Can Saxenda stop working over time? Many patients using Saxenda (liraglutide 3.0 mg) for weight management experience a plateau or reduced effectiveness after initial success. This phenomenon may result from physiological adaptation as your metabolism adjusts to a lower body weight, behavioural changes affecting diet and activity levels, or treatment fatigue. Understanding why Saxenda's effects may diminish, recognising the signs of reduced efficacy, and knowing when to seek clinical review are essential for optimising your weight management journey. This article explores the mechanisms behind treatment plateaus, practical steps to take if Saxenda stops working, and alternative options available through the NHS.
Summary: Saxenda can appear to stop working due to metabolic adaptation, behavioural changes, or treatment fatigue, though it may still be pharmacologically active.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed by the MHRA for weight management in adults with obesity or overweight with comorbidities.
- Weight loss plateaus often result from reduced basal metabolic rate after weight loss, decreased adherence to lifestyle measures, or treatment fatigue rather than true medication failure.
- NICE guidance recommends discontinuing Saxenda if patients do not achieve at least 5% weight loss after 12 weeks at the full 3.0 mg daily maintenance dose.
- Signs of reduced efficacy include weight plateau or regain, return of appetite, reduced satiety, and increased snacking despite consistent dosing.
- Clinical review should assess adherence, injection technique, storage conditions, lifestyle factors, and potential medical causes before considering treatment changes.
- Alternatives include Wegovy (semaglutide 2.4 mg weekly), orlistat, bariatric surgery for eligible patients, and specialist weight management services with behavioural support.
Table of Contents
Can Saxenda Stop Working Over Time?
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for weight management in adults with obesity or overweight with weight-related comorbidities, and in certain adolescents. While Saxenda can be effective for weight loss, some patients report that its effects diminish over time—a phenomenon sometimes referred to as a weight loss plateau.
Several mechanisms may explain why Saxenda appears to become less effective. Physiological adaptation is one key factor: as you lose weight, your basal metabolic rate naturally declines, meaning fewer calories are required to maintain your new body weight. This can slow further weight loss even when the medication continues to work at a pharmacological level.
Behavioural factors also play a significant role. Initial dietary and lifestyle changes may become less stringent over time, leading to increased calorie intake or reduced physical activity. Additionally, some patients may experience treatment fatigue, where adherence to daily injections or accompanying lifestyle modifications wanes after several months.
It is important to note that NICE guidance (TA664) recommends discontinuing Saxenda if patients do not achieve at least 5% weight loss after 12 weeks at the full maintenance dose (3.0 mg daily). This criterion, which aligns with the SmPC, helps identify non-responders early when the medication is used within specialist weight management services. However, for those who initially respond well, a subsequent plateau does not necessarily mean the medication has completely stopped working—it may simply indicate that additional strategies are needed to continue progress.
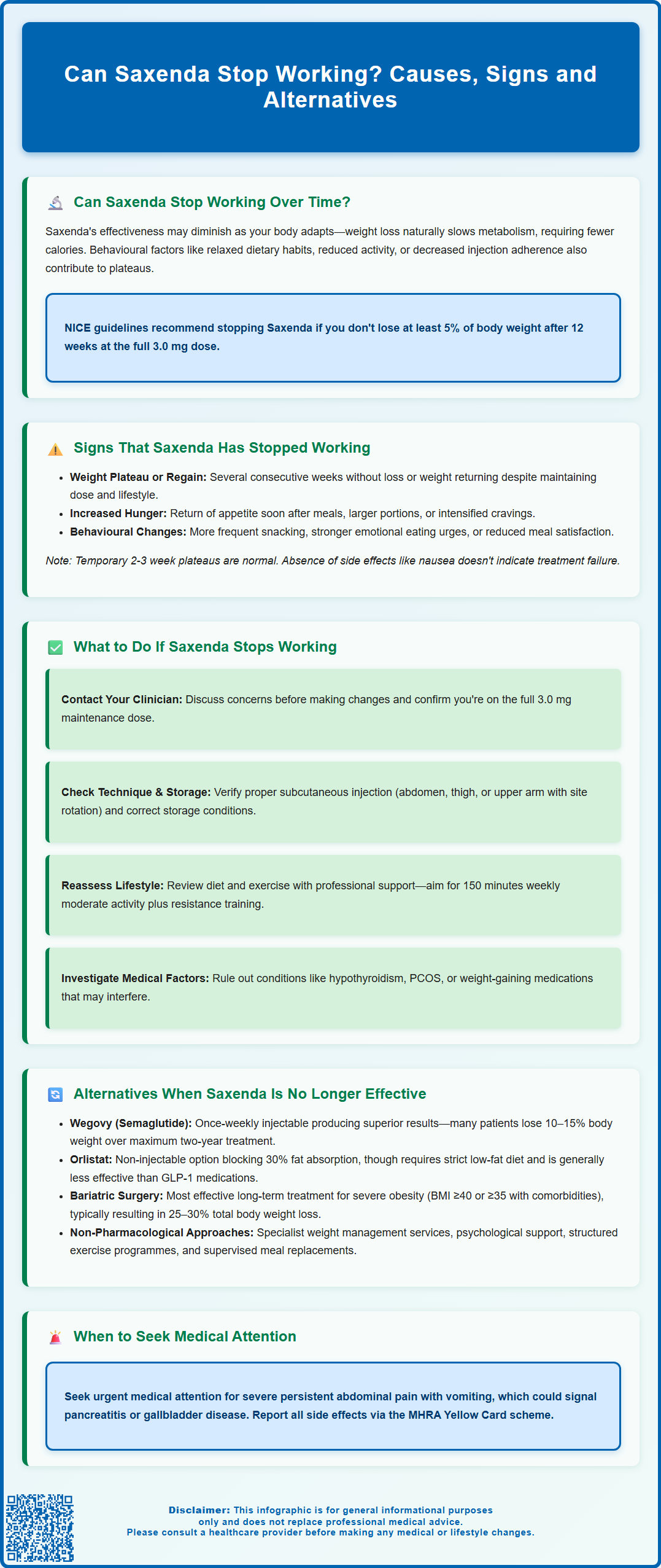
Signs That Saxenda Has Stopped Working
Recognising when Saxenda may no longer be effective is important for timely clinical review and potential treatment adjustment. Weight plateau or regain is the most obvious indicator. If you have stopped losing weight for several consecutive weeks despite maintaining your prescribed dose and lifestyle measures, or if you begin to regain weight, this may suggest reduced efficacy.
Return of appetite and reduced satiety are key subjective signs. Saxenda works primarily by acting on brain receptors to reduce appetite and energy intake, with additional effects on gastric emptying (particularly early in treatment). If you notice that hunger returns more quickly after meals, portion sizes increase, or cravings intensify despite consistent dosing, the medication's appetite-regulating effects may have diminished.
Changes in eating behaviour can also signal reduced effectiveness. Patients may find themselves snacking more frequently, experiencing stronger urges to eat in response to emotional triggers, or feeling less satisfied after meals. These behavioural changes often precede measurable weight regain.
It is essential to distinguish between a true treatment failure and normal weight loss patterns. Weight loss is rarely linear—temporary plateaus lasting 2–3 weeks are common and do not necessarily indicate treatment failure. However, if multiple signs occur together, particularly weight regain alongside increased appetite, clinical review is warranted.
Importantly, the presence or absence of side effects is not a reliable indicator of whether Saxenda is working. Many patients continue to benefit from the medication even after initial side effects like nausea have subsided.
What to Do If Saxenda Stops Working
If you suspect Saxenda has stopped working, the first step is to contact your prescribing clinician or GP for a comprehensive review. Discuss your concerns before making any changes to your treatment, as stopping the medication may lead to weight regain. Your healthcare provider will assess whether you are receiving the full maintenance dose (3.0 mg daily), as inadequate dosing can mimic treatment failure.
Review adherence and injection technique. Ensure you are administering Saxenda correctly—subcutaneously into the abdomen, thigh, or upper arm—and rotating injection sites to prevent lipohypertrophy, which can impair absorption. Check that the medication has been stored properly (refrigerated before first use, then below 30°C for up to one month after first use; do not freeze; protect from light) and has not expired.
Reassess lifestyle factors thoroughly. Even with medication, weight management requires sustained dietary modification and physical activity. Consider consulting a dietitian to review your eating patterns, portion sizes, and overall calorie intake. The NHS recommends at least 150 minutes of moderate-intensity aerobic activity weekly, alongside resistance training. A structured programme combining behavioural support with pharmacotherapy often yields better outcomes than medication alone.
Investigate potential medical causes for weight plateau or regain. Your clinician may arrange investigations based on your symptoms and clinical features. Conditions such as hypothyroidism, polycystic ovary syndrome (PCOS), or medication-induced weight gain (e.g., from antidepressants, antipsychotics, or corticosteroids) can interfere with weight loss.
Seek urgent medical advice if you experience severe, persistent abdominal pain (especially with vomiting), which could indicate pancreatitis or gallbladder disease—rare but serious side effects of GLP-1 medications. Report any suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Alternatives When Saxenda Is No Longer Effective
When Saxenda fails to maintain efficacy, several alternative pharmacological and non-pharmacological options exist within the UK healthcare system. Wegovy (semaglutide 2.4 mg) is a newer GLP-1 receptor agonist licensed for weight management, administered once weekly rather than daily. NICE (TA875) recommends semaglutide for use in specialist weight management services for eligible patients, typically for a maximum of two years. Clinical trials demonstrate superior weight loss compared to liraglutide, with many patients achieving 10–15% body weight reduction.
Orlistat works through a different mechanism—a lipase inhibitor that reduces dietary fat absorption by approximately 30%. Available on NHS prescription for patients with BMI ≥30 kg/m² (or ≥28 kg/m² with comorbidities), orlistat requires strict adherence to a low-fat diet to minimise gastrointestinal side effects such as oily spotting and faecal urgency. Whilst generally less effective than GLP-1 agonists, it may suit patients seeking a non-injectable option.
Bariatric surgery remains the most effective long-term intervention for severe obesity. NICE (CG189) recommends considering surgery for patients with BMI ≥40 kg/m² (or ≥35 kg/m² with significant comorbidities) who have not achieved adequate weight loss with non-surgical methods. Lower BMI thresholds may apply for people with recent-onset type 2 diabetes and those from certain ethnic backgrounds. Procedures such as gastric bypass or sleeve gastrectomy typically result in 25–30% total body weight loss and significant improvement in obesity-related conditions.
Non-pharmacological approaches should never be overlooked. Referral to specialist weight management services, psychological support for emotional eating, and structured exercise programmes can all contribute meaningfully. Some patients benefit from meal replacement programmes under dietetic supervision. Your GP or specialist can discuss which options are most appropriate for your individual circumstances, considering medical history, comorbidities, and personal preferences.
Frequently Asked Questions
How long does Saxenda typically work before a plateau occurs?
Weight loss plateaus with Saxenda vary individually but commonly occur after several months of treatment as metabolic rate adjusts to lower body weight. NICE recommends reviewing treatment at 12 weeks; patients who initially respond may experience plateaus later, which do not necessarily indicate complete treatment failure but may require additional lifestyle strategies or clinical reassessment.
Can I restart Saxenda if it stopped working previously?
Restarting Saxenda after discontinuation requires clinical assessment by your prescribing doctor or specialist. Your healthcare provider will evaluate why the medication appeared to stop working, whether underlying factors have been addressed, and if reintroduction is appropriate based on your individual circumstances and NICE guidance for weight management services.
Is weight regain inevitable after stopping Saxenda?
Weight regain after stopping Saxenda is common but not inevitable. Maintaining weight loss requires sustained lifestyle modifications including dietary changes and regular physical activity. Patients who continue structured behavioural support, dietetic input, and exercise programmes after discontinuing medication have better long-term weight maintenance outcomes than those who rely solely on pharmacotherapy.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript