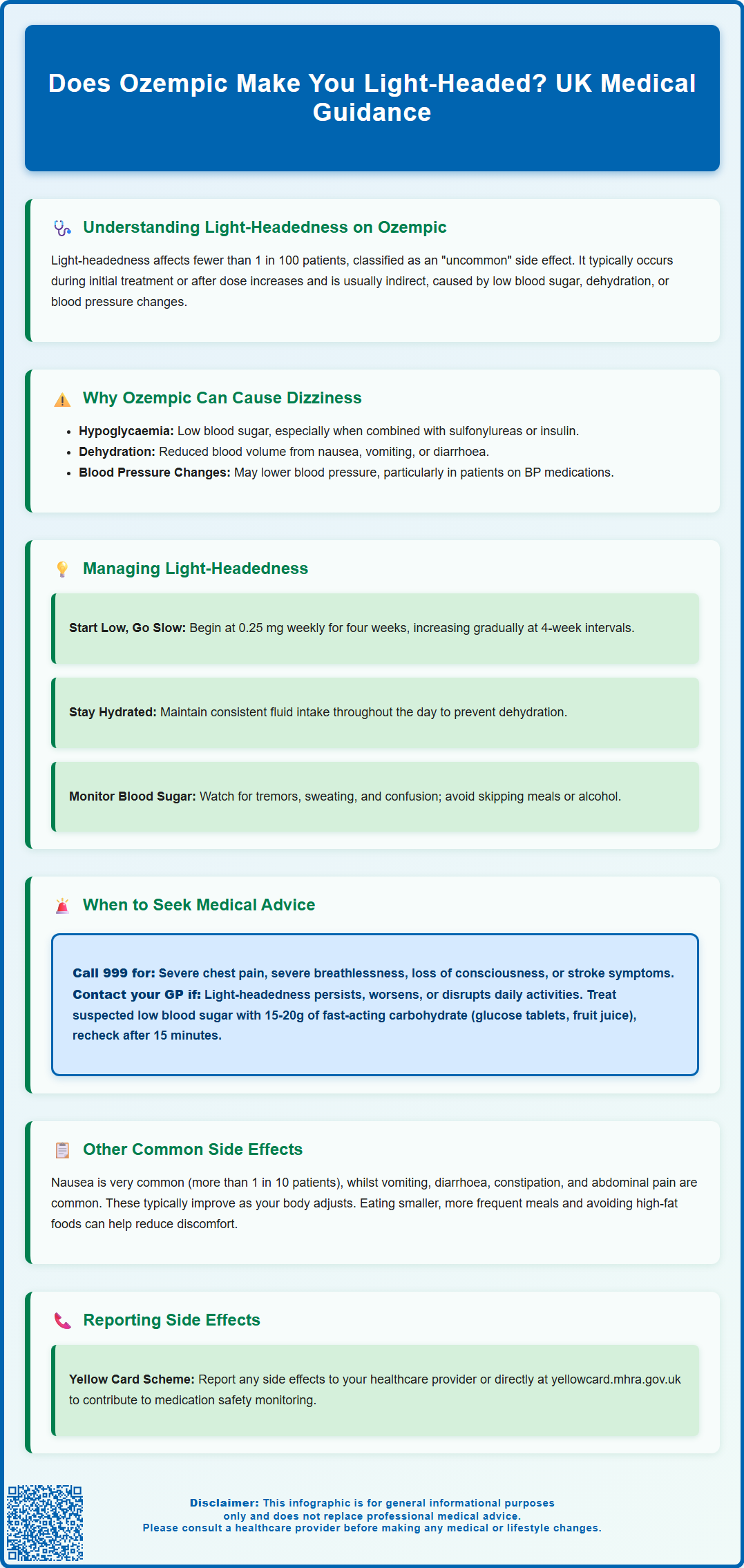
Does Ozempic make you light-headed? Yes, Ozempic (semaglutide) can cause light-headedness in some patients, though this is classified as an uncommon side effect by the MHRA. This GLP-1 receptor agonist, licensed for type 2 diabetes mellitus treatment in the UK, may trigger dizziness through several mechanisms including hypoglycaemia (particularly when combined with other diabetes medications), dehydration from gastrointestinal effects, or blood pressure changes. Whilst mild, transient light-headedness often resolves as the body adjusts to treatment, persistent or severe symptoms warrant medical review. Understanding when light-headedness requires intervention and how to manage it safely is essential for patients prescribed this medication.
Summary: Ozempic can cause light-headedness in fewer than 1 in 100 patients, typically through indirect mechanisms such as hypoglycaemia, dehydration, or blood pressure changes rather than direct pharmacological effects.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus treatment.
- Light-headedness is classified as an uncommon side effect by the MHRA, affecting fewer than 1 in 100 patients.
- Hypoglycaemia risk increases when Ozempic is combined with sulfonylureas or insulin, requiring dose adjustment of concomitant medications.
- Dehydration from gastrointestinal side effects (nausea, vomiting, diarrhoea) can cause orthostatic hypotension and dizziness.
- Seek urgent medical attention if light-headedness is accompanied by chest pain, fainting, severe hypoglycaemia, or visual disturbances.
- Regular monitoring of blood glucose and blood pressure helps identify and manage causes of light-headedness during Ozempic treatment.
Table of Contents
Does Ozempic Make You Light-Headed?
Yes, Ozempic (semaglutide) can cause light-headedness in some patients, though it is not among the most commonly reported side effects. Light-headedness, dizziness, or feeling faint may occur particularly during the initial weeks of treatment or following dose increases. According to the MHRA/EMC Summary of Product Characteristics (SmPC), dizziness is classified as an 'uncommon' side effect, affecting fewer than 1 in 100 patients.
Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by enhancing insulin secretion in response to elevated blood glucose levels, suppressing glucagon release, and slowing gastric emptying. These mechanisms improve glycaemic control but can also contribute to symptoms such as light-headedness through several pathways.
The relationship between Ozempic and light-headedness is typically indirect rather than a direct pharmacological effect. Most cases relate to the medication's impact on blood glucose levels, blood pressure, hydration status, or gastrointestinal function. Patients may experience light-headedness due to hypoglycaemia (particularly when Ozempic is combined with other glucose-lowering medications such as sulfonylureas or insulin), dehydration secondary to gastrointestinal side effects, or changes in blood pressure. When used as monotherapy, Ozempic has a low risk of causing hypoglycaemia.
It is important to distinguish between occasional mild light-headedness and persistent or severe symptoms. Transient light-headedness that resolves quickly may not require immediate intervention, whereas recurrent episodes, especially those accompanied by other symptoms, warrant medical review. Understanding the potential causes and recognising warning signs enables patients to manage their treatment safely and seek appropriate advice when necessary.
When to Seek Medical Advice About Light-Headedness on Ozempic
Patients should contact their GP or diabetes specialist nurse if light-headedness persists, worsens, or interferes with daily activities. Whilst mild, occasional dizziness may settle as the body adjusts to Ozempic, certain presentations require prompt medical assessment to exclude serious underlying causes or complications.
Seek urgent medical attention if light-headedness is accompanied by:
-
Severe or persistent hypoglycaemia – symptoms including confusion, sweating, tremor, palpitations, or difficulty concentrating
-
Chest pain or palpitations – which may indicate cardiovascular complications
-
Severe dehydration – signs include reduced urine output, dark urine, extreme thirst, or dry mucous membranes
-
Fainting or loss of consciousness – even brief episodes warrant investigation
-
Visual disturbances – blurred vision, double vision, or visual field defects
-
Severe headache – particularly if sudden onset or unlike previous headaches
-
Difficulty breathing or speaking – which may suggest a serious adverse reaction
Call 999 immediately for severe chest pain, severe breathlessness, loss of consciousness, or symptoms of stroke. For urgent concerns when unsure, contact NHS 111 for advice.
If you suspect hypoglycaemia (low blood sugar), take 15-20g of fast-acting carbohydrate (e.g., glucose tablets, fruit juice, or sugary drink), check your blood glucose after 15 minutes, and repeat treatment if levels remain low.
Routine medical review is advisable if:
-
Light-headedness occurs frequently or predictably (e.g., after each injection)
-
Symptoms develop after a dose increase and do not improve within one to two weeks
-
You experience recurrent episodes of low blood glucose readings
-
Light-headedness is associated with persistent nausea, vomiting, or diarrhoea
-
You have concerns about medication interactions or other health conditions
Your healthcare professional may need to adjust your Ozempic dose, review concomitant medications (particularly other diabetes treatments, antihypertensives, or diuretics), or investigate alternative causes. Never discontinue Ozempic without medical guidance, as abrupt cessation may lead to deterioration in glycaemic control. Do not drive or operate machinery if experiencing dizziness or symptoms of hypoglycaemia. Maintaining open communication with your diabetes care team ensures safe, effective treatment management.
Other Common Side Effects of Ozempic to Be Aware Of
Ozempic is generally well tolerated, but gastrointestinal side effects are the most frequently reported adverse reactions. Understanding the full side effect profile helps patients distinguish between expected, manageable symptoms and those requiring medical attention.
Gastrointestinal effects are particularly common, especially during treatment initiation and dose escalation:
-
Nausea – classified as 'very common' (affecting more than 1 in 10 patients) in the SmPC
-
Vomiting – 'common' (affecting up to 1 in 10 patients)
-
Diarrhoea – 'common' according to the MHRA/EMC SmPC
-
Constipation – 'common', likely related to delayed gastric emptying
-
Abdominal pain or discomfort – 'common', generally mild to moderate in severity
-
Decreased appetite – 'common', which may lead to reduced food intake and weight loss (note that while weight loss can occur with Ozempic, it is not licensed for weight management in the UK)
These gastrointestinal symptoms usually diminish over time as the body adapts to the medication. Eating smaller, more frequent meals and avoiding high-fat foods may help minimise discomfort.
Other notable side effects include:
-
Hypoglycaemia – risk increases when Ozempic is used alongside sulfonylureas or insulin; dose adjustment of concomitant medications may be necessary
-
Injection site reactions – mild redness, itching, or swelling at the injection site
-
Headache – generally mild and self-limiting
Rare but serious adverse effects that require immediate medical attention include:
-
Pancreatitis – severe, persistent abdominal pain radiating to the back, often accompanied by vomiting
-
Gallbladder problems – right upper abdominal pain, particularly after eating fatty meals
-
Diabetic retinopathy complications – worsening of existing diabetic eye disease, particularly with rapid glycaemic improvement
-
Acute kidney injury – usually secondary to severe dehydration from gastrointestinal effects
If you experience any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed above. You can also report side effects directly via the Yellow Card Scheme at yellowcard.mhra.gov.uk to help provide more information on the safety of this medicine.
Why Ozempic Can Cause Dizziness and Light-Headedness
Understanding the mechanisms behind light-headedness helps patients and clinicians identify contributing factors and implement appropriate management strategies. Ozempic's effects on multiple physiological systems can lead to dizziness through several distinct pathways.
Hypoglycaemia (low blood glucose) represents the most clinically significant cause of light-headedness in Ozempic users. Semaglutide enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release, improving glycaemic control. However, when combined with other glucose-lowering medications—particularly sulfonylureas (e.g., gliclazide) or insulin—the risk of hypoglycaemia increases substantially. Symptoms of hypoglycaemia include:
-
Light-headedness or dizziness
-
Tremor and sweating
-
Palpitations
-
Confusion or difficulty concentrating
-
Hunger
Patients experiencing recurrent hypoglycaemia require medication review and possible dose reduction of concomitant diabetes treatments. Caution is also advised when consuming alcohol, during periods of fasting or missed meals, and with unplanned vigorous exercise, as these can increase hypoglycaemia risk when taking Ozempic with sulfonylureas or insulin.
Dehydration and electrolyte disturbances commonly result from Ozempic's gastrointestinal side effects. Nausea, vomiting, and diarrhoea can lead to fluid and electrolyte losses, reducing circulating blood volume and causing orthostatic hypotension (a drop in blood pressure upon standing). This manifests as light-headedness, particularly when moving from sitting to standing positions. Maintaining adequate hydration is essential—patients should aim for regular fluid intake throughout the day, especially during periods of gastrointestinal upset.
Blood pressure changes may occur in some Ozempic users. Whilst GLP-1 receptor agonists can have modest blood pressure-lowering effects (generally beneficial for cardiovascular health), patients taking antihypertensive medications may experience excessive blood pressure reduction, leading to dizziness. Regular blood pressure monitoring helps identify this issue, allowing for adjustment of antihypertensive therapy if necessary. Checking lying and standing blood pressure may be helpful in patients with postural symptoms.
Delayed gastric emptying is a therapeutic mechanism of Ozempic that contributes to improved glycaemic control and satiety. This slowed gastrointestinal transit is part of how the medication works to improve blood glucose control.
Vasovagal responses to injections, though not specific to Ozempic, can cause transient light-headedness or fainting in needle-sensitive individuals. This is a psychological rather than pharmacological response.
NICE guidance on type 2 diabetes management (NG28) emphasises individualised treatment approaches and regular monitoring for adverse effects. Clinicians should assess for hypoglycaemia risk, review concomitant medications, and ensure patients understand how to recognise and respond to concerning symptoms. Dose titration following the recommended schedule helps minimise side effects whilst allowing physiological adaptation to the medication's effects. The Ozempic SmPC recommends starting at 0.25 mg weekly for four weeks (initiation dose only, not for glycaemic control), then increasing to 0.5 mg weekly. If needed, the dose may be increased to 1 mg weekly and then to 2 mg weekly at intervals of at least 4 weeks.
Frequently Asked Questions
Can Ozempic cause low blood sugar and dizziness?
Yes, Ozempic can cause hypoglycaemia and associated dizziness, particularly when combined with sulfonylureas or insulin. When used as monotherapy, the risk of hypoglycaemia is low, but concomitant glucose-lowering medications significantly increase this risk and may require dose adjustment.
How long does light-headedness from Ozempic typically last?
Light-headedness from Ozempic often occurs during initial weeks of treatment or following dose increases and typically improves within one to two weeks as the body adjusts. Persistent or worsening symptoms beyond this period warrant medical review to identify underlying causes.
Should I stop taking Ozempic if I feel dizzy?
Do not discontinue Ozempic without medical guidance, as abrupt cessation may lead to deterioration in glycaemic control. Contact your GP or diabetes specialist nurse if dizziness persists, worsens, or interferes with daily activities for appropriate assessment and management.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript