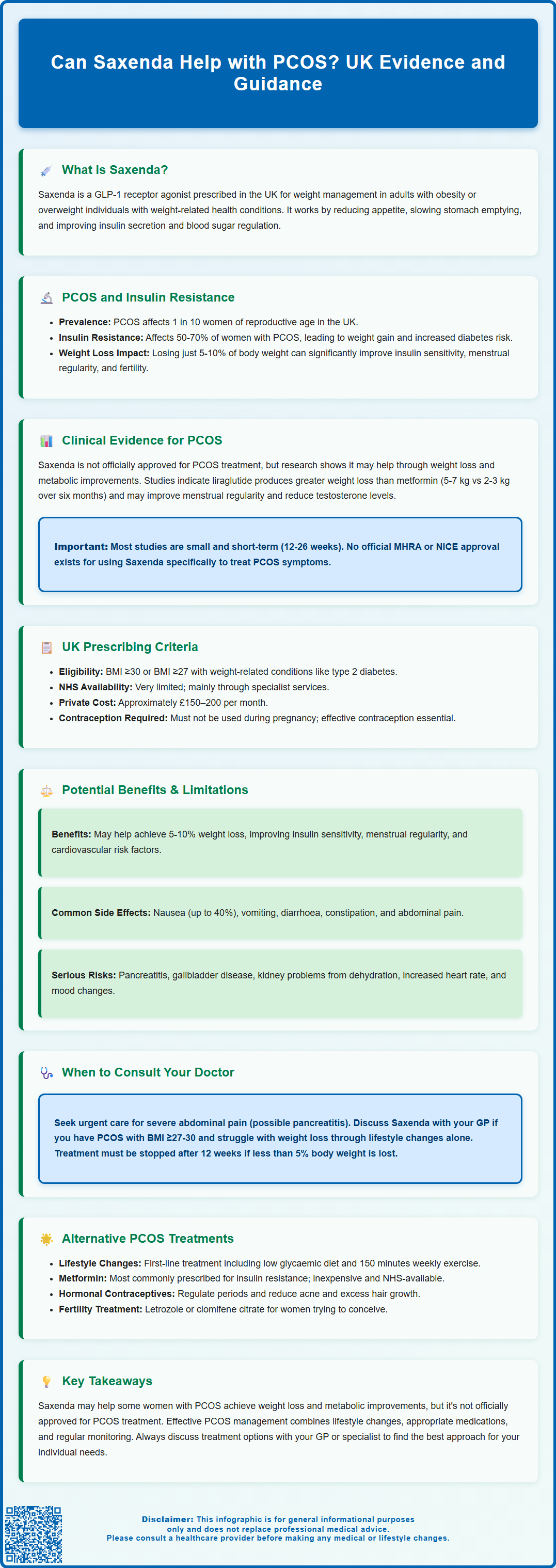
Can Saxenda help with PCOS? Whilst Saxenda (liraglutide 3.0 mg) is not licensed specifically for polycystic ovary syndrome, emerging evidence suggests it may benefit women with PCOS through weight loss and metabolic improvements. As a GLP-1 receptor agonist approved for weight management in the UK, Saxenda addresses key features of PCOS including insulin resistance and obesity. This article examines the clinical evidence, prescribing criteria, potential benefits, and limitations of using Saxenda for PCOS management, alongside alternative treatment options available through the NHS.
Summary: Saxenda may help women with PCOS primarily through weight loss and improved insulin sensitivity, though it is not officially licensed for PCOS treatment in the UK.
- Saxenda is a GLP-1 receptor agonist licensed for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with comorbidities.
- Clinical studies show liraglutide may improve weight loss, insulin sensitivity, menstrual regularity, and androgen levels in women with PCOS.
- Common side effects include nausea, vomiting, and diarrhoea; serious risks include pancreatitis, gallbladder disease, and dehydration requiring monitoring.
- NHS funding is limited; private prescription costs approximately £150–200 monthly, and treatment requires daily subcutaneous injections.
- First-line PCOS management remains lifestyle modification, with metformin, orlistat, and hormonal contraceptives as established alternatives.
- Women must stop Saxenda before attempting pregnancy and use effective contraception during treatment.
Table of Contents
- Understanding Saxenda and Its Mechanism of Action
- The Link Between PCOS, Insulin Resistance, and Weight Management
- Clinical Evidence: Can Saxenda Help with PCOS Symptoms?
- Saxenda Prescribing Criteria and Suitability for PCOS Patients in the UK
- Potential Benefits and Limitations of Saxenda for PCOS Management
- Alternative and Complementary Treatments for PCOS
- Scientific References
- Frequently Asked Questions
Understanding Saxenda and Its Mechanism of Action
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity or those who are overweight with weight-related health conditions. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which were originally developed for treating type 2 diabetes but have proven effective for weight loss at higher doses.
The mechanism of action centres on mimicking a naturally occurring hormone called GLP-1, which is released by the intestines after eating. Saxenda works by:
-
Reducing appetite by acting on areas of the brain that regulate hunger
-
Slowing gastric emptying initially, though this effect may diminish over time
-
Improving insulin secretion in response to food intake
-
Decreasing glucagon release, which helps regulate blood sugar levels
According to the UK Summary of Product Characteristics (SmPC), Saxenda is administered as a once-daily subcutaneous injection, starting at 0.6 mg and increasing by 0.6 mg weekly increments to reach the maintenance dose of 3.0 mg daily. This gradual titration helps minimise common gastrointestinal side effects such as nausea, vomiting, and diarrhoea.
Important safety considerations include risk of pancreatitis (stop treatment and seek urgent medical attention if severe abdominal pain occurs), gallbladder disease, dehydration leading to kidney problems, increased heart rate, and mood changes. Patients should stay well-hydrated, especially if experiencing vomiting or diarrhoea.
Whilst Saxenda is not specifically licensed for polycystic ovary syndrome (PCOS), its effects on weight loss, insulin sensitivity, and metabolic health have generated interest in its potential role for managing PCOS-related symptoms. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Saxenda solely for weight management as part of a comprehensive programme including dietary changes and increased physical activity.
The Link Between PCOS, Insulin Resistance, and Weight Management
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders, affecting approximately one in ten women of reproductive age in the UK. According to the Rotterdam criteria, PCOS is diagnosed when at least two of three features are present: irregular or absent periods, clinical or biochemical signs of excess androgens, and polycystic ovaries on ultrasound.
A critical feature of PCOS is its strong association with insulin resistance, which affects 50–70% of women with the condition, regardless of body weight. Insulin resistance occurs when cells become less responsive to insulin, prompting the pancreas to produce more insulin to maintain normal blood glucose levels. This hyperinsulinaemia contributes to:
-
Increased androgen production by the ovaries, worsening symptoms like excess hair growth and acne
-
Disrupted ovulation, leading to irregular or absent periods and fertility difficulties
-
Weight gain and difficulty losing weight, particularly around the abdomen
-
Increased risk of type 2 diabetes and cardiovascular disease in the long term
Weight management plays a pivotal role in PCOS treatment. Research consistently demonstrates that even modest weight loss of 5–10% of body weight can significantly improve insulin sensitivity, restore more regular menstrual cycles, reduce androgen levels, and enhance fertility outcomes. However, women with PCOS often find weight loss particularly challenging due to the metabolic disturbances inherent to the condition.
The NHS and NICE guidelines emphasise lifestyle modification as the first-line treatment for PCOS, particularly for overweight or obese patients. This includes dietary changes, regular physical activity, and behavioural support. Regular monitoring is essential, including periodic assessment of metabolic parameters (HbA1c or glucose tolerance testing, lipid profile, blood pressure), BMI and waist circumference, and screening for complications such as obstructive sleep apnoea.
Women with PCOS should be referred urgently for assessment if they experience abnormal uterine bleeding. Fertility referral should be considered after 12 months of trying to conceive. Given the difficulties many women face achieving and maintaining weight loss, there is considerable interest in pharmacological interventions that might support these efforts, which is where medications like Saxenda enter the discussion.
Clinical Evidence: Can Saxenda Help with PCOS Symptoms?
Whilst Saxenda is not officially licensed for PCOS treatment, emerging clinical evidence suggests it may offer benefits for women with this condition, primarily through weight loss and metabolic improvements. Several studies have investigated liraglutide (the active ingredient in Saxenda) in PCOS populations, though most research has used doses approved for diabetes (1.2–1.8 mg) rather than the higher Saxenda dose (3.0 mg).
A systematic review and meta-analysis published in the International Journal of Obesity examined randomised controlled trials comparing liraglutide with other treatments in women with PCOS. The findings indicated that liraglutide was associated with:
-
Greater weight loss compared to metformin or placebo
-
Possible improvements in menstrual regularity in some studies
-
Potential reductions in testosterone levels and other androgens
-
Better insulin sensitivity and glucose metabolism markers
One notable study found that women with PCOS taking liraglutide lost an average of 5–7 kg over six months, compared to 2–3 kg with metformin. These metabolic improvements occurred alongside reductions in waist circumference and improvements in cardiovascular risk markers.
However, it is crucial to note several limitations in the current evidence base. Most studies have been relatively small and short-term (typically 12–26 weeks), and there is limited data specifically on the 3.0 mg Saxenda dose in PCOS populations. The reproductive and hormonal benefits appear to be primarily mediated through weight loss and enhanced insulin sensitivity rather than direct effects on ovarian function. Long-term outcomes and effects on fertility remain poorly studied.
Additionally, there is no official indication from the MHRA or NICE for using Saxenda specifically to treat PCOS symptoms. The improvements seen in clinical trials suggest that Saxenda's potential benefits in PCOS are closely tied to its weight management effects, making it most relevant for overweight or obese women with PCOS who struggle with conventional weight loss approaches.
Saxenda Prescribing Criteria and Suitability for PCOS Patients in the UK
In the UK, Saxenda is licensed by the MHRA for weight management in adults who have:
-
Body mass index (BMI) of 30 kg/m² or above (obesity), or
-
BMI of 27 kg/m² or above (overweight) with at least one weight-related comorbidity such as type 2 diabetes, hypertension, or dyslipidaemia
However, NHS funding for Saxenda is more restricted and follows NICE Technology Appraisal guidance. NHS-funded treatment is typically available only through specialist weight management services (Tier 3) for patients meeting specific criteria, and local implementation may vary.
For women with PCOS, the presence of insulin resistance, metabolic syndrome features, or difficulty achieving weight loss through lifestyle measures alone might make them suitable candidates for Saxenda if they meet the BMI criteria. However, prescribers must consider several important factors:
Contraindications and cautions include pregnancy (Saxenda must be stopped if pregnancy occurs), severe gastrointestinal disease, history of pancreatitis, and gallbladder disease. Women of childbearing age should use effective contraception whilst taking Saxenda.
Saxenda is typically available through private prescription in the UK, as NHS funding is limited. Some specialist weight management services may offer it, but availability is not universal. The cost of private treatment is approximately £150–200 per month, which may be prohibitive for many patients.
Treatment should be discontinued after 12 weeks at the 3.0 mg dose if patients have not lost at least 5% of their initial body weight, as continued use is unlikely to provide meaningful benefit. Regular monitoring of weight, metabolic parameters, and side effects is essential throughout treatment.
Women with PCOS considering Saxenda should discuss their individual circumstances, treatment goals, and alternative options with their GP or specialist. Patients should report any suspected side effects via the MHRA Yellow Card scheme.
Potential Benefits and Limitations of Saxenda for PCOS Management
For women with PCOS who meet the prescribing criteria, Saxenda may offer several potential benefits beyond simple weight loss. The metabolic improvements associated with GLP-1 receptor agonists align well with the underlying pathophysiology of PCOS, potentially addressing multiple aspects of the condition simultaneously.
Potential benefits include:
-
Significant weight loss (typically 5–10% of body weight), which can improve virtually all PCOS symptoms
-
Enhanced insulin sensitivity, reducing hyperinsulinaemia and its downstream effects on androgen production
-
Possible improvements in menstrual regularity in some women
-
Potential improvements in cardiovascular risk factors including blood pressure and cholesterol
-
Possible benefits for fertility through weight loss, though Saxenda must be stopped before attempting pregnancy
-
Better quality of life through symptom improvement and increased confidence
However, several important limitations and considerations must be acknowledged. Common side effects include nausea (affecting up to 40% of users), vomiting, diarrhoea, constipation, and abdominal pain, particularly during dose escalation. These gastrointestinal effects can be troublesome enough to cause treatment discontinuation in some patients.
More serious adverse reactions can include:
-
Acute pancreatitis – stop treatment and seek urgent medical attention for severe, persistent abdominal pain, sometimes radiating to the back
-
Gallbladder disease including gallstones and cholecystitis, especially with rapid weight loss
-
Dehydration and acute kidney injury, particularly if experiencing vomiting or diarrhoea
-
Increased heart rate
-
Mood changes including depression and, rarely, suicidal thoughts
Saxenda requires daily injections, which some patients find inconvenient or uncomfortable. The medication is also relatively expensive, and NHS availability is limited. Weight regain after stopping treatment is common unless lifestyle changes are maintained, meaning Saxenda is not a permanent solution.
Crucially, there is no official indication for Saxenda in PCOS treatment, and long-term safety data specifically in PCOS populations remain limited. The medication addresses symptoms rather than curing the underlying condition, and not all women with PCOS will respond equally well. Individual factors including baseline weight, insulin resistance severity, and adherence to lifestyle modifications all influence outcomes.
Alternative and Complementary Treatments for PCOS
Whilst Saxenda may be appropriate for some women with PCOS, it is important to consider the full range of evidence-based treatment options available. NICE guidelines emphasise an individualised approach based on each woman's specific symptoms, concerns, and treatment goals.
First-line lifestyle interventions remain the cornerstone of PCOS management for all patients, particularly those who are overweight. These include:
-
Dietary modification focusing on low glycaemic index foods, reduced refined carbohydrates, and balanced macronutrient intake
-
Regular physical activity (at least 150 minutes of moderate-intensity exercise weekly)
-
Behavioural support through weight management programmes or psychological interventions
Metformin is the most commonly prescribed medication for PCOS in the UK, particularly for women with insulin resistance or impaired glucose tolerance. Whilst it typically produces more modest weight loss than Saxenda (2–3 kg on average), it is well-established, inexpensive, and available on NHS prescription. Metformin can improve insulin sensitivity, support modest weight loss, and may help restore menstrual regularity.
Orlistat is another licensed weight-loss medication available on the NHS that may be suitable for some women with PCOS. For those with severe obesity (typically BMI ≥35–40 with comorbidities), bariatric surgery referral should be considered according to NICE guidance (CG189).
Hormonal contraceptives (combined oral contraceptive pills) are frequently used to regulate menstrual cycles and reduce androgen-related symptoms such as acne and hirsutism. Anti-androgen medications like spironolactone (requires potassium monitoring) or cyproterone acetate (restricted by MHRA due to meningioma risk; use lowest dose for shortest duration) may be added for persistent symptoms. Effective contraception is essential with anti-androgen treatment.
For women trying to conceive, fertility treatments including letrozole (first-line) or clomifene citrate can induce ovulation. Weight loss prior to fertility treatment significantly improves success rates. Referral to fertility services should be considered after 12 months of trying to conceive.
Emerging treatments being investigated include inositol supplements (particularly myo-inositol), which may improve insulin sensitivity and ovarian function, though evidence remains limited.
The optimal approach typically involves combining multiple strategies tailored to individual needs. Women with PCOS should work closely with their GP, and may benefit from referral to specialist services including endocrinology, gynaecology, or dedicated PCOS clinics. Regular monitoring of symptoms, metabolic health, and long-term complications such as diabetes and cardiovascular disease is essential for comprehensive PCOS management.
Scientific References
- Saxenda 6 mg/mL solution for injection in pre-filled pen - Summary of Product Characteristics.
- Saxenda: EPAR - Public Assessment Report.
- Overweight and obesity management (NG246).
- Anti-obesity pharmacological agents for polycystic ovary syndrome: systematic review and meta-analysis to inform the 2023 international evidence-based guideline.
- Obesity - Treatment.
Frequently Asked Questions
Is Saxenda approved for treating PCOS in the UK?
No, Saxenda is not officially licensed by the MHRA for PCOS treatment. It is approved solely for weight management in adults with obesity or overweight with weight-related comorbidities, though emerging evidence suggests potential benefits for PCOS symptoms through weight loss and metabolic improvements.
How does Saxenda improve PCOS symptoms?
Saxenda may improve PCOS symptoms primarily through weight loss and enhanced insulin sensitivity. Clinical studies suggest it can reduce androgen levels, improve menstrual regularity, and address metabolic disturbances, though these benefits appear mediated through weight reduction rather than direct effects on ovarian function.
Can I get Saxenda on the NHS for PCOS?
NHS funding for Saxenda is highly restricted and typically available only through specialist weight management services (Tier 3) for patients meeting specific criteria. Most women with PCOS would need private prescription, costing approximately £150–200 monthly, if they meet the BMI requirements of ≥30 kg/m² or ≥27 kg/m² with comorbidities.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript