Can you take Saxenda with antidepressants? Many patients in the UK require both weight management support and treatment for depression or anxiety, raising important questions about medication compatibility. Saxenda (liraglutide 3.0 mg), a GLP-1 receptor agonist licensed for weight management, is not contraindicated with antidepressants, and concurrent use is common in clinical practice. However, individual patient factors, the specific antidepressant prescribed, and potential additive side effects require careful consideration. This article examines the safety, monitoring requirements, and practical considerations for patients using Saxenda alongside antidepressant therapy, providing evidence-based guidance aligned with UK clinical standards.
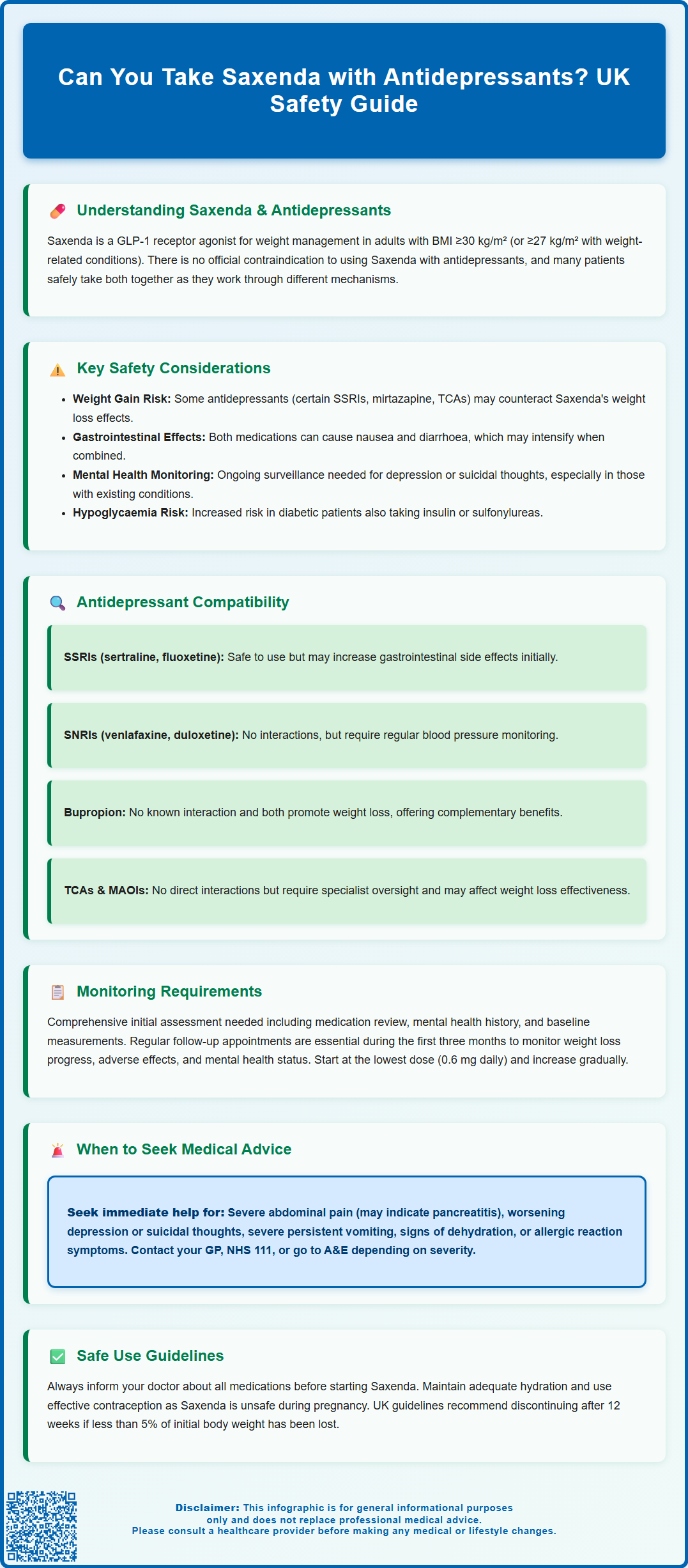
Summary: Saxenda can be taken with antidepressants as there is no official contraindication, and many patients use both medications safely together under appropriate medical supervision.
- Saxenda is a GLP-1 receptor agonist that regulates appetite through different pathways than antidepressants, which modulate neurotransmitter systems.
- No pharmacokinetic interactions exist between Saxenda and commonly prescribed antidepressants such as SSRIs, SNRIs, or TCAs.
- Both medication types may cause gastrointestinal side effects, potentially leading to additive nausea or diarrhoea during treatment initiation.
- Patients require ongoing monitoring for mental health status, gastrointestinal symptoms, weight changes, and cardiovascular parameters.
- All medications should be disclosed to prescribing clinicians before starting Saxenda to ensure individualised assessment and safe treatment planning.
- Treatment should follow NICE TA664 guidance and be discontinued after 12 weeks if less than 5% initial body weight is lost.
Table of Contents
Understanding Saxenda and Antidepressant Interactions
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK as an adjunct to reduced-calorie diet and increased physical activity for weight management in adults with a BMI ≥30 kg/m², or ≥27-<30 kg/m² with at least one weight-related comorbidity. It works by mimicking the action of the naturally occurring hormone GLP-1, which regulates appetite and food intake by acting on areas of the brain involved in appetite regulation. Saxenda slows gastric emptying, increases feelings of fullness, and reduces hunger, thereby supporting calorie reduction.
Antidepressants encompass several drug classes used to treat depression, anxiety disorders, and other mental health conditions. These include selective serotonin reuptake inhibitors (SSRIs), serotonin-noradrenaline reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs), among others. Each class works through different mechanisms affecting neurotransmitter levels in the brain.
There is no official contraindication to using Saxenda alongside antidepressants, and many patients successfully use both medication types concurrently. The pharmacological mechanisms of Saxenda and most antidepressants operate through different pathways—Saxenda primarily affects metabolic and appetite regulation via GLP-1 receptors, whilst antidepressants modulate neurotransmitter systems. However, as with any medication combination, individual patient factors, existing health conditions, and the specific antidepressant prescribed must be considered.
It is essential that patients inform their prescribing clinician about all medications they are taking, including antidepressants, before starting Saxenda. This allows for appropriate assessment of potential interactions, monitoring requirements, and individualised treatment planning to ensure both safety and therapeutic effectiveness. Note that Saxenda's delayed gastric emptying effect may potentially affect the absorption of some oral medicines, though this is usually not clinically significant.
In the UK, Saxenda should be initiated and monitored in line with NICE TA664, typically within specialist weight management services. Treatment should be discontinued after 12 weeks on the 3 mg daily dose if less than 5% of initial body weight has been lost.
Safety Considerations When Combining Saxenda with Antidepressants
When considering the combination of Saxenda with antidepressants, several safety considerations warrant attention. Weight changes represent a key consideration, as some antidepressants—particularly certain SSRIs, mirtazapine, and TCAs—are associated with weight gain, which may counteract Saxenda's weight management effects. Conversely, other antidepressants may promote weight loss.
Gastrointestinal side effects are common with Saxenda, particularly during treatment initiation and dose escalation. The most frequently reported adverse effects include nausea, vomiting, diarrhoea, and constipation. Some antidepressants, especially SSRIs and SNRIs, can also cause gastrointestinal disturbances. When used together, there may be an additive effect on gastrointestinal symptoms, though this does not constitute a formal drug interaction. Patients should be counselled about these potential effects and advised on management strategies, such as taking oral antidepressants with food where appropriate (note that Saxenda is administered as a subcutaneous injection and is not related to meal timing).
Mental health monitoring remains important for all patients taking antidepressants. Saxenda's prescribing information notes that patients should be monitored for signs of depression or suicidal thoughts, particularly those with a history of depression. Whilst there is no established causal link between Saxenda and worsening depression, weight management interventions can affect mood and self-perception. Patients with existing mental health conditions require ongoing psychiatric review to ensure their antidepressant therapy remains optimised.
Hypoglycaemia risk should be considered in patients taking antidepressants alongside Saxenda, particularly if they also have type 2 diabetes and use insulin or sulfonylureas. Whilst Saxenda itself has a low intrinsic risk of hypoglycaemia, some antidepressants may alter glucose control; monitoring is advised if on diabetes medicines.
Additional safety considerations include monitoring for symptoms of gallbladder disease (cholelithiasis/cholecystitis), small increases in heart rate, and maintaining adequate hydration to reduce the risk of renal impairment during significant gastrointestinal adverse effects. Women of childbearing potential should use effective contraception during treatment, as Saxenda should not be used during pregnancy.
Specific Antidepressant Classes and Saxenda Compatibility
Selective serotonin reuptake inhibitors (SSRIs) such as sertraline, fluoxetine, citalopram, and escitalopram are the most commonly prescribed antidepressants in the UK. There are no known pharmacokinetic interactions between SSRIs and Saxenda, and concurrent use is generally considered safe. Both medication types can cause gastrointestinal side effects, so patients may experience increased nausea or diarrhoea, particularly when initiating treatment. These effects typically diminish over time as tolerance develops. Caution regarding hyponatraemia risk with SSRIs is warranted, especially in the context of vomiting or dehydration; monitoring may be advisable in higher-risk groups such as older adults.
Serotonin-noradrenaline reuptake inhibitors (SNRIs) including venlafaxine and duloxetine similarly have no documented interactions with Saxenda. SNRIs may affect appetite and cause nausea; clinical impact on weight with Saxenda varies between individuals. Some SNRIs are associated with modest increases in blood pressure, so patients using both medications should have their blood pressure and pulse monitored regularly as part of routine care.
Tricyclic antidepressants (TCAs) such as amitriptyline are older antidepressants often associated with weight gain and increased appetite. Whilst there is no pharmacological interaction with Saxenda, the opposing effects on weight may reduce the overall effectiveness of weight management efforts. TCAs can also cause constipation, which may be exacerbated or counteracted by Saxenda's gastrointestinal effects.
Monoamine oxidase inhibitors (MAOIs) like phenelzine are rarely prescribed but require careful consideration. Whilst there is no direct interaction with Saxenda, MAOIs have numerous dietary and drug restrictions and may alter glucose control. Patients taking MAOIs require specialist psychiatric care and should have any new medication, including Saxenda, reviewed by both their psychiatrist and prescribing clinician.
Bupropion is licensed in the UK for smoking cessation (not for depression). It has no known interaction with Saxenda. Both medications may contribute to weight loss, potentially offering complementary benefits for weight management, though any use of bupropion as an antidepressant would be off-label in the UK.
Monitoring and Medical Supervision Requirements
Patients using Saxenda alongside antidepressants require appropriate medical supervision to ensure safety and treatment effectiveness. Initial assessment should include a comprehensive medication review, documentation of mental health history, current psychiatric stability, and identification of any previous adverse reactions to either medication class. Baseline measurements should include weight, body mass index (BMI), blood pressure, pulse, and relevant metabolic parameters.
Regular follow-up appointments are essential, particularly during the first three months of Saxenda treatment. Patients should follow local specialist weight management pathways and SmPC review criteria. These appointments provide opportunities to assess weight loss progress, monitor for adverse effects, evaluate mental health status, and adjust treatment as needed. Patients should be asked specifically about mood changes, gastrointestinal symptoms, and any concerns about their medications.
Mental health monitoring should continue as per existing care plans for patients taking antidepressants. Any significant mood changes, emergence of suicidal thoughts, or worsening of depression or anxiety should prompt immediate clinical review. Whilst there is no established link between Saxenda and psychiatric adverse effects in patients with stable mental health conditions, vigilance remains appropriate.
Gastrointestinal symptom management may require additional support. Patients should be advised to start Saxenda at the lowest dose (0.6 mg daily) and increase gradually as tolerated, following the licensed titration schedule. If nausea or vomiting becomes problematic, dose escalation can be delayed. Persistent or severe gastrointestinal symptoms warrant medical review to exclude other causes and consider whether treatment continuation is appropriate.
Diabetes monitoring is crucial for patients with type 2 diabetes taking Saxenda with antidepressants. Weight loss and Saxenda's glucose-lowering effects may necessitate reduction in other diabetes medications, particularly insulin or sulfonylureas, to prevent hypoglycaemia.
Additional monitoring should include pulse and blood pressure, vigilance for biliary symptoms, and review of renal function if significant gastrointestinal adverse effects occur. Treatment should be discontinued after 12 weeks on the 3 mg daily dose if less than 5% of initial body weight has been lost. Women should use effective contraception during treatment and stop Saxenda if pregnancy occurs.
When to Seek Medical Advice
Patients taking Saxenda with antidepressants should be aware of specific circumstances requiring prompt medical attention. Immediate medical advice should be sought if experiencing severe, persistent abdominal pain, particularly if radiating to the back, as this may indicate pancreatitis—a rare but serious potential adverse effect of Saxenda. Other symptoms of pancreatitis include persistent nausea, vomiting, and fever. Patients should stop Saxenda and contact their GP or attend A&E if these symptoms occur.
Gallbladder problems require urgent attention. Seek immediate medical advice for sudden or persistent right upper abdominal pain, fever, or jaundice (yellowing of the skin or whites of the eyes), which may indicate gallbladder disease.
Mental health deterioration requires urgent review. Patients should contact their GP or mental health team promptly if they experience worsening depression, emergence of suicidal thoughts, severe anxiety, or any significant change in mood or behaviour. Whilst there is no established causal relationship between Saxenda and psychiatric symptoms in patients with stable mental health, any concerning changes warrant professional assessment. In crisis situations, patients should contact NHS 111, their crisis team, or attend A&E.
Severe gastrointestinal symptoms that persist beyond the initial adjustment period or significantly impact daily functioning should be discussed with a healthcare professional. Whilst mild nausea is common and usually improves, severe or persistent vomiting can lead to dehydration and may indicate that Saxenda is not suitable. Patients should seek advice if they cannot tolerate oral fluids, experience signs of dehydration (dark urine, dizziness, reduced urination), or have concerns about symptom severity.
Cardiovascular symptoms such as sustained palpitations or a marked increase in resting heart rate should prompt medical review. Allergic reactions, though rare, require immediate attention. Symptoms such as rash, itching, swelling of the face or throat, difficulty breathing, or rapid heartbeat should prompt emergency medical attention. Patients with diabetes should also seek advice if experiencing recurrent hypoglycaemia (blood glucose below 4 mmol/L), as medication adjustments may be necessary.
Routine concerns about medication effectiveness, side effects, or questions about continuing treatment should be discussed at scheduled follow-up appointments or by contacting the prescribing clinician's practice for advice. Patients are encouraged to report any suspected side effects to the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Frequently Asked Questions
Are there any dangerous interactions between Saxenda and SSRIs?
No, there are no known pharmacokinetic interactions between Saxenda and SSRIs such as sertraline, fluoxetine, or citalopram. Both medications can cause gastrointestinal side effects, so patients may experience increased nausea initially, but concurrent use is generally considered safe under medical supervision.
Will antidepressants affect Saxenda's weight loss effectiveness?
Some antidepressants, particularly certain SSRIs, mirtazapine, and tricyclic antidepressants, are associated with weight gain and may counteract Saxenda's weight management effects. Individual responses vary, and treatment effectiveness should be monitored through regular follow-up appointments with weight assessments.
Do I need special monitoring if taking Saxenda with antidepressants?
Yes, patients require regular monitoring including mental health status, gastrointestinal symptoms, weight progress, blood pressure, and pulse. Follow-up appointments are particularly important during the first three months, and any significant mood changes or concerning symptoms should prompt immediate clinical review.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










