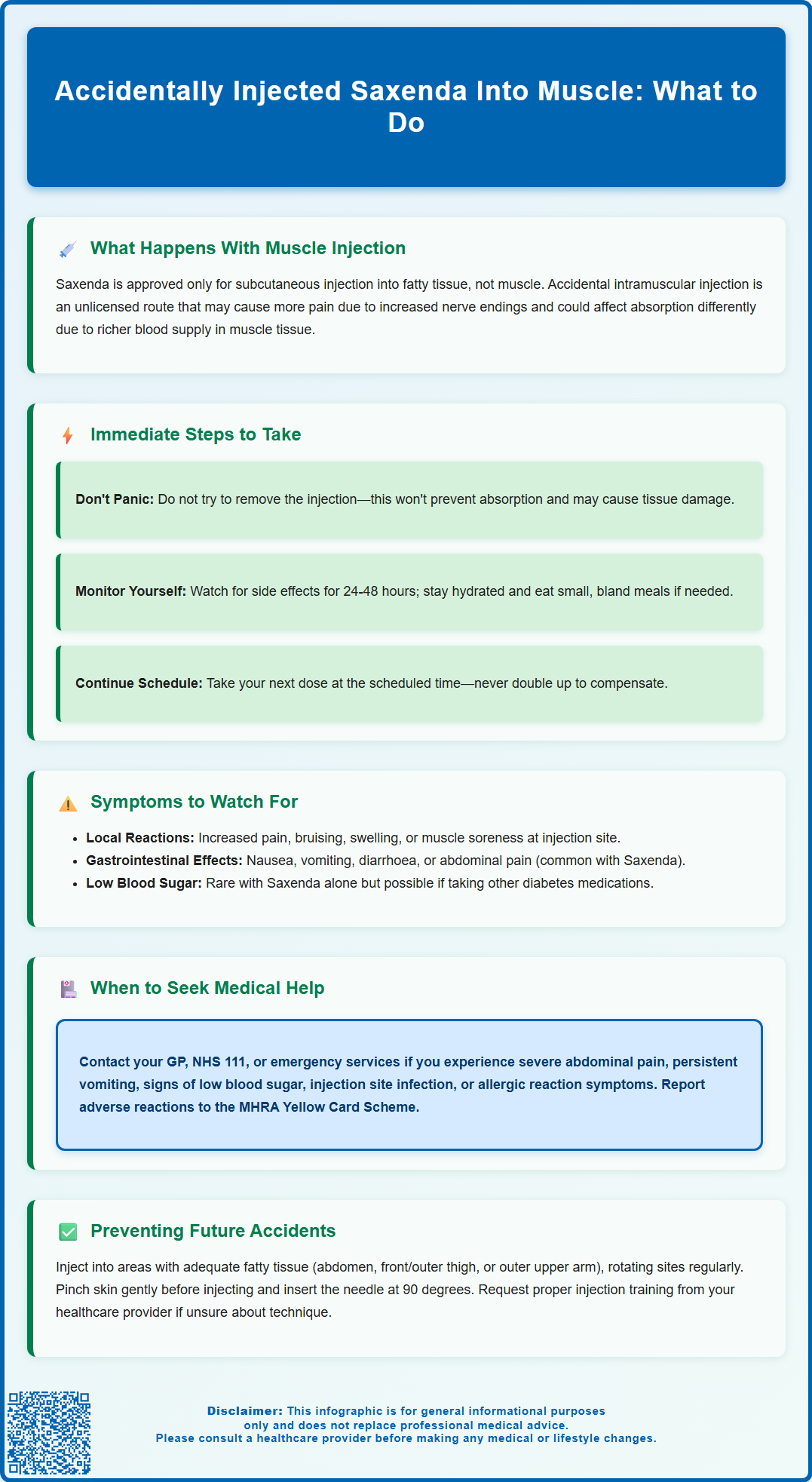
Accidentally injecting Saxenda into muscle rather than subcutaneous tissue is a deviation from the approved administration route that can cause concern. Saxenda (liraglutide) is a GLP-1 receptor agonist licensed for weight management and must be administered subcutaneously into fatty tissue beneath the skin. Whilst intramuscular injection has not been specifically studied for this medication, it may result in increased injection site discomfort and potentially altered absorption. Understanding what to do if this occurs, recognising symptoms to monitor, and learning proper injection technique are essential for safe medication use. This article provides evidence-based guidance aligned with UK regulatory standards and clinical practice.
Summary: Accidental intramuscular injection of Saxenda represents an unlicensed route that may cause increased injection site pain and has not been studied for safety or absorption characteristics.
- Saxenda (liraglutide) is a GLP-1 receptor agonist licensed exclusively for subcutaneous injection into fatty tissue
- Intramuscular injection may cause greater localised discomfort due to increased nerve endings in muscle tissue
- Do not take an additional dose to compensate; continue with your next scheduled dose as normal
- Monitor for gastrointestinal symptoms, injection site reactions, and signs of hypoglycaemia if you have diabetes
- Seek medical advice if you experience severe abdominal pain, persistent vomiting, or signs of allergic reaction
- Proper injection technique includes pinching skin, using appropriate sites with adequate subcutaneous fat, and rotating injection locations
Table of Contents
- What Happens If Saxenda Is Injected Into Muscle Instead of Subcutaneous Tissue
- Immediate Steps to Take After Accidental Intramuscular Injection of Saxenda
- Symptoms and Side Effects of Intramuscular Saxenda Injection
- How to Prevent Accidental Muscle Injection When Using Saxenda
- Frequently Asked Questions
What Happens If Saxenda Is Injected Into Muscle Instead of Subcutaneous Tissue
Saxenda (liraglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with weight-related comorbidities. It is also approved for use in adolescents (12 to <18 years) meeting specific criteria. The medication is specifically formulated and approved for subcutaneous injection only, meaning it should be administered into the fatty tissue layer beneath the skin, typically in the abdomen, thigh, or upper arm.
When Saxenda is accidentally injected into muscle tissue (intramuscular injection), this represents an unlicensed route of administration that has not been studied for safety or pharmacokinetics. In theory, intramuscular tissue has a richer blood supply compared to subcutaneous fat, which could potentially affect how the medication is absorbed, though this has not been specifically studied for liraglutide.
The Medicines and Healthcare products Regulatory Agency (MHRA) and the Summary of Product Characteristics (SmPC) for Saxenda clearly specify subcutaneous administration only. Intramuscular injection may cause localised discomfort, including pain at the injection site, as muscle tissue contains more nerve endings than subcutaneous fat.
It is important to understand that an accidental intramuscular injection represents a deviation from the approved route of administration. If you suspect this has happened, monitor for any unusual symptoms and contact a healthcare professional if you have concerns. Patients should be familiar with proper injection technique to ensure optimal therapeutic effect and minimise potential adverse reactions.
Immediate Steps to Take After Accidental Intramuscular Injection of Saxenda
If you suspect you have accidentally injected Saxenda into muscle rather than subcutaneous tissue, there are several practical steps you should take to ensure your safety and wellbeing.
Do not attempt to remove or reverse the injection. Once the medication has been administered, it will be absorbed by the body. Attempting to manipulate the injection site will not prevent absorption and may cause additional tissue damage or bruising.
Monitor yourself for adverse effects over the next 24-48 hours, particularly gastrointestinal symptoms. These may include nausea, vomiting, abdominal discomfort, or diarrhoea. Stay well hydrated and consider eating small, bland meals if you feel able.
Take your next scheduled dose as normal at the usual time. Do not administer another dose to compensate for the potentially altered absorption. Taking an additional dose could lead to overdose symptoms, including severe nausea, vomiting, and hypoglycaemia (low blood sugar), particularly if you have type 2 diabetes or are taking other glucose-lowering medications.
Contact your GP, practice nurse, or NHS 111 if you experience concerning symptoms, including:
-
Severe or persistent abdominal pain, especially if radiating to your back (may indicate pancreatitis)
-
Persistent vomiting preventing fluid intake
-
Signs of hypoglycaemia (shakiness, confusion, sweating, rapid heartbeat)
-
Severe injection site pain, swelling, or signs of infection
-
Symptoms of gallbladder problems (pain in upper right abdomen, fever, yellowing of skin/eyes)
-
Signs of allergic reaction (rash, swelling, difficulty breathing)
Call 999 if you experience severe allergic reaction symptoms or severe, sudden abdominal pain with vomiting.
Report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Document the incident and inform your healthcare provider at your next appointment. This information helps them provide appropriate guidance and reinforces proper injection technique. Your practice nurse or diabetes specialist nurse can offer additional training on correct administration if needed.
Symptoms and Side Effects of Intramuscular Saxenda Injection
The symptoms following accidental intramuscular injection of Saxenda may include the known adverse effects of the medication, though the impact of intramuscular versus subcutaneous administration has not been specifically studied.
Gastrointestinal symptoms are the most commonly reported adverse effects of Saxenda. These include:
-
Nausea and vomiting – the most frequent side effects, affecting more than 1 in 10 users with standard subcutaneous administration
-
Diarrhoea or constipation
-
Abdominal pain or discomfort
-
Dyspepsia (indigestion)
-
Reduced appetite (which is part of the therapeutic mechanism)
Local injection site reactions may differ from those seen with subcutaneous injection. Intramuscular injection can cause:
-
More significant pain or tenderness at the injection site
-
Bruising or haematoma formation
-
Localised swelling
-
Muscle soreness that may persist for several days
Hypoglycaemia (low blood sugar) is uncommon with Saxenda monotherapy in people without diabetes, as GLP-1 receptor agonists have a glucose-dependent mechanism of action. However, if you have type 2 diabetes and take other glucose-lowering medications (particularly insulin or sulphonylureas), there may be an increased risk. Symptoms include trembling, sweating, confusion, palpitations, and hunger.
Serious adverse effects requiring immediate medical attention include:
-
Pancreatitis: persistent, severe abdominal pain, sometimes radiating to the back, often with vomiting
-
Gallbladder problems: pain in the upper right abdomen, fever, yellowing of skin or eyes
-
Severe allergic reactions: rash, swelling of face/throat, difficulty breathing
-
Dehydration from persistent vomiting or diarrhoea, which may affect kidney function
If you experience severe, persistent, or concerning symptoms following an accidental intramuscular injection, seek medical advice promptly through your GP, NHS 111, or emergency services as appropriate. Report suspected adverse reactions to the MHRA Yellow Card Scheme.
How to Prevent Accidental Muscle Injection When Using Saxenda
Preventing accidental intramuscular injection of Saxenda requires understanding proper injection technique and selecting appropriate injection sites. The following guidance is based on the Saxenda Summary of Product Characteristics (SmPC), Patient Information Leaflet (PIL), and Forum for Injection Technique UK (FIT UK) recommendations.
Choose appropriate injection sites with adequate subcutaneous tissue. Saxenda should be injected into areas with sufficient fatty tissue:
-
Abdomen – at least 5 cm away from the navel, avoiding the midline. This site typically has the most consistent subcutaneous fat layer.
-
Thigh – the front or outer aspect of the upper thigh, where subcutaneous tissue is usually adequate
-
Upper arm – the outer back portion of the upper arm (this site may be more challenging to self-administer and has less subcutaneous tissue in some individuals)
Rotate injection sites within these areas to prevent lipohypertrophy (fatty lumps) or lipoatrophy (fat loss), which can affect absorption and increase the risk of inadvertent muscle injection.
Use correct injection technique to ensure subcutaneous delivery:
-
Pinch the skin gently between your thumb and forefinger to lift the subcutaneous tissue away from the underlying muscle. This creates a thicker target area of fatty tissue.
-
Insert the needle at a 90-degree angle to the skin surface when using a 4 mm needle (the standard length for most adults). For very lean individuals or areas with minimal subcutaneous fat, a 45-degree angle may be more appropriate.
-
Hold the pen in place for the full count as recommended in the Instructions for Use (typically 6 seconds) after pressing the injection button to ensure the full dose is delivered.
-
Release the pinch only after withdrawing the needle to prevent medication leakage.
Seek professional training and support. When initiating Saxenda, your prescriber, practice nurse, or diabetes specialist nurse should provide comprehensive injection technique training. Request a review appointment if you feel uncertain about your technique. Many NHS diabetes services offer ongoing support and can assess your injection sites and method.
Special considerations for lean individuals: If you have a lower BMI or limited subcutaneous fat, discuss injection site selection with your healthcare provider. They may recommend specific sites or techniques to minimise the risk of intramuscular injection. Some individuals may benefit from shorter needles or modified injection angles.
Never share your Saxenda pen or needles with others, even if the needle has been changed, as this poses a risk of infection transmission.
Frequently Asked Questions
Should I take another dose of Saxenda if I accidentally injected it into muscle?
No, do not take an additional dose. Continue with your next scheduled dose at the usual time, as taking extra medication could lead to overdose symptoms including severe nausea and hypoglycaemia.
What symptoms should I watch for after accidentally injecting Saxenda into muscle?
Monitor for increased injection site pain, gastrointestinal symptoms (nausea, vomiting, abdominal discomfort), and signs of hypoglycaemia if you have diabetes. Seek medical advice if symptoms are severe or persistent.
How can I prevent accidentally injecting Saxenda into muscle tissue?
Pinch the skin gently to lift subcutaneous tissue, inject at a 90-degree angle using appropriate sites (abdomen, thigh, upper arm), and rotate injection locations. Request injection technique training from your practice nurse if needed.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript