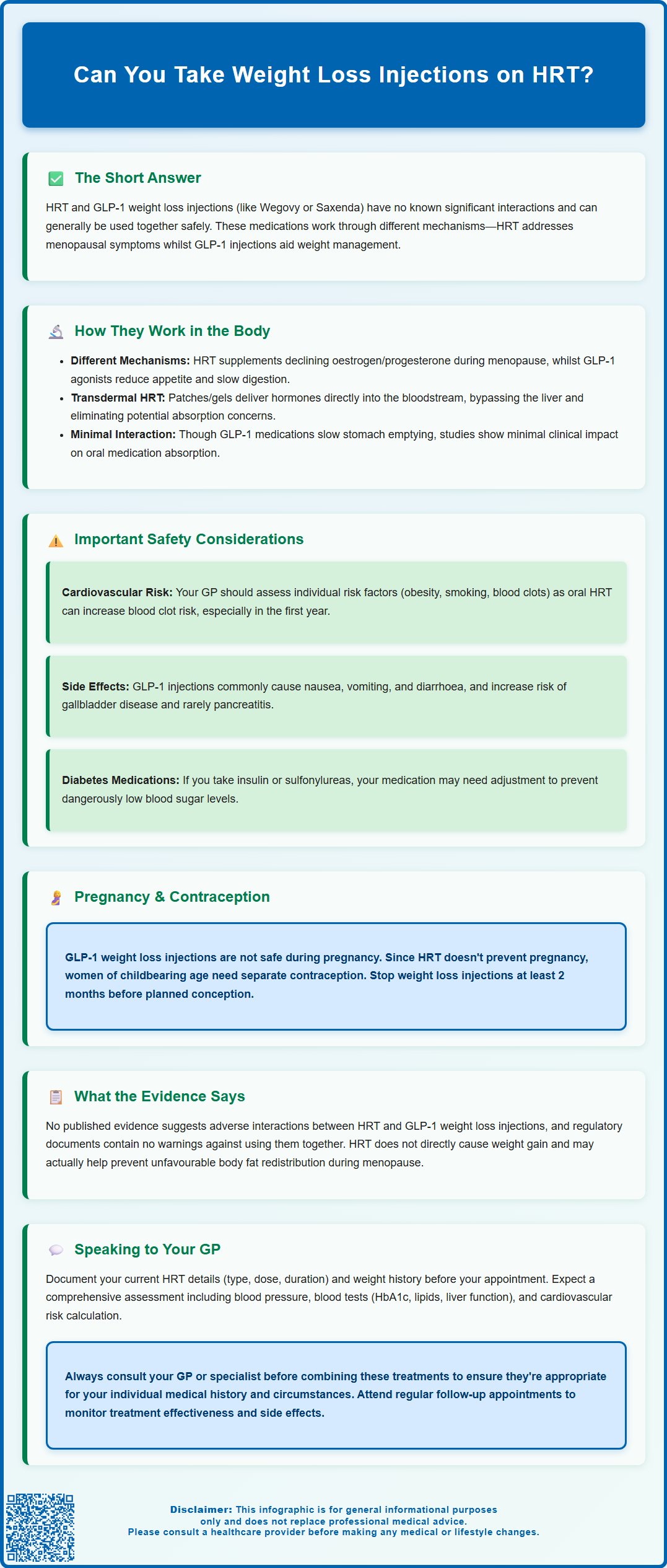
Many women managing menopause with hormone replacement therapy (HRT) also seek support for weight management. If you're considering weight loss injections whilst taking HRT, you may wonder whether these treatments can be safely combined. There is no known clinically significant interaction between HRT and GLP-1 weight loss injections such as semaglutide (Wegovy) or liraglutide (Saxenda). These medications work through different mechanisms and are not listed as contraindications in UK product information. However, individual circumstances vary, and the decision to combine these therapies should always be made in consultation with your GP, who can assess your complete medical history and individual risk factors.
Summary: There is no known clinically significant interaction between HRT and GLP-1 weight loss injections, and their concurrent use is not contraindicated in UK product information.
- GLP-1 receptor agonists (semaglutide, liraglutide) and HRT work through different mechanisms and do not compete for the same receptors or metabolic pathways.
- Cardiovascular risk assessment is important as oral HRT can slightly increase VTE risk, whilst some GLP-1 agents have shown cardiovascular benefits in clinical trials.
- Common GLP-1 side effects include gastrointestinal symptoms and increased risk of gallbladder disease; severe abdominal pain requires urgent medical attention.
- Women with an intact uterus require progestogen with oestrogen HRT, and effective contraception is essential as GLP-1 injections are contraindicated in pregnancy.
- NICE guidance supports individualised treatment approaches and does not contraindicate weight management medications alongside HRT.
- Regular GP monitoring is essential to assess treatment effectiveness, manage side effects, and adjust medications as needed.
Table of Contents
- Can You Take Weight Loss Injections on HRT?
- How HRT and Weight Loss Injections Work in the Body
- Safety Considerations When Combining HRT and Weight Loss Injections
- What the Evidence Says About Using Both Treatments Together
- Speaking to Your GP About Weight Loss Injections While on HRT
- Frequently Asked Questions
Can You Take Weight Loss Injections on HRT?
Many women approaching or experiencing menopause find themselves managing multiple health concerns simultaneously, including menopausal symptoms and weight management. If you're currently taking hormone replacement therapy (HRT) and considering weight loss injections, you may wonder whether these treatments can be safely combined.
There is no known clinically significant interaction between HRT and GLP-1 weight loss injections, and their concurrent use is not listed as a contraindication in UK product information. These medications work through different mechanisms in the body and generally do not interact in ways that would make their combination unsafe. However, as with any medical treatment, individual circumstances vary considerably, and what is appropriate for one person may not be suitable for another.
Weight loss injections, primarily GLP-1 receptor agonists such as semaglutide (Wegovy) or liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. Similarly, HRT remains the most effective treatment for menopausal symptoms and is available in various formulations including tablets, patches, gels, and implants. Both treatments are prescribed for distinct clinical indications, and require individual assessment.
Importantly, women with an intact uterus require a progestogen component with oestrogen HRT to protect the lining of the womb. Additionally, GLP-1 weight loss injections are contraindicated in pregnancy, and HRT is not a form of contraception. If you are of childbearing potential, you should use effective contraception while taking these medications.
The decision to combine these therapies should always be made in consultation with your GP or specialist, who can assess your complete medical history, current medications, and individual risk factors. This personalised approach ensures that both treatments are appropriate for your specific circumstances and that you receive proper monitoring throughout your treatment journey.
How HRT and Weight Loss Injections Work in the Body
Understanding how these medications function helps clarify why they can typically be used together without direct pharmaceutical interaction.
Hormone Replacement Therapy (HRT) works by supplementing the declining levels of oestrogen (and sometimes progesterone) that occur during perimenopause and menopause. Oestrogen receptors are found throughout the body, and HRT helps alleviate symptoms such as hot flushes, night sweats, mood changes, and vaginal dryness. Different HRT formulations deliver hormones through various routes—oral tablets are metabolised through the liver, whilst transdermal preparations (patches and gels) deliver hormones directly into the bloodstream, bypassing first-pass hepatic metabolism. This distinction can be clinically significant for women with certain risk factors.
Weight loss injections, specifically GLP-1 receptor agonists, work by mimicking the action of glucagon-like peptide-1, a naturally occurring hormone produced in the intestine. These medications slow gastric emptying, reduce appetite, and enhance feelings of satiety after eating. They also improve insulin sensitivity and glucose metabolism. The injections are administered subcutaneously, typically once weekly (semaglutide) or once daily (liraglutide), and work primarily through the gastrointestinal system and central nervous system appetite centres. GLP-1 receptor agonists can also cause small average increases in heart rate.
Because HRT primarily affects hormone receptors throughout the body whilst weight loss injections target appetite regulation and glucose metabolism, their mechanisms of action are fundamentally different. This pharmacological separation means they do not compete for the same receptors or metabolic pathways, reducing the likelihood of direct drug-drug interactions.
However, the delayed gastric emptying caused by GLP-1 receptor agonists could theoretically affect the absorption of oral medications, including oral HRT. Most studies show no clinically relevant effect on many oral medicines, but monitoring is prudent if you experience significant gastrointestinal symptoms. Transdermal HRT formulations bypass the digestive system entirely, eliminating this concern.
Safety Considerations When Combining HRT and Weight Loss Injections
Whilst there is no direct contraindication to using HRT and weight loss injections together, several important safety considerations warrant careful evaluation by your healthcare provider.
Cardiovascular risk assessment is particularly important when considering both treatments. HRT, especially oral oestrogen, can slightly increase the risk of venous thromboembolism (blood clots), particularly in the first year of use and in women with additional risk factors such as obesity, smoking, or thrombophilia. Transdermal HRT is preferred for women with higher VTE risk factors. Some GLP-1 receptor agonists have shown cardiovascular benefits in clinical trials, particularly semaglutide in the SELECT trial, though these benefits are not established for all agents or doses used for obesity. Your GP will assess your individual cardiovascular risk profile, considering factors such as age, BMI, blood pressure, and family history.
Gastrointestinal and gallbladder effects are common with GLP-1 receptor agonists. Nausea, vomiting, diarrhoea, and constipation typically occur when starting treatment or increasing doses. These medications also increase the risk of gallbladder disease (cholelithiasis/cholecystitis) and, rarely, pancreatitis. If you experience severe upper abdominal pain (with or without vomiting, fever or jaundice), seek urgent medical care. If you're taking oral HRT, significant gastrointestinal symptoms could potentially affect absorption, though this is rarely clinically significant.
Metabolic monitoring becomes important when using both treatments. Weight loss injections can affect blood glucose levels, which is beneficial for those with type 2 diabetes or prediabetes. If you have diabetes and take insulin or sulfonylureas, your medication may need adjustment to prevent hypoglycaemia. There is also a small risk of temporary worsening of diabetic retinopathy in people with diabetes who experience rapid improvement in blood glucose levels. HRT can also influence insulin sensitivity and glucose metabolism, though effects vary between individuals.
Individual risk factors such as personal or family history of breast cancer, endometrial cancer, liver disease, or pancreatitis require careful consideration. Your GP will review your complete medical history to ensure both treatments are appropriate for your circumstances.
What the Evidence Says About Using Both Treatments Together
The scientific literature specifically examining the concurrent use of HRT and weight loss injections remains limited, as these combinations have not been extensively studied in dedicated clinical trials. However, we can draw upon broader evidence regarding each treatment individually and their known effects on overlapping health parameters.
There is no published evidence suggesting that HRT and GLP-1 receptor agonists interact adversely when used together. The product information for these medications does not list specific contraindications for their concurrent use, though direct studies of the combination are limited. The absence of interaction warnings in regulatory documents suggests that no clinically significant issues have been identified through pharmacovigilance.
Weight management during menopause is a common concern, as hormonal changes can contribute to increased abdominal adiposity and metabolic changes. Some women report weight gain when starting HRT, though evidence suggests HRT does not directly cause weight gain and may actually help prevent the unfavourable redistribution of body fat associated with menopause. The addition of weight loss injections may help address weight concerns whilst allowing women to continue benefiting from HRT for menopausal symptom management.
NICE guidance on menopause (NG23) emphasises individualised treatment approaches and does not contraindicate the use of weight management medications alongside HRT. For weight loss medications, NICE technology appraisals TA875 (semaglutide) and TA664 (liraglutide) provide specific eligibility criteria for NHS treatment in England. These typically involve initiation in specialist weight management services, with stricter criteria than in some other countries. Treatment is usually time-limited, and lower BMI thresholds may apply for some minority ethnic groups.
The MHRA's Yellow Card scheme continues to monitor for any emerging safety signals, and patients are encouraged to report suspected side effects from any medication.
Speaking to Your GP About Weight Loss Injections While on HRT
If you're considering adding weight loss injections to your existing HRT regimen, or vice versa, a thorough discussion with your GP is essential to ensure safe and appropriate treatment.
Prepare for your appointment by documenting your current HRT formulation (type, dose, and route of administration), how long you've been taking it, and how well it's controlling your menopausal symptoms. Keep a record of your weight history, previous weight management attempts, and any weight-related health conditions such as type 2 diabetes, hypertension, or sleep apnoea. This information helps your GP assess whether weight loss injections are clinically appropriate.
Key topics to discuss include:
-
Your eligibility for weight loss injections based on NICE criteria
-
Whether referral to a specialist Tier 3 weight management service is required
-
Your complete medical history, including cardiovascular risk factors
-
Current medications and any previous adverse reactions
-
Realistic expectations about weight loss and timeframes
-
Potential side effects of weight loss injections and how to manage them
-
Monitoring requirements, including blood tests and follow-up appointments
-
Whether your HRT formulation might need adjustment
-
Contraception if you are of childbearing potential (GLP-1 RAs are contraindicated in pregnancy and should be stopped at least 2 months before planned pregnancy)
-
Cost considerations, as weight loss injections may not always be available on the NHS
Be prepared for your GP to conduct a comprehensive assessment, which may include blood pressure measurement, blood tests (including HbA1c, lipid profile, and liver function), and calculation of your cardiovascular risk score. They may also discuss lifestyle modifications, as diet and exercise remain fundamental to successful weight management alongside any pharmacological treatment.
If your GP prescribes weight loss injections, ensure you understand the injection technique, dose escalation schedule, and when to seek medical advice. Contact your GP promptly if you experience severe abdominal pain, persistent vomiting, right upper abdominal pain, fever, jaundice, or any concerning symptoms. If you have diabetes, agree on a plan to monitor and adjust your diabetes medications if needed to prevent hypoglycaemia.
Regular follow-up appointments allow monitoring of treatment effectiveness, side effects, and any necessary adjustments to either your HRT or weight loss medication. Report any suspected side effects via the MHRA Yellow Card scheme. This collaborative approach ensures you receive safe, effective, and personalised care throughout your treatment journey.
Frequently Asked Questions
Do weight loss injections interact with HRT?
There is no known clinically significant interaction between HRT and GLP-1 weight loss injections. These medications work through different mechanisms and are not listed as contraindications in UK product information, though individual assessment by your GP is essential.
Should I use transdermal or oral HRT with weight loss injections?
Transdermal HRT (patches or gels) bypasses the digestive system entirely, eliminating any theoretical concerns about absorption affected by delayed gastric emptying from GLP-1 injections. Your GP can advise on the most appropriate HRT formulation based on your individual risk factors.
What should I monitor when taking both HRT and weight loss injections?
Regular monitoring should include cardiovascular risk factors, gastrointestinal symptoms, blood glucose levels (especially if diabetic), and treatment effectiveness. Contact your GP promptly if you experience severe abdominal pain, persistent vomiting, or any concerning symptoms.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript