contact your GP within 24-48 hours for persistent itching, rash development, or itching with jaundice.
What else could cause itching in people with type 2 diabetes?
Multiple factors can cause itching in diabetes including poor glycaemic control leading to dry skin, diabetic neuropathy, fungal or bacterial infections, kidney disease, liver conditions, and other medications. A thorough clinical assessment is needed to identify the underlying cause.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












