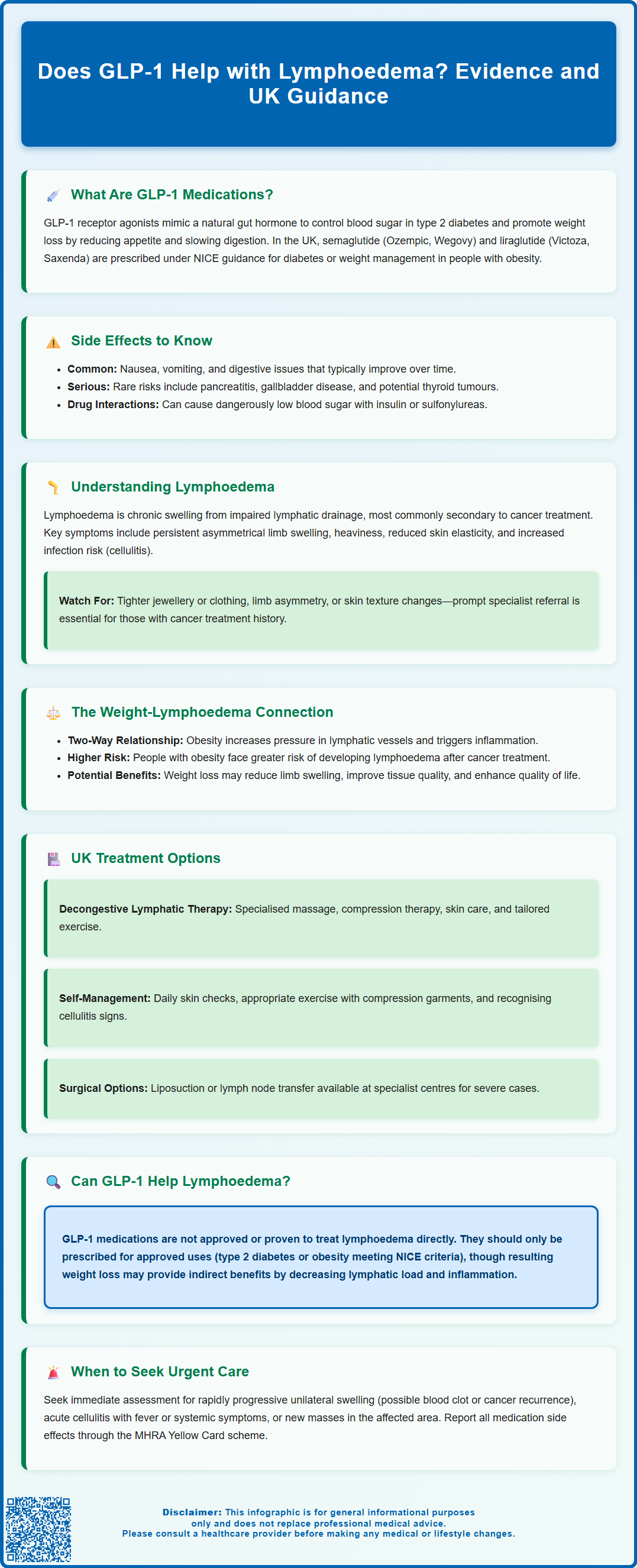
Lymphoedema is a chronic condition causing persistent limb swelling due to impaired lymphatic drainage, often following cancer treatment. Obesity significantly increases lymphoedema risk and symptom severity. GLP-1 receptor agonists—medications such as semaglutide and liraglutide—are licensed in the UK for type 2 diabetes and weight management, producing substantial weight loss. Whilst weight reduction may improve lymphoedema symptoms indirectly, there is currently no established evidence that GLP-1 medications directly treat lymphoedema or should be prescribed specifically for this indication. This article examines the potential relationship between GLP-1 therapy, weight loss, and lymphoedema management within current UK clinical guidance.
Summary: There is currently no established evidence that GLP-1 receptor agonists directly treat lymphoedema or are indicated for this condition.
- GLP-1 receptor agonists (semaglutide, liraglutide) are licensed in the UK for type 2 diabetes and weight management, not lymphoedema.
- Obesity increases lymphoedema risk and severity; weight loss may reduce limb volume and improve symptoms indirectly.
- GLP-1 medications produce substantial weight reduction through appetite suppression and metabolic effects.
- Standard lymphoedema management includes decongestive lymphatic therapy, compression, skin care, and exercise.
- GLP-1 therapy should only be prescribed according to licensed indications (diabetes or obesity meeting NICE criteria), with specialist input if lymphoedema coexists.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for managing type 2 diabetes mellitus, though certain formulations are now licensed for weight management in adults with obesity or overweight with weight-related comorbidities. In the UK, medications include semaglutide (Ozempic for diabetes; Wegovy for weight management) and liraglutide (Victoza for diabetes; Saxenda for weight management), prescribed under specific NICE guidance and MHRA regulation.
These medications work by mimicking the action of naturally occurring GLP-1, a hormone released from the intestine in response to food intake. GLP-1 receptor agonists enhance glucose-dependent insulin secretion from pancreatic beta cells, suppress inappropriate glucagon release, and slow gastric emptying. Importantly, they also act on appetite-regulating centres in the hypothalamus, leading to reduced hunger and increased satiety. This multifaceted mechanism results in improved glycaemic control in people with diabetes and significant weight reduction in those using higher doses for obesity management.
Most GLP-1 receptor agonists are administered via subcutaneous injection, typically once weekly (semaglutide, dulaglutide) or once daily (liraglutide), depending on the specific agent. Oral semaglutide (Rybelsus) is also available for type 2 diabetes. Common adverse effects include nausea, vomiting, diarrhoea, and constipation, which are usually transient and improve with dose titration. More serious but rare complications include pancreatitis, gallbladder disease (particularly with rapid weight loss), and potential thyroid C-cell tumours (observed in animal studies). Caution is needed when combining with insulin or sulfonylureas due to hypoglycaemia risk. Patients should report suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Whilst GLP-1 receptor agonists have demonstrated benefits in metabolic health and cardiovascular outcomes in specific populations, their role in conditions beyond diabetes and obesity—such as lymphoedema—remains an area of emerging interest rather than established clinical practice.
Understanding Lymphoedema: Causes and Symptoms
Lymphoedema is a chronic condition characterised by abnormal accumulation of protein-rich fluid in the interstitial tissues, resulting in progressive swelling, typically affecting the limbs. It arises from impaired lymphatic drainage, which may be congenital (primary lymphoedema) or acquired (secondary lymphoedema). In the UK, secondary lymphoedema is more common and frequently develops following cancer treatment, particularly after lymph node dissection or radiotherapy for breast, gynaecological, or urological malignancies.
The condition manifests as persistent, often asymmetrical swelling that may initially be soft and pitting but progresses to firm, non-pitting oedema as fibrotic changes develop. Patients commonly report sensations of heaviness, tightness, or discomfort in the affected limb. The skin may become thickened, with reduced elasticity and increased susceptibility to infection (cellulitis), which can trigger acute inflammatory episodes and further compromise lymphatic function. Left untreated, lymphoedema can significantly impair mobility, body image, and quality of life.
Risk factors for secondary lymphoedema include the extent of lymph node removal, radiation therapy, surgical trauma, obesity, and lack of limb mobility. Obesity is particularly significant, as excess adipose tissue increases lymphatic load and may directly impair lymphatic vessel function through inflammatory mechanisms. Studies suggest that individuals with higher body mass index (BMI) have increased risk of developing lymphoedema and experience more severe symptoms.
Early recognition is crucial. Patients should be advised to monitor for subtle changes such as jewellery or clothing feeling tighter, asymmetry between limbs, or skin texture changes. Prompt referral to specialist lymphoedema services is recommended when lymphoedema is suspected, particularly in those with cancer treatment history. Red flags requiring urgent assessment include rapidly progressive unilateral swelling (consider deep vein thrombosis or cancer recurrence), acute cellulitis with systemic features (requiring immediate antibiotic therapy), or new masses in the affected area.
Weight Loss and Lymphoedema Management
The relationship between obesity and lymphoedema is bidirectional and clinically significant. Excess body weight increases hydrostatic pressure in the venous and lymphatic systems, elevates inflammatory cytokines, and may directly damage lymphatic vessels through lipotoxicity and chronic low-grade inflammation. Observational studies have demonstrated that individuals with obesity are at substantially higher risk of developing lymphoedema following cancer treatment, and those with established lymphoedema experience greater symptom burden and functional impairment when overweight or obese.
Some evidence suggests that weight reduction may be associated with improvements in lymphoedema symptoms. Research indicates that weight loss may reduce limb volume, improve tissue composition, and enhance quality of life in people with lymphoedema, though the evidence base is limited and heterogeneous. Studies examining weight loss interventions in lymphoedema populations have reported potential benefits, including reduced limb circumference and improved mobility in some patients. These improvements likely result from reduced lymphatic load, decreased inflammatory mediators, and enhanced lymphatic vessel function.
Given these observations, there is growing interest in whether GLP-1 receptor agonists, which produce substantial and sustained weight loss, might benefit individuals with lymphoedema. Whilst these medications are not currently licensed or recommended specifically for lymphoedema management, their ability to achieve clinically meaningful weight reduction raises the possibility of indirect benefits through the mechanisms described above. However, there is no official link or established evidence base demonstrating that GLP-1 medications directly treat lymphoedema or should be prescribed for this indication.
Patients with lymphoedema who are overweight or obese should be offered evidence-based weight management support as part of comprehensive care. This includes dietary modification, physical activity programmes tailored to their functional capacity, and behavioural interventions. In selected cases meeting NICE criteria for obesity pharmacotherapy (e.g., semaglutide 2.4mg/Wegovy with BMI ≥35 kg/m² with comorbidities or ≥30 kg/m² with weight-related comorbidities, prescribed through specialist weight management services) or bariatric surgery, these interventions may be considered, with specialist input to ensure safe implementation alongside lymphoedema management strategies. Patients should be monitored for gallbladder symptoms, as rapid weight loss increases the risk of gallstones.
Treatment Options for Lymphoedema in the UK
Management of lymphoedema in the UK follows a structured, multidisciplinary approach centred on conservative therapies, as there is currently no cure for the condition. NHS and specialist services provide comprehensive assessment and individualised treatment plans. The cornerstone of management is decongestive lymphatic therapy (DLT), which comprises four main components:
-
Manual lymphatic drainage (MLD): A specialised massage technique that stimulates lymphatic flow and redirects fluid to functioning lymphatic pathways
-
Compression therapy: Multi-layer bandaging during intensive treatment phases, followed by compression garments for long-term maintenance
-
Skin care: Meticulous hygiene, emollient use, and prompt treatment of skin breaks to prevent cellulitis
-
Exercise: Tailored physical activity programmes that promote lymphatic drainage through muscle pump action whilst wearing compression
Patients should be educated about self-management strategies, including daily skin inspection, appropriate exercise, limb elevation when resting, and recognition of cellulitis symptoms (increased warmth, redness, pain, or systemic features such as fever). Immediate medical attention should be sought if infection is suspected, as prompt antibiotic therapy is essential to prevent complications and progression of lymphoedema. Suspected deep vein thrombosis presenting as unilateral limb swelling requires same-day assessment per NICE guidance.
Adjunctive therapies may include intermittent pneumatic compression devices for home use, weight management programmes (as discussed previously), and psychological support to address the emotional impact of living with a chronic, visible condition. In selected cases of severe, treatment-resistant lymphoedema, surgical options such as liposuction (covered by NICE interventional procedures guidance), lymphaticovenous anastomosis, or vascularised lymph node transfer may be considered at specialist centres, though these remain relatively uncommon.
Regarding GLP-1 medications and lymphoedema, there is currently insufficient evidence to recommend their use specifically for this condition. Whilst weight loss achieved through any means—including GLP-1 receptor agonists in appropriately selected patients—may provide indirect benefits, these medications should only be prescribed according to their licensed indications (type 2 diabetes or obesity meeting specific NICE criteria) and not solely for lymphoedema management. Patients interested in weight loss interventions should discuss options with their GP or lymphoedema specialist to ensure coordinated, safe care that addresses both conditions appropriately.
Frequently Asked Questions
Can GLP-1 medications be prescribed for lymphoedema in the UK?
No, GLP-1 receptor agonists are not licensed or recommended specifically for lymphoedema. They may only be prescribed for type 2 diabetes or weight management in patients meeting NICE criteria, with any lymphoedema benefit being indirect through weight loss.
How does weight loss affect lymphoedema symptoms?
Weight reduction may reduce limb volume, decrease inflammatory mediators, and improve lymphatic vessel function, potentially alleviating lymphoedema symptoms. However, evidence is limited and weight loss should be part of comprehensive lymphoedema management.
What is the standard treatment for lymphoedema in the UK?
Standard treatment includes decongestive lymphatic therapy (manual lymphatic drainage, compression therapy, skin care, and tailored exercise), with specialist NHS services providing individualised care. Weight management may be recommended for patients with obesity.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript