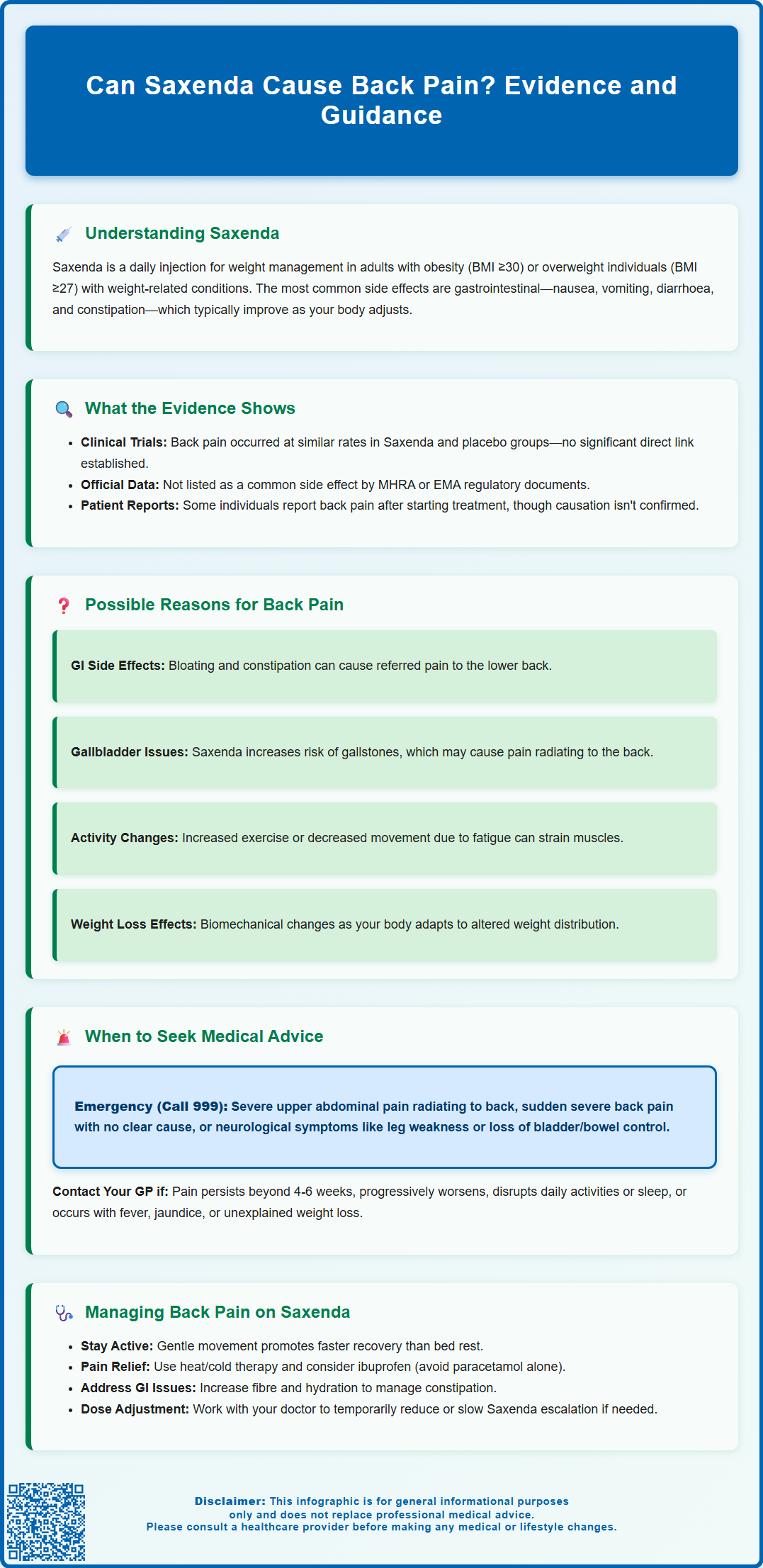
Can Saxenda cause back pain? Whilst back pain is not listed among the common side effects in official prescribing information, some patients report experiencing this symptom during treatment with Saxenda (liraglutide 3.0 mg), a GLP-1 receptor agonist used for weight management. Understanding the potential relationship between this medication and back pain, along with recognising when symptoms require medical attention, is important for patients and healthcare professionals. This article examines the evidence, explores possible mechanisms, and provides guidance on managing back pain whilst taking Saxenda.
Summary: Back pain is not officially listed as a common side effect of Saxenda, though some patients report it during treatment, potentially due to gastrointestinal effects, gallbladder disease, or musculoskeletal changes.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities.
- Back pain does not appear in the Summary of Product Characteristics as a common side effect, and clinical trials showed no significant increase versus placebo.
- Possible indirect causes include referred pain from gastrointestinal side effects, gallbladder disease, postural changes, or musculoskeletal adaptation to weight loss.
- Seek urgent medical attention for severe upper abdominal pain radiating to the back, neurological symptoms, or sudden severe back pain without mechanical cause.
- Management includes conservative measures (activity, analgesia), addressing contributing factors like constipation, and medication review with the prescribing clinician.
- Report suspected side effects through the MHRA Yellow Card Scheme to support ongoing medication safety monitoring.
Table of Contents
Understanding Saxenda and Its Common Side Effects
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or those who are overweight (BMI ≥27 kg/m²) with weight-related health conditions. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking a naturally occurring hormone that regulates appetite and food intake.
The mechanism of action involves binding to GLP-1 receptors in the brain, particularly in areas that control appetite. This leads to increased feelings of fullness, reduced hunger, and consequently lower calorie intake. Saxenda also delays gastric emptying, which can affect the absorption of oral medicines. It is administered as a once-daily subcutaneous injection, typically in the abdomen, thigh, or upper arm. The dose is gradually increased over five weeks to minimise side effects, reaching a maintenance dose of 3.0 mg daily.
Common side effects associated with Saxenda predominantly affect the gastrointestinal system, as GLP-1 receptors are abundant in the digestive tract. According to the MHRA-approved Summary of Product Characteristics (SmPC), the most frequently reported adverse effects include:
-
Nausea and vomiting (affecting more than 1 in 10 people)
-
Diarrhoea or constipation
-
Abdominal pain or discomfort
-
Indigestion and gastro-oesophageal reflux (GORD)
-
Headache
-
Injection site reactions (redness, itching, or bruising)
-
Gallbladder disorders including gallstones (cholelithiasis) and inflammation (cholecystitis)
-
Increased heart rate
These side effects are usually most pronounced during the initial weeks of treatment and often diminish as the body adjusts to the medication. Most gastrointestinal side effects are mild to moderate in severity and resolve without discontinuing treatment. However, patients should be aware that individual responses vary, and some may experience persistent or more troublesome symptoms that require medical review.
Treatment should be discontinued after 12 weeks on the 3.0 mg daily dose if patients have not lost at least 5% of their initial body weight.
Can Saxenda Cause Back Pain? Examining the Evidence
The relationship between Saxenda and back pain is not straightforward, and there is no official direct link established in the primary clinical trial data. Back pain is not listed among the common or very common side effects in the Summary of Product Characteristics (SmPC) approved by the MHRA or the European Medicines Agency (EMA).
However, post-marketing surveillance and patient reports have documented instances of back pain occurring during Saxenda treatment. In the SCALE clinical trial programme, which included over 5,000 participants, musculoskeletal symptoms including back pain were reported, though the frequency did not appear to be significantly higher than in placebo groups. This suggests that when back pain does occur, it may not always be directly caused by the medication itself.
Important considerations when evaluating this potential association include:
-
Incidence rates: Back pain was reported as an adverse event in clinical trials but did not reach statistical significance compared to control groups
-
Temporal relationship: Some patients report back pain beginning shortly after starting Saxenda or increasing the dose
-
Individual variation: Not all patients experience back pain, and those who do may have other contributing factors
The Yellow Card scheme operated by the MHRA allows healthcare professionals and patients to report suspected side effects. It's important to note that Yellow Card reports cannot establish causality or frequency of side effects, but they help regulatory authorities monitor medication safety. The presence of back pain reports among Saxenda users through this system does not confirm a causal relationship but contributes to ongoing safety monitoring.
Why Back Pain May Occur During Saxenda Treatment
While a direct pharmacological mechanism linking Saxenda to back pain has not been established, several plausible explanations exist for why some patients may experience this symptom during treatment.
Gastrointestinal effects and referred pain: The most common side effects of Saxenda involve the digestive system. Severe or persistent gastrointestinal symptoms such as bloating, constipation, or abdominal cramping can sometimes manifest as referred pain in the lower back. The proximity of abdominal organs to the lumbar spine means that visceral discomfort may be perceived as back pain. Additionally, chronic constipation—a recognised side effect of GLP-1 receptor agonists—can contribute to lower back discomfort.
Gallbladder disease: Saxenda is associated with an increased risk of gallbladder disorders, including gallstones (cholelithiasis) and inflammation (cholecystitis). These conditions can present with pain in the right upper abdomen that may radiate to the back, particularly the right shoulder blade area. The risk increases with greater weight loss and is listed as a common side effect in the SmPC.
Postural and activity changes: Patients using Saxenda for weight management may simultaneously increase physical activity levels as part of their overall lifestyle modification programme. Individuals who have been relatively sedentary may experience musculoskeletal discomfort, including back pain, when beginning new exercise routines. Conversely, the initial side effects of nausea and fatigue might lead to reduced activity and poor posture, potentially contributing to back pain.
Pancreatitis considerations: Though rare, acute pancreatitis is a serious potential side effect of GLP-1 receptor agonists. Pancreatitis typically presents with severe upper abdominal pain that may radiate to the back. Whilst this is uncommon, it represents an important differential diagnosis that should not be overlooked if back pain is accompanied by severe abdominal pain, nausea, or vomiting.
Weight loss and musculoskeletal adaptation: As patients lose weight, the body undergoes biomechanical changes. The musculoskeletal system must adapt to altered weight distribution and centre of gravity, which can temporarily cause discomfort in weight-bearing structures including the spine. This is generally a transient phenomenon as the body adjusts.
Renal complications: In rare cases, severe gastrointestinal side effects may lead to dehydration, which could affect kidney function. Renal impairment might present with flank or back pain, particularly if accompanied by reduced urine output.
When to Seek Medical Advice About Back Pain on Saxenda
Whilst mild, transient back pain may not require immediate medical attention, certain warning signs indicate the need for prompt evaluation by a healthcare professional. Patients should contact their GP or prescribing clinician if they experience:
Urgent symptoms requiring emergency assessment (call 999 or go to A&E):
-
Severe upper abdominal pain radiating to the back, particularly if accompanied by nausea, vomiting, or fever (potential pancreatitis)
-
Sudden onset of severe back pain with no obvious mechanical cause
-
Neurological symptoms such as leg weakness, numbness, tingling, or loss of bladder or bowel control (especially new urinary retention/incontinence or saddle anaesthesia, which may indicate cauda equina syndrome)
Symptoms warranting GP consultation:
-
Back pain that persists or is not improving after a few weeks (4-6 weeks) despite simple measures
-
Pain that progressively worsens rather than improves
-
Back pain that significantly interferes with daily activities or sleep
-
Right upper abdominal pain, fever, or yellowing of the skin/eyes (possible gallbladder disease)
-
Uncertainty about whether symptoms are related to Saxenda or another condition
-
Back pain accompanied by unexplained weight loss (beyond expected treatment effects), fever, or night sweats
When consulting a healthcare professional, patients should provide a comprehensive history including:
-
When the back pain started in relation to commencing Saxenda or dose increases
-
The character, location, and severity of the pain
-
Any aggravating or relieving factors
-
Other symptoms experienced concurrently
-
Previous history of back problems
This information enables clinicians to distinguish between Saxenda-related effects, coincidental musculoskeletal problems, and potentially serious complications requiring specific investigation or management.
Managing Back Pain While Taking Saxenda
For patients experiencing back pain during Saxenda treatment, a systematic approach to management can help determine whether continuation of the medication is appropriate whilst addressing symptoms effectively.
Initial conservative measures that may provide relief include:
-
Maintaining activity: Avoiding prolonged bed rest is important for most back pain. Gentle movement and continuation of normal activities as tolerated generally promotes faster recovery, in line with NICE guidance (NG59)
-
Heat or cold therapy: Applying a warm compress or cold pack to the affected area for 15-20 minutes several times daily may reduce discomfort
-
Over-the-counter analgesia: Consider an oral NSAID such as ibuprofen (if not contraindicated) at the lowest effective dose for the shortest duration. Paracetamol alone is not recommended for low back pain according to NICE guidance. Check with a pharmacist or doctor before taking NSAIDs if you have stomach, kidney, heart problems or are taking other medications
-
Posture awareness: Ensuring good posture during sitting, standing, and sleeping may prevent exacerbation of symptoms
Addressing potential contributing factors:
If gastrointestinal side effects such as constipation are present, managing these may indirectly improve back pain. Strategies include increasing dietary fibre, maintaining adequate hydration, and discussing with a healthcare professional whether a laxative might be appropriate. Patients should also review their physical activity programme to ensure they are not overexerting themselves, particularly if recently increasing exercise intensity.
Medication review: In consultation with the prescribing clinician, options may include:
-
Temporarily reducing the Saxenda dose to assess whether symptoms improve
-
Slowing the dose escalation schedule
-
Discontinuing Saxenda if back pain is severe, persistent, or accompanied by concerning features
NICE guidance on low back pain and sciatica (NG59) recommends considering referral for physiotherapy or structured exercise programmes for persistent symptoms. Patients should work collaboratively with their healthcare team to balance the benefits of continued weight management treatment against any adverse effects experienced, ensuring that the overall approach remains safe and tolerable.
Patients are encouraged to report any suspected side effects to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk), which helps monitor the safety of medicines.
Frequently Asked Questions
Is back pain a common side effect of Saxenda?
No, back pain is not listed as a common side effect in the official Summary of Product Characteristics for Saxenda. Clinical trials did not show a statistically significant increase in back pain compared to placebo groups, though some patients do report this symptom during treatment.
What should I do if I experience back pain whilst taking Saxenda?
For mild back pain, try conservative measures such as maintaining activity, applying heat or cold therapy, and using appropriate analgesia. Contact your GP if pain persists beyond 4-6 weeks, worsens progressively, or is accompanied by other concerning symptoms such as severe abdominal pain or neurological changes.
Could back pain on Saxenda indicate a serious complication?
Whilst most back pain is not serious, severe upper abdominal pain radiating to the back could indicate pancreatitis or gallbladder disease, both recognised complications of GLP-1 receptor agonists. Seek emergency medical attention if you experience severe pain with nausea, vomiting, fever, or any neurological symptoms.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript