Can I take Saxenda while breastfeeding? This is an important question for new mothers considering weight management options. Saxenda (liraglutide) is a GLP-1 receptor agonist licensed for weight management, but current UK guidance clearly advises against its use during breastfeeding. The Medicines and Healthcare products Regulatory Agency (MHRA) and manufacturer state that Saxenda should be avoided whilst nursing due to insufficient data on excretion into breast milk and potential effects on infants. This article examines the evidence, safety considerations, and alternative approaches to weight management for breastfeeding mothers, helping you make informed decisions in consultation with your healthcare provider.
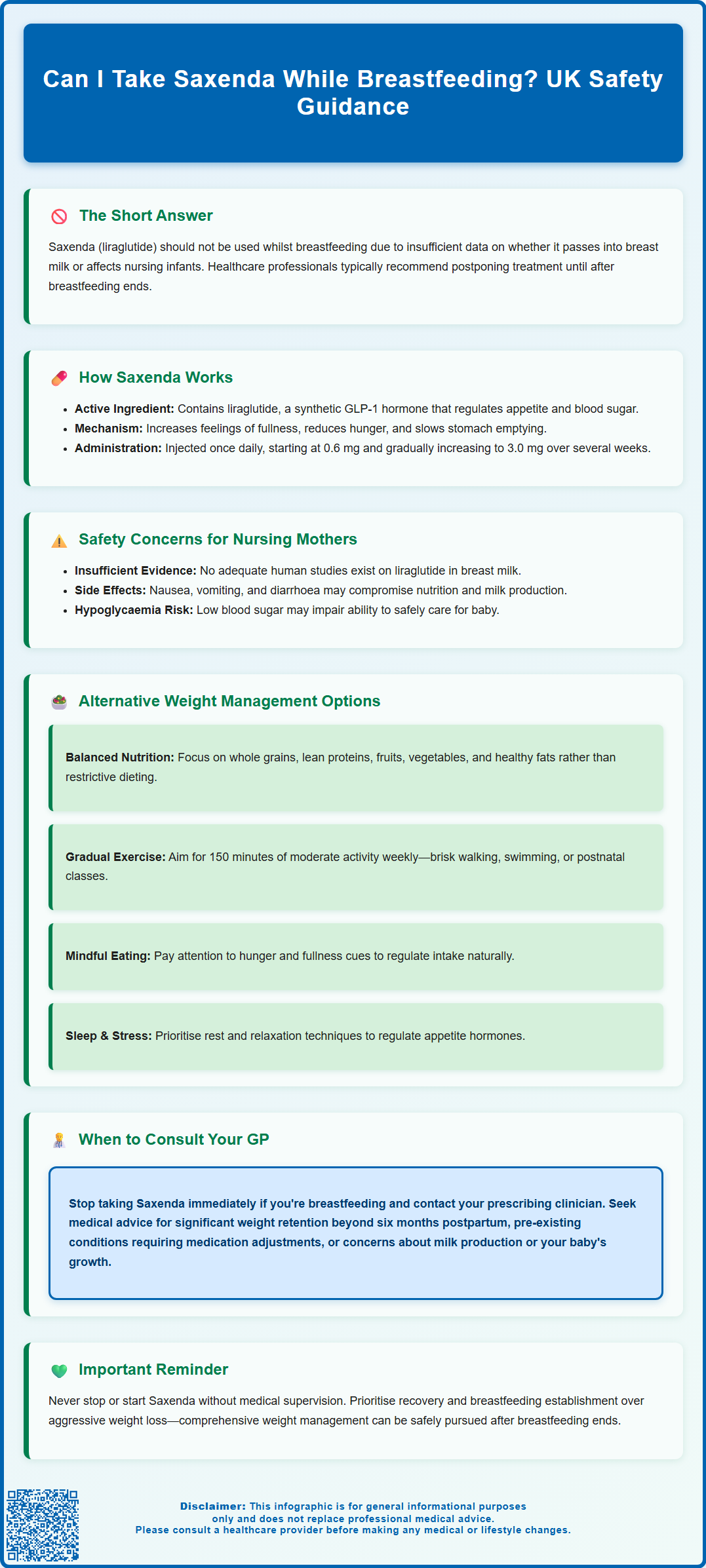
Summary: Saxenda (liraglutide) should not be used during breastfeeding due to insufficient data on excretion into breast milk and potential effects on nursing infants.
- Liraglutide is a GLP-1 receptor agonist that reduces appetite and slows gastric emptying to support weight management.
- UK regulatory guidance (MHRA, manufacturer SmPC) contraindicates Saxenda use whilst breastfeeding due to lack of human safety data.
- Animal studies show liraglutide presence in milk, but relevance to human lactation remains unclear.
- Non-pharmacological approaches including balanced nutrition, gradual physical activity, and behavioural support are recommended for postpartum weight management.
- Consult your GP immediately if currently taking Saxenda and breastfeeding, or before starting any weight management medication during lactation.
Table of Contents
Can I Take Saxenda While Breastfeeding?
Saxenda (liraglutide) should not be used during breast-feeding. The Medicines and Healthcare products Regulatory Agency (MHRA) and the manufacturer clearly state in the Summary of Product Characteristics (SmPC) that Saxenda should be avoided whilst breastfeeding due to insufficient data on whether the medication passes into breast milk and what effects it might have on nursing infants.
Currently, there are no adequate studies examining liraglutide excretion in human breast milk or its potential impact on breastfed babies. Animal studies have shown that liraglutide and similar compounds can be detected in milk, though the relevance to human lactation remains unclear. Given this uncertainty and the fact that Saxenda is not essential for immediate health preservation, regulatory bodies adopt a precautionary approach.
The decision to use any medication whilst breastfeeding requires careful consideration of the benefits to the mother against potential risks to the infant. For weight management medications like Saxenda, which are used for non-urgent conditions, healthcare professionals typically recommend postponing treatment until after breastfeeding has concluded. This approach prioritises infant safety whilst the evidence base remains limited.
If you are currently taking Saxenda and discover you are breastfeeding, or if you are considering starting Saxenda whilst nursing, it is essential to discuss this with your GP or prescribing clinician immediately. They can provide personalised advice based on your individual circumstances and help you explore safer alternatives for weight management during this period. Never stop or start Saxenda without medical supervision, as abrupt changes may affect your metabolic control, particularly if you have other related health conditions.
How Saxenda Works and Its Active Ingredient
Saxenda contains liraglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist that is licensed for weight management. Liraglutide is a synthetic analogue of human GLP-1, a naturally occurring hormone produced in the intestine that plays a crucial role in appetite regulation and glucose metabolism.
The mechanism of action involves several physiological pathways. Liraglutide binds to GLP-1 receptors in the brain, particularly in areas that control appetite and food intake. This activation leads to increased feelings of satiety (fullness) and reduced hunger, helping individuals consume fewer calories. Additionally, liraglutide slows gastric emptying, meaning food remains in the stomach longer, which contributes to prolonged satiety after meals.
In terms of glucose regulation, liraglutide stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner—meaning it only promotes insulin release when blood glucose levels are elevated. It also suppresses glucagon secretion, a hormone that raises blood glucose. These combined effects help improve glycaemic control in people with type 2 diabetes.
Saxenda is administered as a once-daily subcutaneous injection, typically in the abdomen, thigh, or upper arm. The dose is gradually increased over several weeks from 0.6 mg to 3.0 mg to minimise gastrointestinal side effects. The medication has a half-life of approximately 13 hours, allowing for once-daily dosing. It is prescribed alongside a reduced-calorie diet and increased physical activity as part of a comprehensive weight management programme for adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with weight-related comorbidities such as hypertension or dyslipidaemia.
Safety Considerations for Breastfeeding Mothers
The primary safety concern regarding Saxenda during breastfeeding centres on the lack of human data. Pharmaceutical manufacturers and regulatory authorities require robust evidence before recommending medication use in breastfeeding women, and such evidence is currently absent for liraglutide. The precautionary principle therefore applies: without proof of safety, the medication should be avoided.
Animal studies provide limited reassurance. Research in lactating rats demonstrated that liraglutide and its metabolites were present in milk at concentrations lower than those found in maternal plasma. However, extrapolating animal data to human lactation is problematic due to differences in milk composition, feeding patterns, and infant metabolism. Furthermore, the potential effects on infant growth, development, and metabolic function remain unknown.
Beyond the question of drug transfer into breast milk, there are additional considerations. Saxenda commonly causes gastrointestinal adverse effects including nausea, vomiting, diarrhoea, and constipation. These side effects could potentially affect a mother's nutritional status and hydration, which are important for maintaining adequate milk production. Severe nausea or vomiting might compromise a mother's ability to maintain proper nutrition during the demanding period of breastfeeding.
There is also a concern about hypoglycaemia (low blood sugar), particularly when liraglutide is combined with insulin or sulfonylureas in women with diabetes. Hypoglycaemic episodes could impair a mother's ability to safely care for her infant. Additionally, calorie restriction often accompanying Saxenda treatment may not provide sufficient energy for breastfeeding mothers, who need adequate nutrition to support milk production.
The UK Drugs in Lactation Advisory Service (UKDILAS) and similar specialist resources consistently advise against liraglutide use during breastfeeding, reinforcing the manufacturer's guidance. If weight management is medically necessary during breastfeeding, non-pharmacological approaches should be prioritised, with any medication decisions made collaboratively with healthcare professionals who can assess individual risk-benefit profiles.
If you experience any suspected side effects from medications, report them via the MHRA Yellow Card scheme.
Alternative Weight Management Options During Breastfeeding
Breastfeeding mothers seeking to manage their weight have several evidence-based, safer alternatives to pharmacological interventions. The postpartum period presents unique nutritional demands, and any weight management strategy must ensure adequate nutrition to support both maternal health and milk production.
Dietary modifications should be gradual and balanced. UK guidance suggests that breastfeeding women should focus on sustainable, gradual weight loss rather than rapid results. A well-balanced diet rich in whole grains, lean proteins, fruits, vegetables, and healthy fats provides essential nutrients whilst supporting gradual weight reduction. Breastfeeding itself requires energy, but restrictive dieting should be avoided as it may affect milk supply and maternal wellbeing. The NHS recommends focusing on nutritional quality rather than calorie counting during breastfeeding.
Physical activity offers significant benefits for postpartum weight management and overall wellbeing. The UK Chief Medical Officers' guidelines recommend that adults, including postpartum women, aim for at least 150 minutes of moderate-intensity activity weekly. This might include brisk walking, swimming, postnatal exercise classes, or cycling. Exercise can begin gradually after birth, with the timeline depending on delivery type and any complications. Pelvic floor exercises should be incorporated to address postpartum muscular changes.
Behavioural strategies and support systems play a vital role in sustainable weight management. These include:
-
Mindful eating practices – paying attention to hunger and fullness cues
-
Adequate sleep – though challenging with a newborn, prioritising rest when possible helps regulate appetite hormones
-
Stress management – techniques such as relaxation exercises or seeking support for postnatal mental health
-
Structured meal planning – preparing nutritious meals in advance to avoid reliance on convenience foods
Many areas offer NHS weight management services that can support postpartum women, though availability varies by location. Your GP can advise on local services and referral options. Consultation with a registered dietitian can provide personalised nutritional advice that accounts for breastfeeding requirements, food preferences, and any medical conditions. These multifaceted, non-pharmacological approaches offer effective weight management without the uncertainties associated with medication use during lactation.
When to Consult Your GP or Healthcare Provider
Several situations warrant prompt consultation with your GP or healthcare provider regarding weight management during breastfeeding. If you are currently taking Saxenda and have recently given birth or are planning to breastfeed, contact your prescribing clinician immediately to discuss discontinuation and alternative strategies. Similarly, if you are breastfeeding and considering starting Saxenda, a thorough discussion with your GP is essential before making any decisions.
Seek medical advice if you are experiencing difficulties with postpartum weight that are affecting your physical or mental health. Significant weight retention beyond six months postpartum, or conversely, excessive or rapid weight loss, may indicate underlying issues requiring professional assessment. Your GP can evaluate potential contributing factors such as thyroid dysfunction, polycystic ovary syndrome (PCOS), or postnatal depression, all of which can affect weight and may require specific management.
If you have pre-existing conditions such as type 2 diabetes, hypertension, or cardiovascular disease, weight management becomes more complex during breastfeeding. These conditions may have previously been managed with medications that are also contraindicated or require careful consideration during lactation. Your GP or specialist can review your medication regimen and adjust treatment plans to ensure both maternal and infant safety whilst maintaining disease control.
Contact your healthcare provider if you experience:
-
Difficulty producing adequate breast milk despite proper technique and frequency
-
Symptoms of nutritional deficiency (fatigue, hair loss, poor wound healing)
-
Signs of postnatal depression or anxiety affecting your ability to care for yourself or your baby
-
Concerns about your infant's growth or feeding patterns
-
Pressure from others to lose weight rapidly, causing distress
Specialist referral may be appropriate in certain circumstances. Your GP can refer you to a dietitian for tailored nutritional guidance, an endocrinologist if metabolic conditions complicate weight management, or a lactation consultant if breastfeeding difficulties arise. For women with complex medical histories or significant obesity (BMI ≥35 kg/m² with comorbidities or ≥40 kg/m²), referral to specialist weight management services may be considered, though criteria vary locally.
Remember that the postpartum period is not the optimal time for aggressive weight loss interventions. Prioritising your recovery, establishing breastfeeding, and caring for your newborn are paramount. Weight management can be addressed more comprehensively once breastfeeding is established or completed, allowing for a broader range of safe and effective treatment options including, if appropriate, medications like Saxenda under proper medical supervision.
Frequently Asked Questions
Why is Saxenda not recommended during breastfeeding?
Saxenda is not recommended during breastfeeding because there is insufficient data on whether liraglutide passes into breast milk or what effects it might have on nursing infants. UK regulatory bodies adopt a precautionary approach when evidence of safety is lacking.
What are safe alternatives to Saxenda for weight management whilst breastfeeding?
Safe alternatives include gradual dietary modifications with balanced nutrition, regular physical activity (at least 150 minutes weekly of moderate-intensity exercise), behavioural strategies such as mindful eating, and support from NHS weight management services or registered dietitians.
When should I contact my GP about weight management during breastfeeding?
Contact your GP if you are currently taking Saxenda and breastfeeding, experiencing significant postpartum weight concerns affecting your health, have pre-existing conditions like diabetes requiring medication review, or notice difficulties with milk production or signs of nutritional deficiency.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










