Mounjaro (tirzepatide) is a once-weekly injectable medication licensed in the UK for type 2 diabetes mellitus and weight management in adults with obesity or overweight with comorbidities. As a dual GIP and GLP-1 receptor agonist, it enhances glycaemic control and promotes weight reduction. Whilst Mounjaro demonstrates significant clinical efficacy, some patients report skin reactions, including rashes. Understanding whether Mounjaro causes rashes, their types, frequency, and management is essential for patient safety and informed decision-making. This article provides evidence-based guidance on dermatological reactions associated with Mounjaro, when to seek medical attention, and practical strategies for prevention and management.
Summary: Mounjaro can cause rashes, most commonly mild injection site reactions affecting 1 in 10 to 1 in 100 patients, whilst generalised rashes are uncommon.
- Tirzepatide is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management.
- Injection site reactions (redness, itching, swelling) are common and typically self-limiting within days.
- Generalised rashes including urticaria and maculopapular eruptions are uncommon hypersensitivity reactions.
- Angioedema, facial swelling, or breathing difficulties require immediate emergency medical attention.
- Proper injection technique, site rotation, and room-temperature medication help prevent skin reactions.
- Report suspected adverse effects via the MHRA Yellow Card scheme for ongoing pharmacovigilance.
Table of Contents
Understanding Mounjaro and Skin Reactions
Mounjaro (tirzepatide) is a once-weekly injectable medication licensed in the UK for the treatment of type 2 diabetes mellitus. Tirzepatide is also authorised for weight management in adults with obesity or overweight with weight-related comorbidities, though this may be under the brand name Zepbound rather than Mounjaro. As a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, Mounjaro works by enhancing insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite. Whilst the medication has demonstrated significant efficacy in glycaemic control and weight reduction, patients and healthcare professionals should be aware of potential adverse effects, including dermatological reactions.
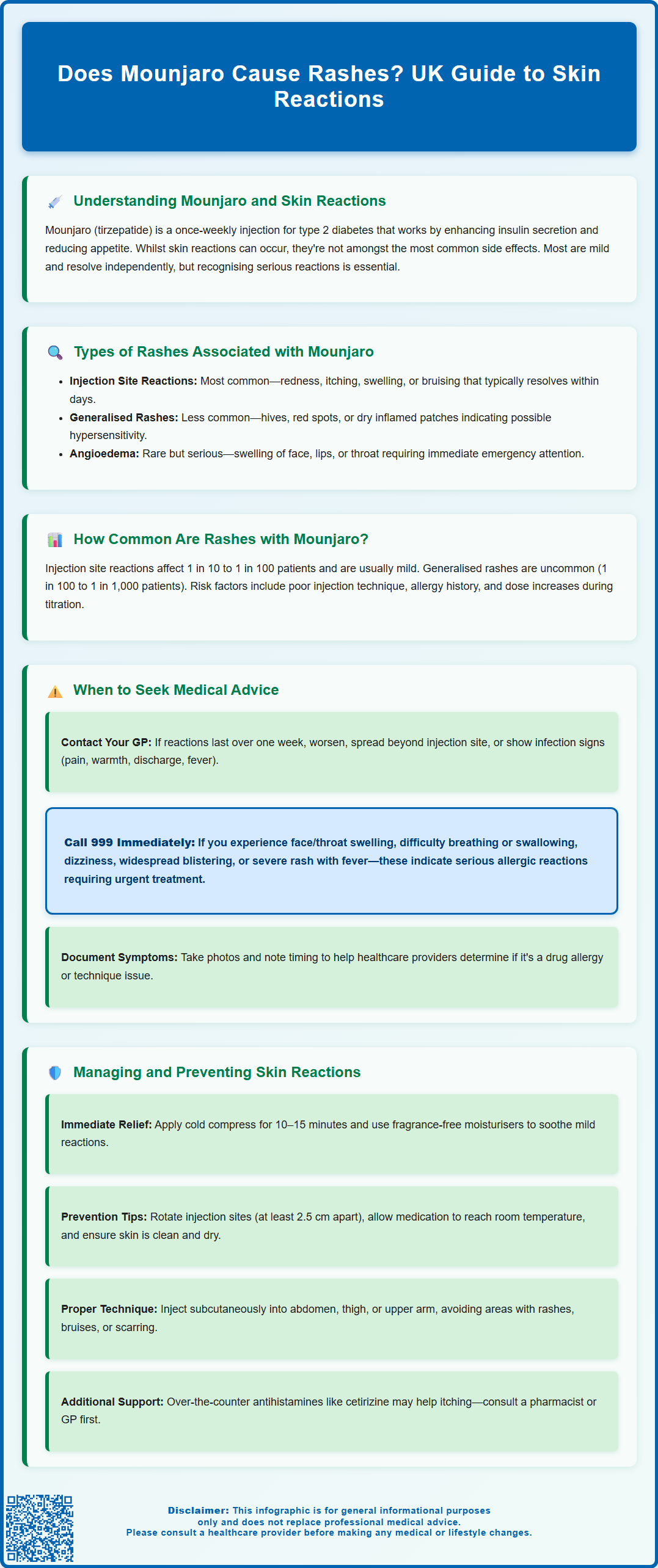
Skin reactions, including rashes, have been reported by some individuals using Mounjaro, though they are not amongst the most commonly documented side effects. The mechanism by which tirzepatide might trigger cutaneous reactions is not fully established, but possibilities include localised injection site reactions, hypersensitivity responses, or idiosyncratic immune-mediated phenomena. It is important to distinguish between injection site reactions—which are relatively common with subcutaneous medications—and more generalised or systemic rashes that may indicate an allergic or hypersensitivity reaction.
Understanding the nature and frequency of these skin reactions is essential for appropriate patient counselling and clinical management. Whilst most dermatological side effects are mild and self-limiting, recognising when a rash may signify a more serious reaction is crucial for patient safety. This article provides evidence-based guidance on the types of rashes associated with Mounjaro, their prevalence, and practical advice on management and when to seek medical attention.
Types of Rashes Associated with Mounjaro
Skin reactions associated with Mounjaro can be broadly categorised into localised injection site reactions and generalised or systemic rashes. Injection site reactions are the most frequently reported dermatological adverse effects and typically manifest as:
-
Erythema (redness) at the injection site
-
Pruritus (itching) localised to the area of administration
-
Swelling or induration (hardness) around the injection site
-
Bruising or discolouration
These localised reactions usually appear within hours to days following injection and tend to resolve spontaneously within a few days without specific intervention. They are generally considered mild and are common to many subcutaneous injectable medications.
Generalised rashes are less common but may occur as part of a hypersensitivity reaction. These can present as:
-
Urticaria (hives)—raised, itchy welts that may appear anywhere on the body
-
Maculopapular rash—flat or slightly raised red spots that may become confluent
-
Generalised pruritus—itching without visible rash
-
Eczematous reactions—dry, scaly, inflamed patches of skin
In rare instances, more serious dermatological reactions such as angioedema (swelling of deeper skin layers, particularly around the face, lips, or throat) may occur. Angioedema represents a medical emergency requiring immediate attention. Severe cutaneous adverse reactions such as Stevens-Johnson syndrome or toxic epidermal necrolysis are not currently listed in the product information for Mounjaro, though ongoing pharmacovigilance continues for all new medications.
Patients should be educated to differentiate between expected, mild injection site reactions and more concerning systemic manifestations that may require medical evaluation.
How Common Are Rashes with Mounjaro?
According to the UK Summary of Product Characteristics (SmPC) and data submitted to regulatory authorities including the Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA), injection site reactions are classified as a common adverse effect of Mounjaro (affecting between 1 in 10 and 1 in 100 patients). These reactions are typically mild to moderate in severity and rarely lead to treatment discontinuation.
Generalised rashes and hypersensitivity reactions are classified as uncommon (affecting between 1 in 100 and 1 in 1,000 patients). It is important to note that clinical trial populations may not fully represent real-world diversity, and post-marketing surveillance continues to monitor the true incidence of adverse effects in broader patient populations.
Several factors may influence an individual's likelihood of experiencing skin reactions with Mounjaro:
-
Injection technique—improper administration may increase local irritation
-
Individual sensitivity—personal or family history of allergies or atopic conditions
-
Dose escalation—reactions may be more common during titration phases
Whilst rashes are not amongst the most frequently reported side effects of Mounjaro—gastrointestinal symptoms such as nausea, vomiting, and diarrhoea are far more common—dermatological reactions do occur and should be taken seriously. Most injection site reactions are self-limiting and do not require treatment cessation, but persistent, worsening, or generalised rashes warrant clinical assessment to exclude more significant hypersensitivity or allergic phenomena.
When to Seek Medical Advice About Rashes
Patients using Mounjaro should be counselled on when to seek medical advice regarding skin reactions. Whilst mild injection site reactions are generally manageable at home, certain features indicate the need for professional assessment.
Contact your GP or healthcare provider if you experience:
-
Persistent injection site reactions lasting more than one week
-
Worsening local symptoms despite conservative measures
-
Spreading rash beyond the injection site
-
Generalised urticaria (hives) or widespread itching
-
Signs of infection at the injection site—increasing pain, warmth, purulent discharge, or fever
-
Recurrent reactions with each injection that are progressively more severe
Seek immediate medical attention (call 999 or attend A&E) if you develop:
-
Angioedema—swelling of the face, lips, tongue, or throat
-
Difficulty breathing or swallowing
-
Dizziness, light-headedness, or feeling faint (possible anaphylaxis)
-
Widespread blistering or skin peeling
-
Severe generalised rash with systemic symptoms such as fever or malaise
These symptoms may indicate a serious hypersensitivity reaction requiring urgent intervention. Anaphylaxis, though rare with Mounjaro, is a medical emergency necessitating immediate administration of intramuscular adrenaline and emergency care.
For non-urgent concerns, patients should document the nature, timing, and progression of any rash, ideally with photographs, to assist clinical assessment. Healthcare professionals may need to evaluate whether the reaction represents a true drug hypersensitivity, an injection technique issue, or an unrelated dermatological condition. In some cases, temporary treatment interruption or permanent discontinuation may be necessary, particularly if hypersensitivity is confirmed. Alternative glucose-lowering or weight management therapies can be considered in consultation with the prescribing clinician.
Managing and Preventing Skin Reactions
Management of mild injection site reactions typically involves conservative, supportive measures:
-
Cold compress—apply a clean, cool compress to the affected area for 10–15 minutes to reduce inflammation and discomfort
-
Topical emollients—use fragrance-free moisturisers to soothe dry or irritated skin
-
Avoid scratching—this may worsen inflammation and increase infection risk
-
Over-the-counter antihistamines—oral antihistamines such as cetirizine or loratadine may help relieve itching (consult a pharmacist or GP before use)
Preventive strategies to minimise injection site reactions include:
-
Proper injection technique—ensure the medication is administered subcutaneously (not intramuscularly) into appropriate sites (abdomen, thigh, or upper arm)
-
Rotate injection sites—avoid injecting into the same area repeatedly; maintain at least 2.5 cm distance from previous injection sites
-
Room temperature medication—allow Mounjaro to reach room temperature before injection as directed in the Patient Information Leaflet
-
Clean, dry skin—ensure the injection site is clean and completely dry before administration
-
Avoid areas of active skin conditions—do not inject into areas with rashes, bruises, or scarring
For patients experiencing recurrent or bothersome reactions, healthcare professionals may consider:
-
Reviewing injection technique with a practice nurse or diabetes specialist nurse
-
Assessing for potential allergies to excipients in the formulation
-
Prescribing topical corticosteroids for localised inflammatory reactions (on clinician advice and for short-term use only)
-
Evaluating alternative GLP-1 receptor agonists if reactions persist despite optimal technique
Report suspected side effects via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app. Maintaining open communication with healthcare providers ensures appropriate management and optimises treatment outcomes whilst minimising adverse effects.
Frequently Asked Questions
How common are rashes with Mounjaro?
Injection site reactions are common with Mounjaro, affecting between 1 in 10 and 1 in 100 patients. Generalised rashes are uncommon, occurring in 1 in 100 to 1 in 1,000 patients.
What should I do if I develop a rash whilst using Mounjaro?
Mild injection site reactions can be managed with cold compresses and emollients. Contact your GP if the rash spreads, persists beyond one week, or worsens, and seek immediate medical attention for facial swelling or breathing difficulties.
Can I prevent skin reactions when injecting Mounjaro?
Rotate injection sites, allow the medication to reach room temperature before use, ensure proper subcutaneous technique, and inject into clean, dry skin away from areas with existing skin conditions.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript