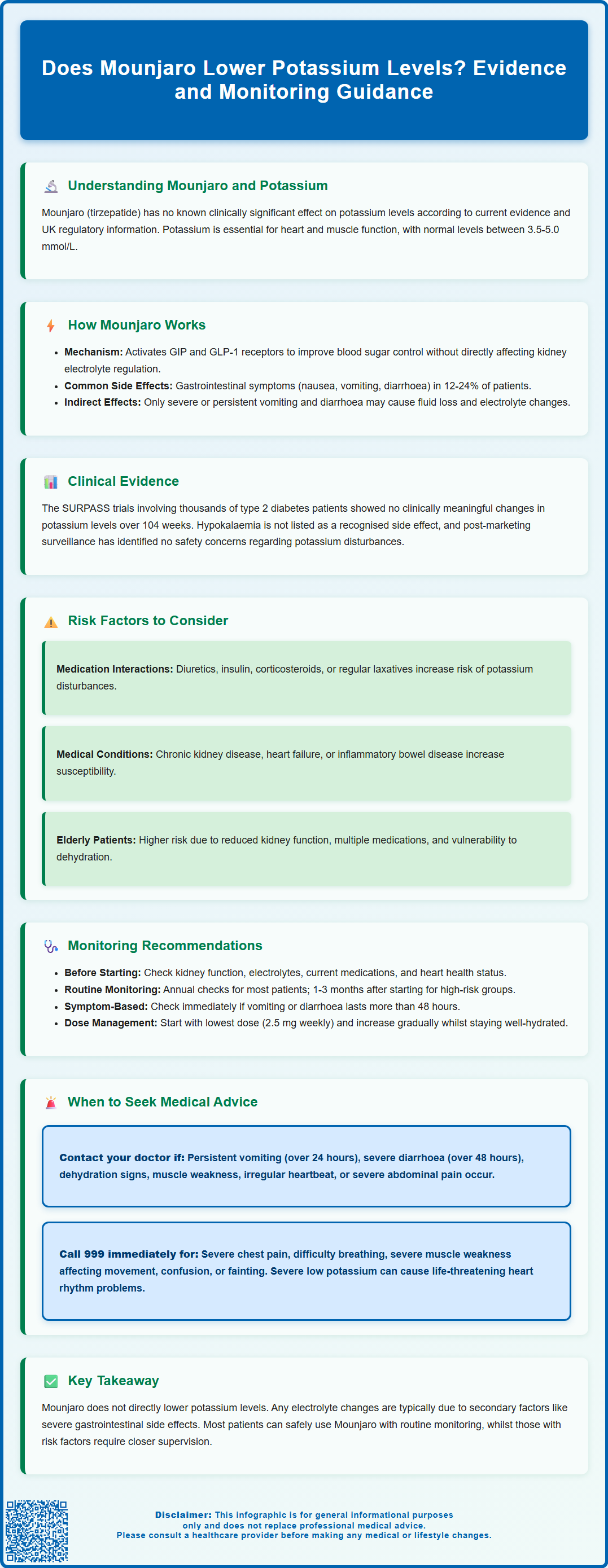
Does Mounjaro lower potassium levels? This is a common concern for patients and clinicians considering tirzepatide therapy. Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Based on current evidence from clinical trials and regulatory data, Mounjaro does not directly lower potassium levels. The MHRA Summary of Product Characteristics does not list hypokalaemia as a recognised adverse effect. However, gastrointestinal symptoms such as nausea, vomiting, or diarrhoea may indirectly affect electrolyte balance through dehydration. This article examines the evidence, explores potential mechanisms, and provides guidance on appropriate monitoring for patients receiving Mounjaro.
Summary: Mounjaro (tirzepatide) does not directly lower potassium levels, and hypokalaemia is not a recognised adverse effect in clinical trials or regulatory guidance.
- Tirzepatide is a dual GIP and GLP-1 receptor agonist with no known direct effect on renal potassium handling or aldosterone activity.
- Gastrointestinal adverse effects (nausea, vomiting, diarrhoea) may indirectly affect electrolytes through dehydration in susceptible patients.
- Clinical trials and post-marketing surveillance have not identified hypokalaemia as a significant safety signal with Mounjaro therapy.
- Patients with severe gastrointestinal symptoms, concurrent diuretics, renal impairment, or elderly individuals may warrant enhanced electrolyte monitoring.
- Baseline and periodic electrolyte assessment is advisable, particularly in at-risk groups or when persistent gastrointestinal symptoms occur.
- Seek medical advice for persistent vomiting, severe diarrhoea, muscle weakness, palpitations, or signs of dehydration whilst taking Mounjaro.
Table of Contents
Understanding Mounjaro and Potassium Levels
Mounjaro (tirzepatide) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. As with any medication that affects metabolic processes, patients and healthcare professionals often enquire about its potential effects on electrolyte balance, particularly potassium levels.
Potassium is a vital electrolyte that plays a crucial role in maintaining normal cellular function, particularly in cardiac and skeletal muscle. Normal serum potassium levels typically range between 3.5 and 5.0 mmol/L. Both hypokalaemia (low potassium) and hyperkalaemia (high potassium) can have serious clinical consequences, including cardiac arrhythmias and muscle weakness.
Based on current evidence, including the Medicines and Healthcare products Regulatory Agency (MHRA) Summary of Product Characteristics, there is no known clinically significant effect of Mounjaro on potassium levels. The prescribing information for tirzepatide does not list hypokalaemia as a recognised adverse effect. Any changes in potassium levels during treatment are more likely to be secondary to gastrointestinal symptoms or dehydration rather than a direct effect of the medication.
This article examines the available evidence regarding Mounjaro's effects on potassium levels, explores potential mechanisms that might theoretically influence electrolyte balance, and provides guidance on appropriate monitoring and management strategies for patients receiving this treatment.
How Mounjaro Affects Electrolyte Balance
Mounjaro works by activating both GIP and GLP-1 receptors, which enhances glucose-dependent insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite. These mechanisms primarily target glycaemic control and weight management rather than directly affecting renal electrolyte handling.
The most common adverse effects of Mounjaro relate to the gastrointestinal system and include:
-
Nausea and vomiting (reported in 12-24% of patients, dose-dependent)
-
Diarrhoea (occurring in 7-20% of patients, dose-dependent)
-
Decreased appetite
-
Abdominal discomfort
These gastrointestinal effects represent the primary theoretical pathway through which Mounjaro might indirectly influence electrolyte balance. Persistent vomiting or severe diarrhoea can lead to fluid and electrolyte losses, potentially affecting potassium levels. In susceptible patients, severe gastrointestinal symptoms can precipitate dehydration and acute kidney injury, which may further disrupt electrolyte balance.
Unlike some other diabetes medications, such as insulin (which can drive potassium into cells and potentially cause hypokalaemia) or certain diuretics (which increase renal potassium excretion), Mounjaro has no known direct effect on renal tubular potassium handling or aldosterone activity, which are the primary regulators of potassium balance in the body.
Patients who experience mild gastrointestinal symptoms that resolve quickly are unlikely to develop electrolyte disturbances. The risk becomes relevant primarily in cases of severe or prolonged symptoms requiring medical intervention.
Clinical Evidence on Mounjaro and Potassium
The clinical development programme for tirzepatide included several large-scale randomised controlled trials, collectively known as the SURPASS studies, which enrolled thousands of patients with type 2 diabetes. These trials provided comprehensive safety data, including monitoring of laboratory parameters such as electrolytes.
Review of the published trial data and the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA) reveals that hypokalaemia was not identified as a significant adverse event during clinical trials. Electrolyte disturbances were not reported among the common or uncommon adverse reactions associated with tirzepatide therapy.
The SURPASS trials, which compared Mounjaro against placebo and active comparators including semaglutide and insulin, monitored patients for up to 40-104 weeks depending on the specific trial. Laboratory assessments included regular measurement of serum electrolytes. No clinically meaningful changes in potassium levels were observed in the treatment groups compared to control groups.
Post-marketing surveillance data from real-world use has similarly not identified hypokalaemia as an emerging safety signal. The European Medicines Agency (EMA) and MHRA continue to monitor adverse event reports, and neither regulatory body has issued warnings regarding potassium disturbances with tirzepatide.
It is worth noting that patients in clinical trials are typically well-monitored with regular laboratory assessments, which may not reflect real-world practice. Additionally, rare idiosyncratic events can occur despite the absence of a clear signal in clinical trials. However, the absence of signals from both controlled trials and post-marketing surveillance provides reassurance that clinically significant effects on potassium levels are not a characteristic feature of Mounjaro therapy. Any electrolyte changes that do occur are more likely attributable to secondary factors such as dehydration from gastrointestinal adverse effects rather than direct drug effects.
Risk Factors for Potassium Changes During Treatment
Whilst Mounjaro itself does not directly lower potassium levels, certain patient populations and clinical scenarios may warrant increased vigilance regarding electrolyte monitoring during treatment.
Patients experiencing severe gastrointestinal adverse effects represent the primary at-risk group. Those with persistent vomiting, severe diarrhoea, or significantly reduced oral intake may develop dehydration and secondary electrolyte disturbances. This risk is highest during the initial weeks of treatment or following dose escalation, when gastrointestinal symptoms are most pronounced.
Concurrent medications that affect potassium balance require consideration:
-
Diuretics (particularly loop and thiazide diuretics) increase renal potassium losses
-
Insulin therapy can shift potassium intracellularly
-
Corticosteroids may promote potassium excretion
-
Laxatives used regularly can contribute to gastrointestinal potassium losses
-
ACE inhibitors, ARBs, and potassium-sparing diuretics (such as spironolactone, eplerenone, amiloride) can increase potassium levels and may complicate management
Pre-existing medical conditions may increase susceptibility to electrolyte disturbances:
-
Chronic kidney disease (reduced capacity to regulate potassium)
-
Heart failure (often managed with multiple medications affecting electrolytes)
-
Adrenal insufficiency (impaired aldosterone regulation, typically predisposing to hyperkalaemia)
-
Inflammatory bowel disease (baseline increased gastrointestinal losses)
Elderly patients may be at higher risk due to age-related changes in renal function, polypharmacy, and reduced physiological reserve. They may also be more susceptible to dehydration if fluid intake is inadequate during periods of gastrointestinal upset.
Patients with poorly controlled diabetes experiencing frequent hyperglycaemia and glycosuria may have pre-existing electrolyte disturbances that require monitoring as glycaemic control improves with Mounjaro therapy. The correction of hyperglycaemia itself can sometimes reveal or unmask electrolyte abnormalities.
Monitoring and Managing Electrolytes on Mounjaro
The National Institute for Health and Care Excellence (NICE) provides guidance on the management of type 2 diabetes (NG28), including the use of GLP-1 receptor agonists. Whilst routine electrolyte monitoring is not specifically mandated for patients on Mounjaro in the absence of risk factors, a pragmatic approach to monitoring is advisable.
Baseline assessment before initiating Mounjaro should include:
-
Renal function tests (estimated glomerular filtration rate)
-
Serum electrolytes including potassium
-
Review of concurrent medications
-
Assessment of cardiovascular status
Ongoing monitoring recommendations include:
-
Routine follow-up: For uncomplicated patients without risk factors, electrolyte monitoring can follow standard diabetes care protocols, typically annually or as clinically indicated
-
Enhanced monitoring: Patients with risk factors (renal impairment, concurrent diuretics, elderly) should have electrolytes checked 1-3 months after initiation and following dose escalations, following local protocols
-
Symptomatic monitoring: Any patient experiencing persistent gastrointestinal symptoms, particularly vomiting or diarrhoea lasting more than 48 hours, should have electrolytes assessed
Management strategies for patients on Mounjaro include:
-
Dose titration: Following the recommended gradual dose escalation schedule (starting at 2.5 mg weekly for 4 weeks, then increasing to 5 mg, with further increases in 2.5 mg increments to 10-15 mg as needed) helps minimise gastrointestinal adverse effects
-
Non-pharmacological measures: Eating smaller, more frequent meals and maintaining adequate hydration may help reduce gastrointestinal symptoms
-
Symptomatic treatment: If non-pharmacological measures are insufficient, antiemetics may be considered for persistent nausea, though should be used judiciously with consideration of potential QT interval effects and drug interactions
-
Hydration advice: Patients should be counselled to maintain adequate fluid intake, particularly during the initial treatment period
If electrolyte disturbances are identified, management should address the underlying cause. Temporary dose reduction or treatment interruption may be necessary in cases of severe gastrointestinal symptoms with dehydration. Electrolyte replacement should follow local protocols, with potassium supplementation typically considered if levels fall below 3.0 mmol/L, or at higher levels if the patient is symptomatic or has cardiac risk factors. Caution is needed when supplementing potassium in patients with impaired renal function.
When to Seek Medical Advice
Patients prescribed Mounjaro should be educated about symptoms that warrant medical attention. Whilst serious electrolyte disturbances are uncommon, early recognition and intervention can prevent complications.
Contact your GP or healthcare professional promptly if you experience:
-
Persistent vomiting (unable to keep down fluids for more than 24 hours)
-
Severe or prolonged diarrhoea (lasting more than 48 hours)
-
Signs of dehydration: excessive thirst, dark urine, dizziness, reduced urine output
-
Muscle weakness or cramps (particularly if severe or persistent)
-
Irregular heartbeat or palpitations
-
Unusual fatigue or lethargy
-
Severe persistent abdominal pain, especially if radiating to the back (may suggest pancreatitis)
Seek urgent medical attention (call 999 or attend A&E) if you develop:
-
Severe chest pain or pressure
-
Difficulty breathing or shortness of breath
-
Severe muscle weakness affecting mobility
-
Confusion or altered consciousness
-
Fainting or collapse
These symptoms may indicate significant electrolyte disturbances or other serious complications requiring immediate assessment. Hypokalaemia, when severe (potassium <2.5 mmol/L), can cause life-threatening cardiac arrhythmias and requires urgent treatment.
Regular medication reviews with your GP or diabetes specialist nurse are important to ensure Mounjaro remains appropriate and well-tolerated. Inform your healthcare team about any new medications, including over-the-counter preparations and supplements, as these may interact or affect electrolyte balance.
Patients should not discontinue Mounjaro without medical advice, but if gastrointestinal symptoms are significantly affecting quality of life or causing concern, discuss this with your healthcare professional. Dose adjustment or alternative treatment options can be considered. Maintaining open communication with your diabetes care team ensures safe and effective management of your condition whilst minimising the risk of complications.
If you suspect you are experiencing side effects from Mounjaro, you can report these through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
Frequently Asked Questions
Can Mounjaro cause low potassium levels?
Mounjaro does not directly cause low potassium levels. Clinical trials and regulatory data show no significant effect on potassium. However, severe gastrointestinal side effects such as persistent vomiting or diarrhoea may indirectly lead to electrolyte disturbances through dehydration.
Do I need regular blood tests to check potassium whilst taking Mounjaro?
Routine potassium monitoring is not specifically required for all patients on Mounjaro. However, baseline electrolytes are advisable before starting treatment, and enhanced monitoring may be recommended if you have risk factors such as kidney disease, take diuretics, are elderly, or experience persistent gastrointestinal symptoms.
What symptoms suggest an electrolyte problem whilst on Mounjaro?
Contact your GP if you experience persistent vomiting or diarrhoea lasting more than 24-48 hours, signs of dehydration, muscle weakness or cramps, irregular heartbeat, or unusual fatigue. These may indicate electrolyte disturbances requiring medical assessment and possible treatment adjustment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript