Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus in adults. Whilst Ozempic is not directly associated with causing ketoacidosis in the same manner as some other diabetes medications, understanding the potential metabolic risks remains important for safe prescribing and patient monitoring. Ketoacidosis is a serious condition characterised by dangerous accumulation of ketones in the blood, leading to acidification. This article examines the relationship between Ozempic and ketoacidosis risk, explores warning signs to monitor, and provides guidance on when to seek medical advice whilst taking this medication.
Summary: Ozempic is not directly linked to causing ketoacidosis, though rare cases have been reported when insulin was rapidly reduced or discontinued upon starting GLP-1 receptor agonists.
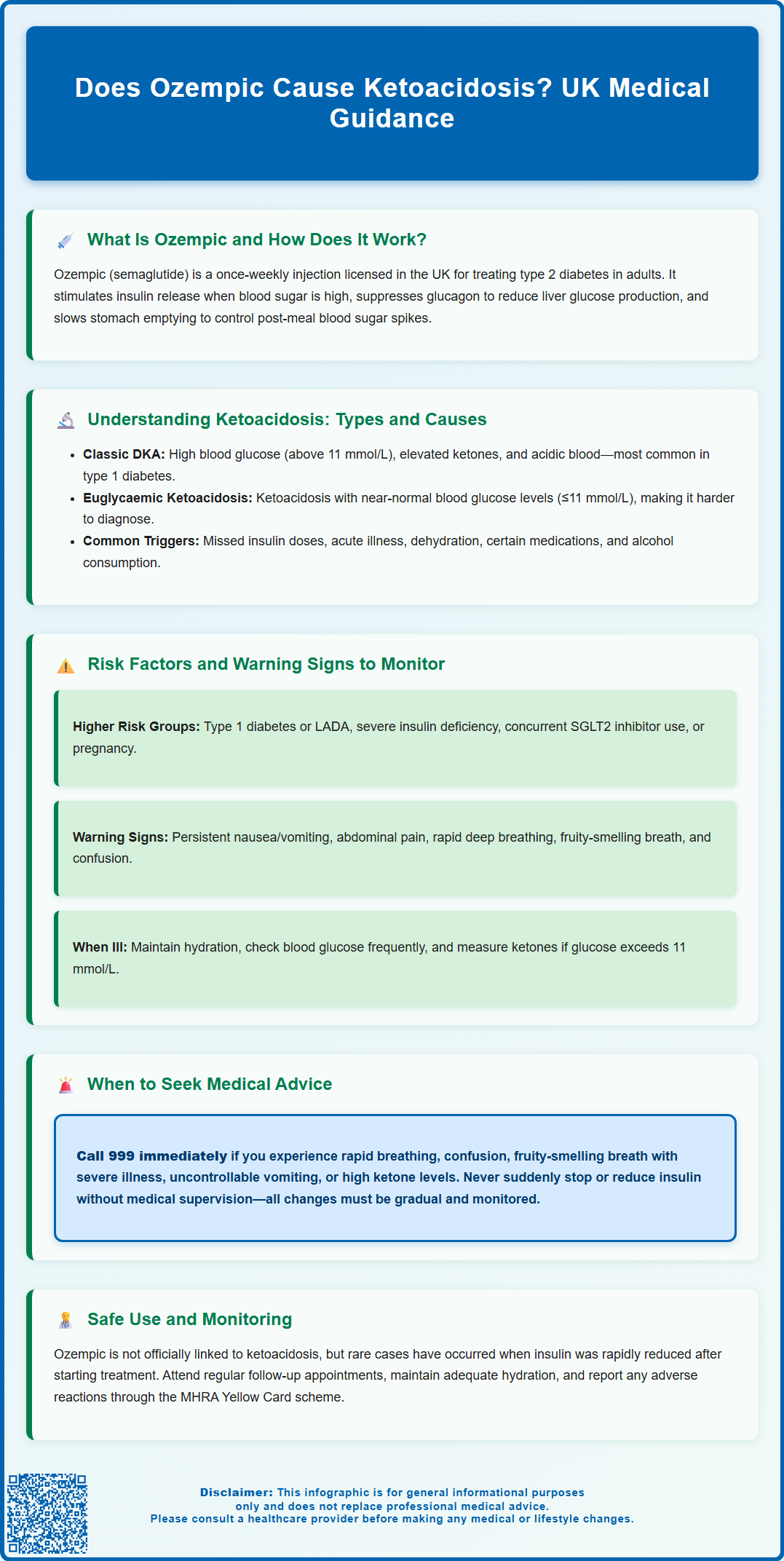
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, not type 1 diabetes or as insulin replacement.
- Ketoacidosis risk increases if insulin is abruptly reduced when starting Ozempic, particularly in insulin-dependent patients or those with severe insulin deficiency.
- Warning signs include persistent vomiting, abdominal pain, rapid breathing, fruity-smelling breath, and confusion requiring immediate medical assessment.
- Patients should follow sick-day rules during illness: maintain hydration, check blood glucose and ketones frequently, and never stop insulin without medical supervision.
- The MHRA monitors semaglutide safety, and healthcare professionals should prescribe according to licensed indications with regular patient follow-up and education.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates blood glucose levels.
The mechanism of action involves several complementary pathways. Ozempic stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it primarily promotes insulin release when blood sugar levels are elevated. This results in a low intrinsic risk of hypoglycaemia, though this risk increases when used alongside insulin or sulfonylureas (dose adjustments of these medications may be needed). Additionally, it suppresses the release of glucagon—a hormone that raises blood glucose—thereby preventing excessive glucose production by the liver.
Beyond glycaemic control, Ozempic initially slows gastric emptying, which helps reduce post-meal blood sugar spikes and promotes a feeling of fullness, though this effect diminishes over time. While weight reduction may occur, in the UK Ozempic is specifically licensed for type 2 diabetes management (Wegovy is the licensed semaglutide product for weight management). The medication is administered once weekly via subcutaneous injection, typically in the abdomen, thigh, or upper arm.
NICE guidance (NG28) supports the use of GLP-1 receptor agonists like Ozempic as part of a comprehensive treatment plan that includes diet, exercise, and other glucose-lowering therapies when glycaemic targets are not achieved with first-line treatments. The MHRA continues to monitor the safety profile of semaglutide, and healthcare professionals should prescribe it in accordance with its licensed indications and patient-specific factors.
Understanding Ketoacidosis: Types and Causes
Ketoacidosis is a serious metabolic condition characterised by the accumulation of ketone bodies in the blood, leading to acidification of the bloodstream. There are two main types relevant to diabetes management: diabetic ketoacidosis (DKA) and euglycaemic diabetic ketoacidosis.
Diabetic ketoacidosis (DKA) is most commonly associated with type 1 diabetes, though it can occur in type 2 diabetes under certain circumstances. It develops when there is insufficient insulin to allow glucose to enter cells for energy. The body then breaks down fat as an alternative fuel source, producing ketones as a by-product. When ketones accumulate rapidly, they cause the blood to become acidic. Classic DKA presents with significantly elevated blood glucose levels (typically above 11 mmol/L), alongside ketones in blood (≥3.0 mmol/L) or urine, and metabolic acidosis (pH <7.3 and/or bicarbonate <15 mmol/L).
Euglycaemic diabetic ketoacidosis is a less common variant where ketoacidosis occurs with blood glucose levels that are near-normal or only moderately elevated (≤11.0-11.1 mmol/L). This atypical presentation can make diagnosis more challenging, as clinicians may not immediately suspect ketoacidosis when glucose readings are not markedly raised.
Causes of ketoacidosis include:
-
Insulin deficiency (missed doses, pump failure, or inadequate dosing)
-
Acute illness or infection (increasing insulin requirements)
-
Dehydration
-
Certain medications that affect glucose or ketone metabolism
-
Alcohol consumption (particularly binge drinking)
-
Pregnancy (increased insulin resistance)
It's important to note that GLP-1 receptor agonists like Ozempic are not licensed for type 1 diabetes and are not a substitute for insulin therapy in insulin-dependent patients.
Risk Factors and Warning Signs to Monitor
Whilst Ozempic is not officially linked to causing ketoacidosis in the same manner as SGLT2 inhibitors (another class of diabetes medication with a recognised association), healthcare professionals and patients should remain vigilant about potential metabolic complications. The MHRA has reported rare cases of diabetic ketoacidosis when insulin was rapidly reduced or discontinued upon initiation of GLP-1 receptor agonists.
Risk factors that may increase susceptibility to ketoacidosis in people with diabetes include:
-
Type 1 diabetes or latent autoimmune diabetes in adults (LADA)
-
Severe insulin deficiency or pancreatic insufficiency
-
Acute illness, infection, or surgery (increasing metabolic stress)
-
Significant reduction in food intake or prolonged fasting
-
Excessive alcohol consumption
-
Concurrent use of SGLT2 inhibitors (which have a recognised ketoacidosis risk)
-
Pregnancy (increased insulin resistance)
Warning signs of ketoacidosis that patients should monitor include:
-
Persistent nausea and vomiting
-
Abdominal pain
-
Unusual fatigue or weakness
-
Rapid, deep breathing (Kussmaul respiration)
-
Fruity-smelling breath (acetone odour)
-
Confusion or difficulty concentrating
-
Excessive thirst and urination
Patients taking Ozempic should follow sick-day rules if unwell: maintain hydration, continue carbohydrate intake if possible, check blood glucose more frequently, and measure blood ketones if glucose is >11 mmol/L or if experiencing persistent vomiting (even with normal glucose levels). SGLT2 inhibitors should be temporarily stopped during acute illness. The gastrointestinal side effects of Ozempic (nausea, vomiting) may contribute to dehydration, which can increase ketosis risk, so adequate fluid intake is essential.
When to Seek Medical Advice While Taking Ozempic
Patients prescribed Ozempic should be provided with clear guidance on when to contact their GP, diabetes specialist nurse, or seek urgent medical attention. Immediate medical assessment is warranted if any signs of ketoacidosis develop, particularly the combination of persistent vomiting, abdominal pain, and unusual fatigue.
Contact your GP or diabetes team promptly if you experience:
-
Persistent nausea or vomiting lasting more than 24 hours, especially if unable to keep down fluids
-
Severe abdominal pain that is unexplained
-
Signs of dehydration (reduced urination, dizziness, dry mouth)
-
Unexplained weight loss beyond expected therapeutic effects
-
Difficulty managing blood glucose levels despite adherence to treatment
-
Symptoms of pancreatitis (severe upper abdominal pain radiating to the back)
Seek emergency care (call 999 or attend A&E) if you develop:
-
Rapid, deep breathing or shortness of breath
-
Confusion, drowsiness, or loss of consciousness
-
Fruity-smelling breath combined with feeling very unwell
-
Severe, unrelenting vomiting with inability to retain any fluids
-
Blood ketone levels ≥3.0 mmol/L or high urine ketones with symptoms
-
Chest pain or signs of cardiovascular compromise
Importantly, do not abruptly reduce or stop insulin when starting Ozempic, as this can precipitate ketoacidosis. Any insulin adjustments should be made gradually under medical supervision with careful monitoring. If you are severely unwell or pancreatitis is suspected, it may be appropriate to temporarily withhold Ozempic while seeking medical advice.
During periods of illness, check blood ketones if you have persistent vomiting or glucose >11 mmol/L, maintain hydration, and stop any SGLT2 inhibitors. For urgent non-emergency advice, contact NHS 111.
NICE recommendations emphasise the importance of patient education and shared decision-making when initiating GLP-1 receptor agonists. Regular follow-up appointments allow healthcare professionals to assess treatment response, monitor for adverse effects, and adjust therapy as needed. Patients should report suspected side effects via the MHRA Yellow Card scheme.
Frequently Asked Questions
Can Ozempic cause diabetic ketoacidosis in type 2 diabetes patients?
Ozempic is not directly associated with causing ketoacidosis, but rare cases have occurred when insulin was rapidly reduced or stopped upon starting the medication. Patients should never abruptly discontinue insulin without medical supervision.
What are the warning signs of ketoacidosis whilst taking Ozempic?
Warning signs include persistent nausea and vomiting, severe abdominal pain, rapid deep breathing, fruity-smelling breath, confusion, and unusual fatigue. Seek emergency care immediately if these symptoms develop.
Should I check ketone levels whilst taking Ozempic?
Check blood ketones if you have persistent vomiting or blood glucose above 11 mmol/L, particularly during illness. Maintain hydration and follow sick-day rules, contacting your diabetes team if ketones are elevated or symptoms persist.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












