Crohn's disease and Mounjaro represent a complex clinical intersection requiring careful consideration. Crohn's disease is a chronic inflammatory bowel disease causing transmural inflammation throughout the gastrointestinal tract, whilst Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed for type 2 diabetes and weight management. This combination arises when Crohn's patients require weight management or have concurrent diabetes. Given Mounjaro's significant gastrointestinal effects—including nausea, diarrhoea, and delayed gastric emptying—understanding its implications for inflammatory bowel disease is essential. This article examines current evidence, safety considerations, and practical guidance for patients and clinicians navigating this challenging scenario, emphasising individualised risk-benefit assessment and close monitoring.
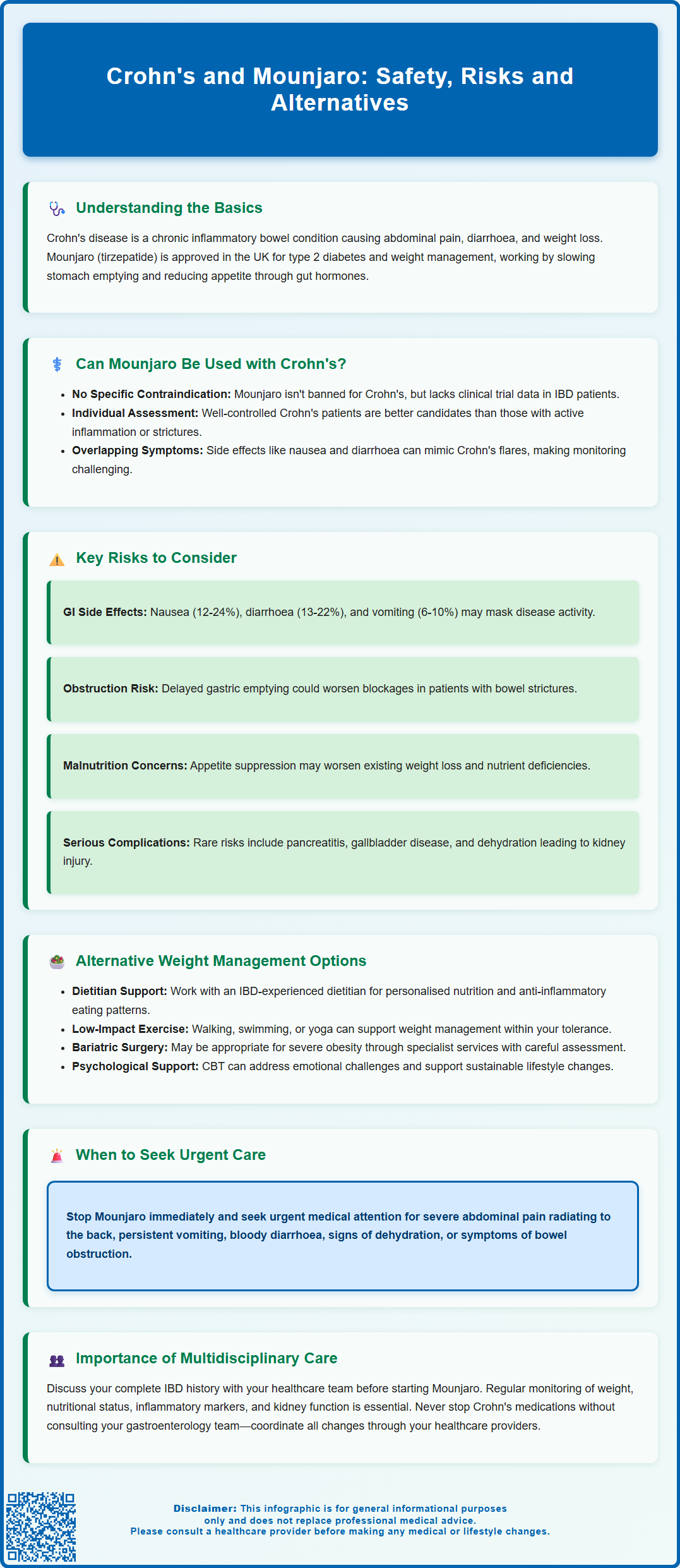
Summary: Mounjaro (tirzepatide) is not specifically contraindicated in Crohn's disease, but requires careful individualised assessment due to overlapping gastrointestinal side effects and limited evidence in inflammatory bowel disease populations.
- Tirzepatide is a dual GIP/GLP-1 receptor agonist licensed for type 2 diabetes and weight management, causing delayed gastric emptying and appetite suppression.
- Common gastrointestinal adverse effects include nausea, diarrhoea, vomiting, and abdominal pain, which may mask or mimic Crohn's disease flares.
- Not recommended in severe gastrointestinal disease or gastroparesis; caution required in patients with strictures or obstructive symptoms.
- Requires close monitoring of disease activity markers, nutritional status, renal function, and coordination between gastroenterology and prescribing teams.
- Alternative weight management options include dietetic support, lifestyle modification, bariatric surgery referral, or other pharmacological agents with established IBD safety profiles.
Table of Contents
Understanding Crohn's Disease and Mounjaro
Crohn's disease is a chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, from the mouth to the anus, though it most commonly involves the terminal ileum and colon. The condition is characterised by transmural inflammation, which can lead to complications including strictures, fistulae, and abscesses. Patients typically experience symptoms such as abdominal pain, diarrhoea (which may be bloody), weight loss, and fatigue. The aetiology involves a complex interplay of genetic susceptibility, environmental factors, and immune dysregulation.
Mounjaro (tirzepatide) is a relatively new medication licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. It is used as an adjunct to a reduced-calorie diet and increased physical activity. Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. It works by enhancing insulin secretion in a glucose-dependent manner, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central mechanisms in the hypothalamus.
The intersection of these two conditions arises primarily when individuals with Crohn's disease seek weight management solutions or have concurrent type 2 diabetes. Given that Mounjaro significantly affects gastrointestinal motility and function, understanding its potential implications for patients with pre-existing inflammatory bowel disease is essential. This article explores the current evidence, safety considerations, and practical guidance for patients and clinicians navigating this clinical scenario. While evidence in Crohn's disease is limited, data from GLP-1 receptor agonists do not show increased IBD flares overall, but careful monitoring is needed. It's important to note that Mounjaro is not recommended during pregnancy or breastfeeding and is not indicated for those under 18 years of age.
Can Mounjaro Be Used in Crohn's Disease?
Currently, there is no specific contraindication to using Mounjaro in patients with Crohn's disease listed in the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA). However, the SmPC does warn that tirzepatide is not recommended in severe gastrointestinal disease, including severe gastroparesis. This is particularly relevant for Crohn's patients with complications such as strictures. Additionally, the clinical trials that led to tirzepatide's approval did not specifically recruit or analyse outcomes in patients with active inflammatory bowel disease, meaning robust evidence for its safety and efficacy in this population is limited.
The decision to prescribe Mounjaro to someone with Crohn's disease must be highly individualised and based on several factors:
-
Disease activity: Patients with well-controlled, quiescent Crohn's disease may be better candidates than those with active inflammation, frequent flares, or complications such as strictures.
-
Gastrointestinal symptoms: Since Mounjaro commonly causes nausea, vomiting, diarrhoea, and abdominal discomfort—symptoms that overlap significantly with Crohn's disease—distinguishing between medication side effects and disease flares could prove challenging.
-
Nutritional status: Many Crohn's patients already struggle with malabsorption and maintaining adequate nutrition. The appetite-suppressing effects of Mounjaro could potentially exacerbate weight loss in those who are already underweight or malnourished.
-
Concurrent medications: Patients with Crohn's disease often take immunosuppressants, biologics, or corticosteroids, and potential drug interactions or cumulative side effects should be considered.
Healthcare professionals should conduct a thorough risk-benefit assessment before initiating Mounjaro in patients with Crohn's disease. Close monitoring during the initial titration phase is essential, with regular review of gastrointestinal symptoms, nutritional parameters, and disease activity markers such as faecal calprotectin or C-reactive protein (CRP). Renal function should be assessed if significant vomiting or diarrhoea occurs, due to the risk of acute kidney injury.
Important additional considerations include:
-
Tirzepatide is typically started at a low dose and gradually increased every 4 weeks to improve gastrointestinal tolerability
-
Women using oral contraceptives should use a non-oral method or add barrier contraception for 4 weeks after starting tirzepatide and after each dose increase, as absorption may be reduced
-
For patients with diabetes using insulin or sulfonylureas, dose reductions of these medications may be needed to prevent hypoglycaemia when starting tirzepatide
Potential Risks and Gastrointestinal Considerations
The primary concern when considering Mounjaro for patients with Crohn's disease relates to its gastrointestinal adverse effect profile. According to the SmPC, the most commonly reported side effects include:
-
Nausea (reported in 12-24% of patients, particularly during dose escalation)
-
Diarrhoea (affecting approximately 13-22% of users)
-
Vomiting (occurring in 6-10% of patients)
-
Abdominal pain and discomfort
-
Constipation (reported in 5-17% of patients)
These side effects are generally more common during dose escalation and may decrease over time.
For individuals with Crohn's disease, these effects could potentially mask or mimic disease flares, making clinical assessment more complex. Distinguishing between medication-related gastrointestinal symptoms and active Crohn's inflammation may require additional investigations, including inflammatory markers, endoscopy, or cross-sectional imaging.
Delayed gastric emptying, a pharmacological effect of GLP-1 receptor agonists, could pose risks in patients with pre-existing gastrointestinal strictures or obstructive symptoms. Slowed transit through narrowed bowel segments might increase the risk of obstruction. While direct evidence with tirzepatide is limited, there have been post-marketing reports of ileus and intestinal obstruction with GLP-1 receptor agonists, warranting caution in patients with known strictures or obstructive symptoms.
There is also consideration regarding pancreatitis risk. GLP-1 receptor agonists have been associated with acute pancreatitis in rare cases. If severe, persistent abdominal pain radiating to the back occurs (possible pancreatitis), tirzepatide should be stopped immediately and urgent medical assessment sought.
Gallbladder disease is another important consideration. GLP-1 receptor agonists and rapid weight loss can both increase the risk of gallstones and other gallbladder problems. Patients should be counselled on symptoms of biliary disease and seek medical advice if these occur.
Dehydration secondary to persistent nausea, vomiting, or diarrhoea represents another important consideration. Severe gastrointestinal adverse effects can lead to acute kidney injury. Patients should be counselled on maintaining adequate fluid intake and recognising signs of dehydration, including reduced urine output, dizziness, or increased thirst. If gastrointestinal symptoms become severe or persistent, patients should contact their healthcare team promptly for assessment, renal function testing, and potential dose adjustment or medication discontinuation.
For patients with diabetes and retinopathy, rapid improvements in blood glucose control with tirzepatide may temporarily worsen diabetic retinopathy, so appropriate monitoring should be considered.
Alternative Weight Management Options for Crohn's Patients
For patients with Crohn's disease who require weight management, several alternative approaches may be more appropriate than Mounjaro, depending on individual circumstances:
Lifestyle modifications remain the cornerstone of weight management and should be tailored to accommodate the specific challenges of Crohn's disease. Working with a registered dietitian experienced in inflammatory bowel disease is invaluable. Dietary strategies might include:
-
Identifying and avoiding personal trigger foods that exacerbate symptoms
-
Ensuring adequate protein and micronutrient intake, particularly during active disease
-
Implementing portion control strategies that don't compromise nutritional status
-
Considering anti-inflammatory dietary patterns, though evidence for specific diets in Crohn's disease remains evolving
Physical activity should be encouraged within individual tolerance levels. Regular exercise can support weight management, improve bone health (important given corticosteroid use in many Crohn's patients), and enhance overall wellbeing. Low-impact activities such as walking, swimming, or yoga may be particularly suitable during periods of active disease.
Bariatric surgery is an important option for people with severe obesity (BMI ≥40 kg/m², or ≥35 kg/m² with obesity-related conditions) in line with NICE guidance. Referral would typically be via specialist weight management services (Tier 3/4). The suitability of different surgical procedures should be carefully assessed in Crohn's patients, considering disease location and activity.
Alternative pharmacological options for weight management include:
-
Orlistat: A lipase inhibitor that reduces fat absorption. However, it is contraindicated in chronic malabsorption syndrome (relevant to some Crohn's patients) and commonly causes gastrointestinal side effects including oily stools and faecal urgency. It may also reduce absorption of fat-soluble vitamins, which could worsen nutritional deficiencies.
-
Naltrexone-bupropion combination: This acts centrally to reduce appetite but has limited evidence in IBD populations. It is contraindicated in uncontrolled hypertension and carries seizure risk. Availability varies across NHS regions.
-
Other GLP-1 receptor agonists (e.g., semaglutide, liraglutide) may have similar gastrointestinal adverse effects to tirzepatide and require the same cautions in Crohn's disease.
Psychological support addressing the emotional aspects of living with chronic illness and weight management can be beneficial. Cognitive behavioural therapy (CBT) or other psychological interventions may help patients develop sustainable lifestyle changes.
For patients with Crohn's disease and concurrent type 2 diabetes requiring glucose control, metformin remains first-line therapy and has a more established safety profile in IBD populations, though gastrointestinal side effects can still occur. NICE guidance on type 2 diabetes management should be followed, with specialist input when managing complex cases involving inflammatory bowel disease.
When to Consult Your Healthcare Team
Patients with Crohn's disease considering Mounjaro, or those already taking it, should maintain close communication with their healthcare team. This typically includes both the gastroenterology team managing their IBD and the prescriber of Mounjaro (whether a GP, diabetologist, or weight management specialist).
Before starting Mounjaro, patients should discuss:
-
Current Crohn's disease activity and recent flare history
-
Existing gastrointestinal symptoms and their severity
-
Nutritional status and any history of malabsorption
-
All current medications, including immunosuppressants and biologics
-
Previous complications such as strictures, fistulae, or surgeries
-
Pregnancy intentions or breastfeeding status (tirzepatide is not recommended during pregnancy or breastfeeding)
Seek urgent medical advice if you experience:
-
Severe or persistent abdominal pain, particularly if different from usual Crohn's symptoms
-
Severe, persistent abdominal pain radiating to the back – stop tirzepatide immediately (possible pancreatitis)
-
Bloody diarrhoea or significant increase in stool frequency
-
Persistent vomiting preventing adequate fluid or medication intake
-
Signs of dehydration: reduced urination, dizziness, confusion, or extreme thirst
-
Symptoms suggesting bowel obstruction: severe cramping pain, abdominal distension, inability to pass stool or wind
-
Unexplained fever or signs of infection
-
Signs of severe allergic reaction (e.g., swelling of face/lips/tongue, breathing difficulty) – call emergency services
-
Symptoms of hypoglycaemia (if taking insulin or sulfonylureas): sweating, shakiness, confusion, irritability
Routine monitoring should include regular assessment of:
-
Weight trends and nutritional parameters
-
Gastrointestinal symptom patterns
-
Inflammatory markers (CRP, faecal calprotectin) as clinically indicated
-
Blood glucose levels (if diabetic)
-
Medication adherence and tolerability
-
Renal function if experiencing significant gastrointestinal side effects
Patients should never stop Crohn's disease medications without consulting their gastroenterology team, even if experiencing side effects from Mounjaro. Similarly, any decision to discontinue or adjust Mounjaro should be made in consultation with the prescribing clinician. A multidisciplinary approach involving gastroenterology, diabetes/weight management services, dietetics, and primary care ensures comprehensive, coordinated care that addresses both conditions safely and effectively.
If you experience any suspected side effects from Mounjaro, these can be reported through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Is Mounjaro safe for people with Crohn's disease?
Mounjaro is not specifically contraindicated in Crohn's disease, but requires careful individualised assessment. It is not recommended in severe gastrointestinal disease, and patients with active inflammation, strictures, or complications may face increased risks from its gastrointestinal side effects.
What are the main risks of using Mounjaro with Crohn's disease?
The primary risks include gastrointestinal side effects (nausea, diarrhoea, vomiting) that may mask Crohn's flares, delayed gastric emptying potentially worsening strictures, dehydration leading to acute kidney injury, and appetite suppression that could worsen malnutrition in already underweight patients.
What alternatives to Mounjaro exist for weight management in Crohn's patients?
Alternatives include specialist dietetic support tailored to inflammatory bowel disease, structured lifestyle modification programmes, bariatric surgery referral for severe obesity (following NICE guidance), and other pharmacological options such as orlistat, though each requires careful assessment for suitability in Crohn's disease.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












