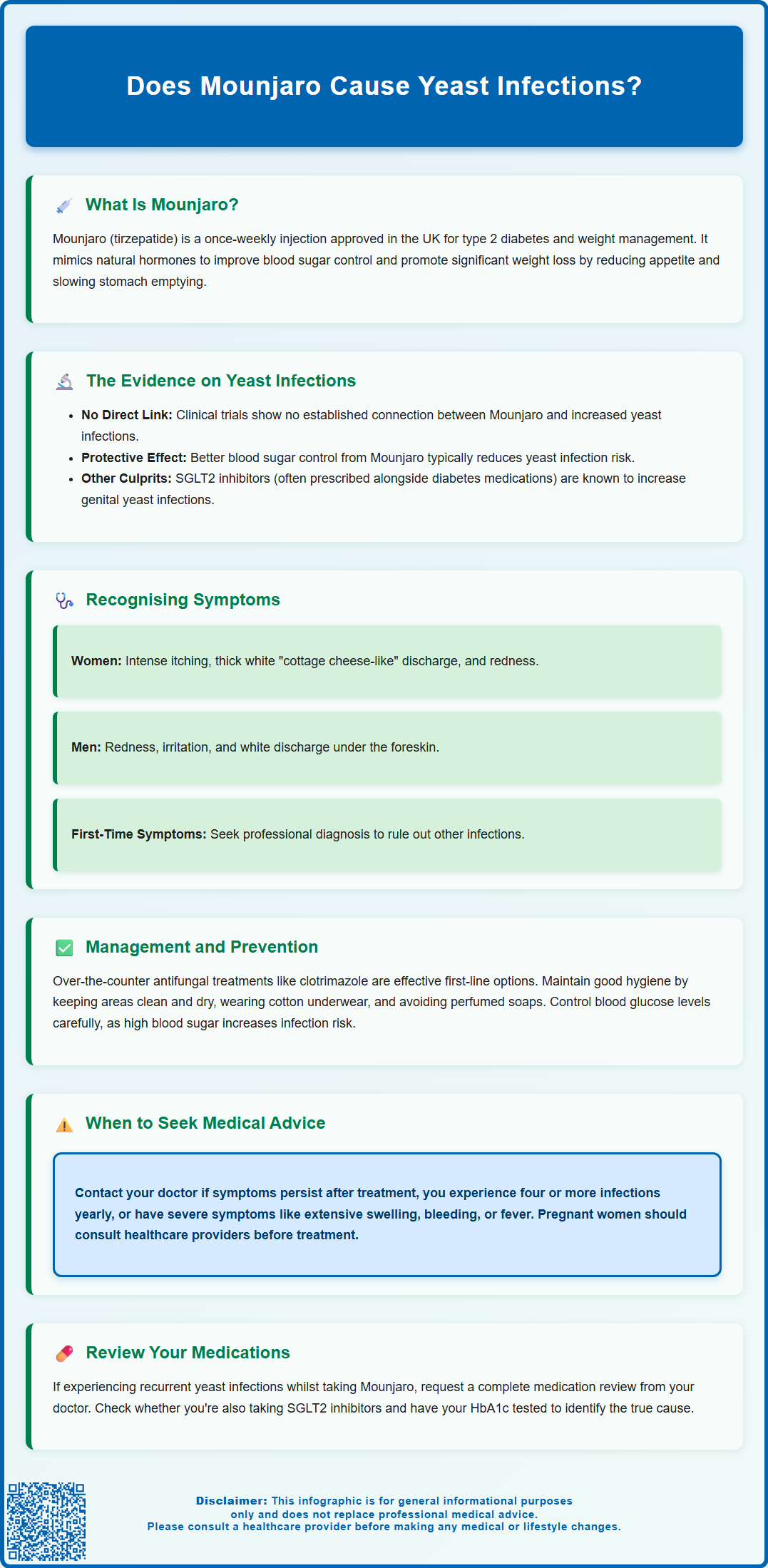
Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management. Whilst some patients wonder whether Mounjaro causes yeast infections, there is no established causal link in clinical trials or product literature. However, understanding the relationship between diabetes medications, blood glucose control, and infection risk is important. This article examines the evidence, explores why yeast infections might occur during treatment, and provides guidance on recognition, management, and when to seek medical advice.
Summary: Mounjaro (tirzepatide) is not established to cause yeast infections, and improved glycaemic control typically reduces infection risk.
- Mounjaro is a dual GIP and GLP-1 receptor agonist for type 2 diabetes and weight management, administered as a once-weekly subcutaneous injection.
- No causal link exists between Mounjaro and increased yeast infection risk in clinical trials or product literature.
- Improved blood glucose control from Mounjaro generally reduces yeast infection risk, as high glucose levels favour Candida growth.
- Concomitant SGLT2 inhibitors (not Mounjaro) are known to increase genital candidiasis risk due to increased urinary glucose.
- Recurrent yeast infections warrant medical review to assess glycaemic control, medication regimen, and underlying contributing factors.
- Seek GP advice if symptoms persist after antifungal treatment, recur frequently, or are accompanied by unusual discharge or systemic symptoms.
Table of Contents
What Is Mounjaro and How Does It Work?
Mounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with weight-related comorbidities, alongside diet and physical activity. It belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists.
The mechanism of action involves mimicking two naturally occurring incretin hormones that regulate blood glucose and appetite. By activating both GIP and GLP-1 receptors, Mounjaro enhances insulin secretion in response to meals, suppresses glucagon release (which reduces glucose production by the liver), slows gastric emptying, and promotes satiety. This dual action results in improved glycaemic control and significant weight loss in many patients.
Mounjaro is administered as a once-weekly subcutaneous injection, typically starting at a low dose (2.5 mg) and gradually titrated upwards to minimise gastrointestinal side effects. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved doses ranging from 2.5 mg to 15 mg, depending on individual response and tolerability.
Common adverse effects include nausea, vomiting, diarrhoea, constipation, abdominal pain, and decreased appetite—most of which are gastrointestinal in nature and tend to diminish over time. The risk of hypoglycaemia is increased when used alongside insulin or sulfonylureas. Other safety considerations include potential risks of pancreatitis and gallbladder disease. Patients using oral contraceptives should be aware that the delayed gastric emptying effect may reduce contraceptive efficacy during treatment initiation or dose escalation, and additional contraceptive measures may be needed. Understanding how Mounjaro works helps contextualise any potential secondary effects, including changes that might influence infection risk.
Why Might Yeast Infections Occur With Mounjaro?
There is no established causal link between Mounjaro (tirzepatide) and an increased risk of yeast infections (candidiasis) in the product literature or clinical trials. However, several factors may explain why some patients might experience yeast infections whilst taking this medication.
Primarily, improved glycaemic control is generally beneficial for reducing yeast infection risk. Patients with poorly controlled type 2 diabetes often experience recurrent yeast infections due to elevated blood glucose levels, which create a favourable environment for Candida species to thrive. As Mounjaro improves blood glucose control, this should typically reduce the risk of candidiasis over time.
Importantly, concomitant medications may be responsible for any observed increase in yeast infections. SGLT2 inhibitors (such as dapagliflozin, empagliflozin, or canagliflozin), which are often prescribed alongside other diabetes treatments, are known to increase the risk of genital candidiasis due to increased glucose in urine. If you are taking both an SGLT2 inhibitor and Mounjaro, the SGLT2 inhibitor may be the more likely cause of any yeast infections.
Individual patient factors—including immune status, hygiene practices, antibiotic use, hormonal changes, and pre-existing conditions—play significant roles in yeast infection risk. It is important to consider the broader clinical context rather than attributing symptoms solely to one medication.
If you are experiencing recurrent infections, a thorough review of all medications and underlying health conditions with your GP or diabetes specialist is advisable. They can assess your overall glycaemic control through HbA1c testing and review your complete medication regimen to identify potential contributors.
Recognising and Managing Yeast Infections
Yeast infections, most commonly caused by Candida albicans, can affect various parts of the body, but vulvovaginal candidiasis in women and balanitis (inflammation of the glans penis) in men are the most frequent presentations. Recognising the symptoms early enables prompt and effective management.
Common symptoms of vulvovaginal candidiasis include:
-
Intense itching and irritation around the vagina and vulva
-
Thick, white, "cottage cheese-like" vaginal discharge (usually odourless)
-
Redness, swelling, and soreness of the vulval area
-
Pain or discomfort during sexual intercourse or urination
In men, symptoms of candidal balanitis may include:
-
Redness, irritation, or a rash on the glans or foreskin
-
Itching or burning sensation
-
White discharge under the foreskin
-
Difficulty retracting the foreskin (in severe cases)
Oral thrush (oropharyngeal candidiasis) can also occur, presenting as white patches on the tongue, inner cheeks, or throat, often accompanied by soreness or difficulty swallowing.
Management strategies typically involve:
-
Antifungal treatments: Over-the-counter options such as clotrimazole pessaries or cream (for vaginal infections) are first-line treatments in the UK. Oral fluconazole capsules may be available from pharmacies under certain conditions or by prescription, but should be avoided during pregnancy (topical azoles are preferred for pregnant women).
-
Good hygiene practices: Keeping affected areas clean and dry, wearing breathable cotton underwear, and avoiding irritants such as perfumed soaps or douches.
-
Glycaemic control: Ensuring optimal blood glucose management, as persistently high levels can predispose to recurrent infections.
-
Probiotic support: Some evidence suggests that probiotics might help restore healthy microbial balance, though evidence is limited and inconsistent. Probiotics should complement, not replace, standard antifungal treatment.
If symptoms persist beyond a week of treatment, recur frequently (more than four times per year), or are accompanied by unusual discharge or systemic symptoms, further medical evaluation is necessary.
When to Seek Medical Advice
Whilst many yeast infections can be managed with over-the-counter treatments, certain circumstances warrant prompt medical consultation to rule out complications or alternative diagnoses.
You should contact your GP or healthcare professional if:
-
Symptoms do not improve after a full course of antifungal treatment (typically 1–7 days, depending on the product)
-
You experience recurrent infections (four or more episodes within 12 months), which may indicate underlying issues such as uncontrolled diabetes, immunosuppression, or antibiotic overuse
-
You develop severe symptoms, including extensive swelling, ulceration, or bleeding
-
You notice unusual or foul-smelling discharge, which could suggest bacterial vaginosis or a sexually transmitted infection rather than candidiasis
-
You experience systemic symptoms such as fever, chills, or feeling generally unwell, which may indicate a more serious infection
-
You are pregnant, as oral antifungals like fluconazole should be avoided; topical treatments are preferred during pregnancy
-
You are unsure of the diagnosis—if this is your first suspected yeast infection, it is advisable to have it confirmed by a healthcare professional
For patients taking Mounjaro, it is also important to discuss any new or recurrent infections with your diabetes specialist or prescribing clinician. They can review your overall diabetes management plan, assess glycaemic control through HbA1c testing, and consider whether any medication adjustments (particularly if you are also taking SGLT2 inhibitors) are needed.
NICE guidance recommends that individuals with diabetes who experience recurrent infections should have their blood glucose control optimised and be screened for other potential contributing factors. Your healthcare team can provide tailored advice on infection prevention, including lifestyle modifications and, if necessary, referral to specialist services such as genitourinary medicine (GUM) clinics for persistent or complex cases.
If you suspect that Mounjaro or any other medication may be causing side effects, you can report this through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk), which helps monitor medication safety in the UK.
Remember, open communication with your healthcare professionals about all symptoms and concerns ensures comprehensive, safe, and effective care whilst taking Mounjaro or any other medication.
Scientific References
- Mounjaro - Assessment report.
- Mounjaro KwikPen 2.5mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Diabetic foot problems: prevention and management. NG19.
- Thrush in men and women.
- Tirzepatide Once Weekly for the Treatment of Obesity.
- Incidence and risk of vaginal candidiasis associated with sodium-glucose co-transporter-2 inhibitors.
Frequently Asked Questions
Can Mounjaro increase the risk of yeast infections?
There is no established causal link between Mounjaro (tirzepatide) and increased yeast infection risk. In fact, improved glycaemic control from Mounjaro typically reduces infection risk, as high blood glucose levels favour Candida growth.
What should I do if I develop a yeast infection whilst taking Mounjaro?
Most yeast infections can be treated with over-the-counter antifungal treatments such as clotrimazole. If symptoms persist after treatment, recur frequently, or are severe, contact your GP for further evaluation and to review your diabetes medication regimen.
Could other diabetes medications be causing yeast infections instead of Mounjaro?
Yes, SGLT2 inhibitors (such as dapagliflozin or empagliflozin) are known to increase genital yeast infection risk due to increased glucose in urine. If you take both an SGLT2 inhibitor and Mounjaro, the SGLT2 inhibitor is the more likely cause of any yeast infections.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript