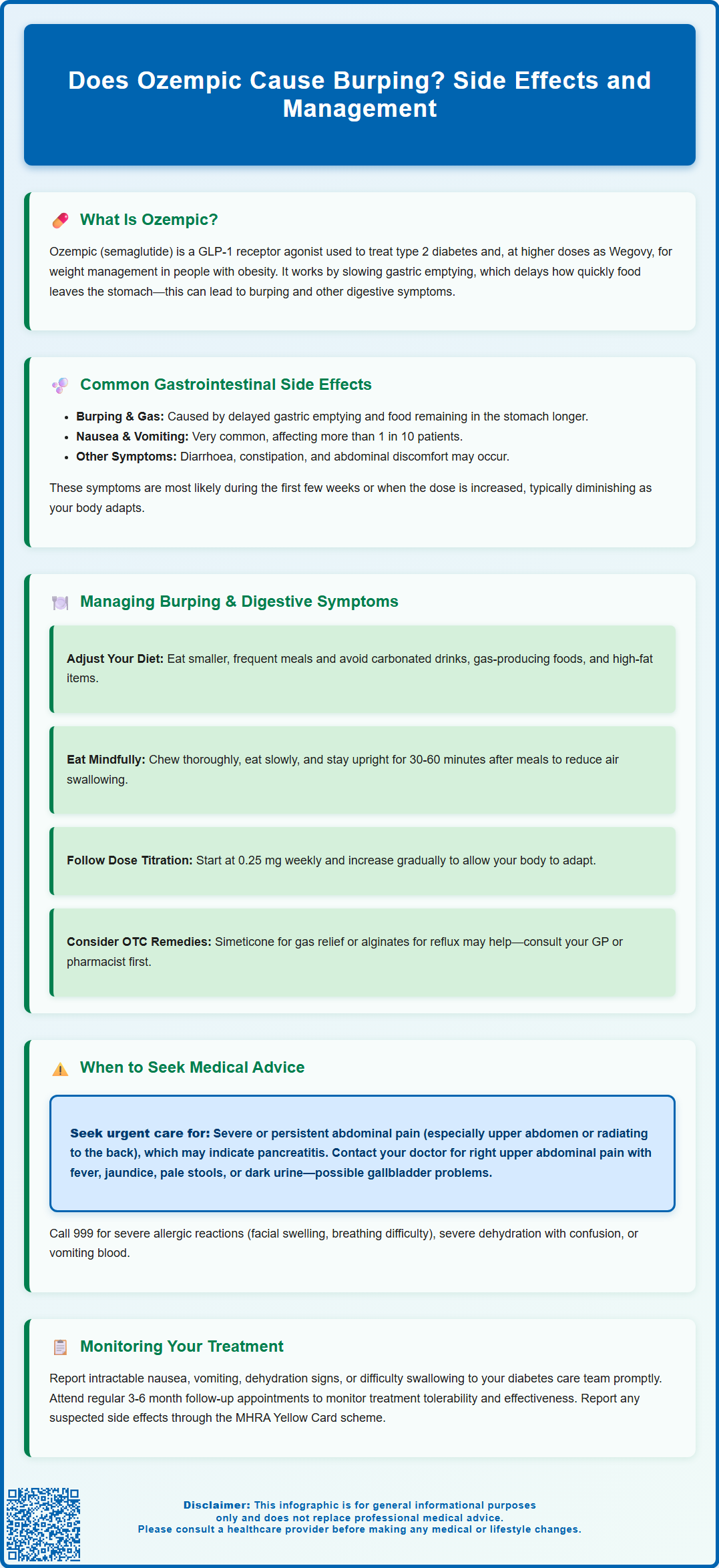
Does Ozempic cause burping? Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management. Burping, or eructation, can occur as part of the gastrointestinal side effects associated with this medication. Ozempic works by slowing gastric emptying, which may contribute to upper gastrointestinal symptoms including burping, particularly during initial treatment or dose increases. Whilst not separately quantified in UK product information, burping may occur alongside other common gastrointestinal effects such as nausea, vomiting, and abdominal discomfort. Understanding these potential symptoms helps patients and clinicians manage treatment effectively.
Summary: Ozempic can cause burping as part of its gastrointestinal side effects, related to its mechanism of slowing gastric emptying.
- Semaglutide is a GLP-1 receptor agonist that delays gastric emptying, which may contribute to burping and other upper gastrointestinal symptoms.
- Gastrointestinal side effects are very common with Ozempic, affecting more than 1 in 10 patients, particularly during initial treatment and dose escalation.
- Symptoms typically improve over time with dietary modifications such as smaller meals, avoiding carbonated drinks, and following recommended dose titration schedules.
- Seek medical advice if burping is accompanied by severe abdominal pain, persistent vomiting, signs of dehydration, or symptoms suggesting pancreatitis or gallbladder problems.
Table of Contents
Does Ozempic Cause Burping?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus and, at higher doses (marketed as Wegovy), for weight management in adults with obesity or overweight with comorbidities. Gastrointestinal symptoms are amongst the most frequently reported side effects associated with semaglutide therapy.
Burping (eructation) can occur as part of the broader spectrum of gastrointestinal disturbances linked to Ozempic's mechanism of action. According to the MHRA-approved Summary of Product Characteristics (SmPC), semaglutide works by slowing gastric emptying, enhancing insulin secretion in a glucose-dependent manner, and reducing appetite. The delayed gastric emptying may contribute to upper gastrointestinal symptoms, which could include burping or belching in some patients.
Patients initiating Ozempic commonly report symptoms such as nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. While eructation is not specifically quantified for Ozempic in the SmPC, it may occur alongside other gastrointestinal symptoms, particularly in the early weeks of treatment or following dose escalation. Understanding the potential for these symptoms helps patients and healthcare professionals anticipate and manage them effectively during the course of treatment.
How Common Is Burping with Ozempic?
The precise incidence of burping as an isolated symptom with Ozempic is not separately quantified in the product information, as it is typically grouped under broader categories of gastrointestinal adverse effects. However, gastrointestinal side effects overall are very common, affecting more than 1 in 10 patients (≥10%) according to the MHRA-approved product information.
In the clinical trials such as the SUSTAIN programme, nausea was reported as very common (≥1/10), whilst vomiting, diarrhoea, and abdominal pain were common (≥1/100 to <1/10), as documented in the SmPC. Upper gastrointestinal symptoms, which may include burping, are generally associated with the medication's effect on slowing gastric emptying. These symptoms are often most noticeable during the initial titration phase and may diminish over time as the body adapts to the medication.
Several factors may influence the likelihood and severity of gastrointestinal symptoms with Ozempic:
-
Dose escalation: Rapid increases in dose may exacerbate gastrointestinal symptoms
-
Dietary habits: Large meals, carbonated beverages, and fatty foods can worsen gas and burping
-
Individual sensitivity: Some patients are more prone to gastrointestinal side effects than others
-
Concurrent medications: Other drugs affecting gastric motility (such as opioids, anticholinergics, or tricyclic antidepressants) may compound symptoms
According to product information, gastrointestinal adverse reactions are typically transient and usually mild to moderate in severity. Most patients find that symptoms improve with time and appropriate dietary modifications.
Managing Burping and Gastrointestinal Side Effects
Effective management of burping and related gastrointestinal symptoms can significantly improve tolerability and adherence to Ozempic therapy. A combination of lifestyle modifications, dietary adjustments, and appropriate medical support forms the cornerstone of symptom management.
Dietary and lifestyle strategies include:
-
Eating smaller, more frequent meals rather than large portions, which reduces gastric distension
-
Avoiding carbonated drinks and foods that produce excess gas (e.g., beans, cruciferous vegetables, onions)
-
Eating slowly and chewing thoroughly to minimise air swallowing (aerophagia)
-
Limiting high-fat foods, which further delay gastric emptying and may worsen symptoms
-
Staying upright after meals for at least 30–60 minutes to facilitate digestion
-
Avoiding tight clothing around the abdomen that may increase intra-abdominal pressure
Medication management considerations include:
-
Following the recommended dose titration schedule (typically starting at 0.25 mg weekly for four weeks, then 0.5 mg weekly, with potential increases to 1 mg and then 2 mg if needed and tolerated) to allow gradual adaptation
-
Taking Ozempic at a consistent time each week, preferably when dietary intake can be monitored
-
Discussing with your GP, pharmacist or diabetes specialist nurse whether temporary use of over-the-counter remedies such as simeticone (for gas relief) or alginates (for reflux symptoms) might be appropriate
-
Maintaining adequate hydration, particularly if experiencing nausea or diarrhoea
Patients should maintain open communication with their healthcare team throughout treatment. If burping is accompanied by persistent nausea, vomiting, or abdominal pain, a temporary dose reduction or slower titration schedule may be warranted. If symptoms persist or worsen, a review to exclude conditions such as gastroparesis may be needed. NICE guidance (NG28) on type 2 diabetes management emphasises individualised treatment approaches, and adjustments to GLP-1 receptor agonist therapy should be made in consultation with prescribing clinicians.
When to Seek Medical Advice About Ozempic Side Effects
Whilst burping alone is generally a benign and self-limiting symptom, certain circumstances warrant prompt medical evaluation. Patients should be aware of red flag symptoms that may indicate more serious complications or conditions requiring urgent assessment.
Contact your GP or diabetes care team if you experience:
-
Persistent or severe abdominal pain, particularly if localised to the upper abdomen or radiating to the back, which could indicate pancreatitis (a rare but serious adverse effect of GLP-1 receptor agonists)
-
Right upper abdominal pain, with or without fever, jaundice (yellowing of skin/eyes), pale stools or dark urine, which may indicate gallbladder problems
-
Intractable nausea and vomiting preventing adequate oral intake or medication adherence
-
Signs of dehydration, including reduced urine output, dizziness, or dry mucous membranes
-
Unexpected weight loss with poor intake or ongoing vomiting
-
Difficulty swallowing or sensation of food getting stuck, which requires medical assessment
-
Hypoglycaemia symptoms if using Ozempic with sulfonylureas or insulin, especially when food intake is reduced
Seek immediate medical attention (call 999 or attend A&E) if you develop:
-
Severe, persistent abdominal pain with or without vomiting, which may indicate acute pancreatitis
-
Symptoms of allergic reaction, such as facial swelling, difficulty breathing, or widespread rash
-
Severe dehydration with confusion, rapid heartbeat, or inability to keep down fluids
-
Persistent vomiting with blood or coffee-ground appearance
If pancreatitis is suspected, stop taking semaglutide and seek urgent medical assessment, as advised in the product information.
The MHRA's Yellow Card scheme allows patients and healthcare professionals to report suspected adverse drug reactions. Report suspected side effects via the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app. Regular follow-up appointments, typically recommended at 3–6 month intervals for patients on Ozempic, provide opportunities to review tolerability, assess glycaemic control, and adjust treatment as needed.
Frequently Asked Questions
How long does burping from Ozempic typically last?
Burping and other gastrointestinal symptoms are typically most noticeable during the initial titration phase and often diminish over time as the body adapts to the medication. Most patients find symptoms improve within several weeks with appropriate dietary modifications and gradual dose escalation.
Can I take anything to reduce burping whilst on Ozempic?
Discuss with your GP or pharmacist whether over-the-counter remedies such as simeticone for gas relief might be appropriate. Dietary changes including smaller meals, avoiding carbonated drinks, and eating slowly are first-line strategies for managing burping.
Should I stop taking Ozempic if I experience burping?
Burping alone does not usually require stopping Ozempic, as it is generally a benign and self-limiting symptom. However, if accompanied by severe abdominal pain, persistent vomiting, or other concerning symptoms, contact your healthcare team for advice on whether dose adjustment or further assessment is needed.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript